Medicare Part D doesn’t just give seniors access to prescription drugs - it’s built on a smart, numbers-driven system that pushes generic drugs to the front of the line. Why? Because generics save billions. Every year, over 87% of all Part D prescriptions are for generics. That’s not an accident. It’s the result of a carefully designed economic engine that rewards patients and plans for choosing cheaper, equally effective medications.
How Tiered Formularies Drive Generic Use
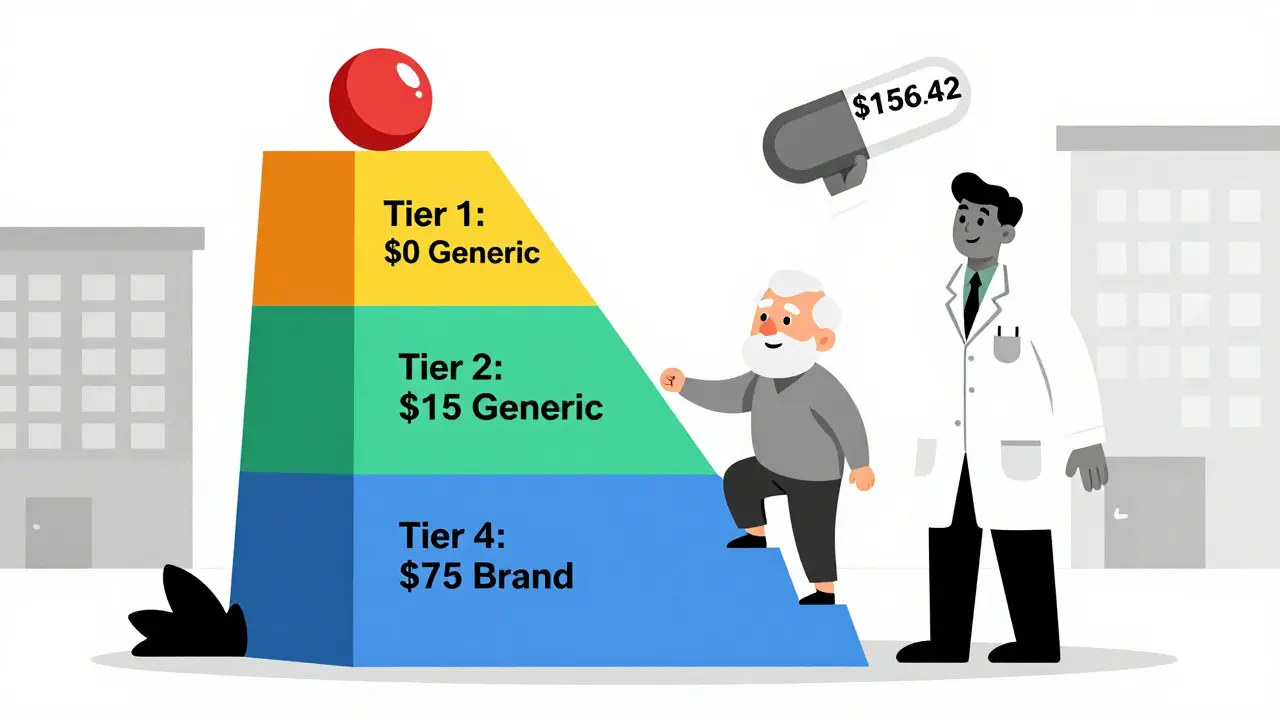
Every Medicare Part D plan uses a tiered formulary - basically a ladder of drug costs. The lowest rung? Preferred generics. These are the drugs that cost the least out-of-pocket for beneficiaries. In 2025, most plans charge $0 to $10 for a 30-day supply of a preferred generic at a preferred pharmacy. Compare that to a brand-name drug on Tier 3 or 4, which can easily cost $45 to $75 for the same amount. That’s a difference of over $1,500 a year per medication.
The system is designed to nudge people toward generics. If you’re paying 25% coinsurance during the initial coverage phase, it doesn’t matter if the drug is generic or brand-name - you pay the same percentage. But since the generic’s total price is so much lower, your actual out-of-pocket cost is tiny. A $10 generic means you pay $2.50. A $75 brand-name drug? You pay $18.75. The math pushes you toward the cheaper option.
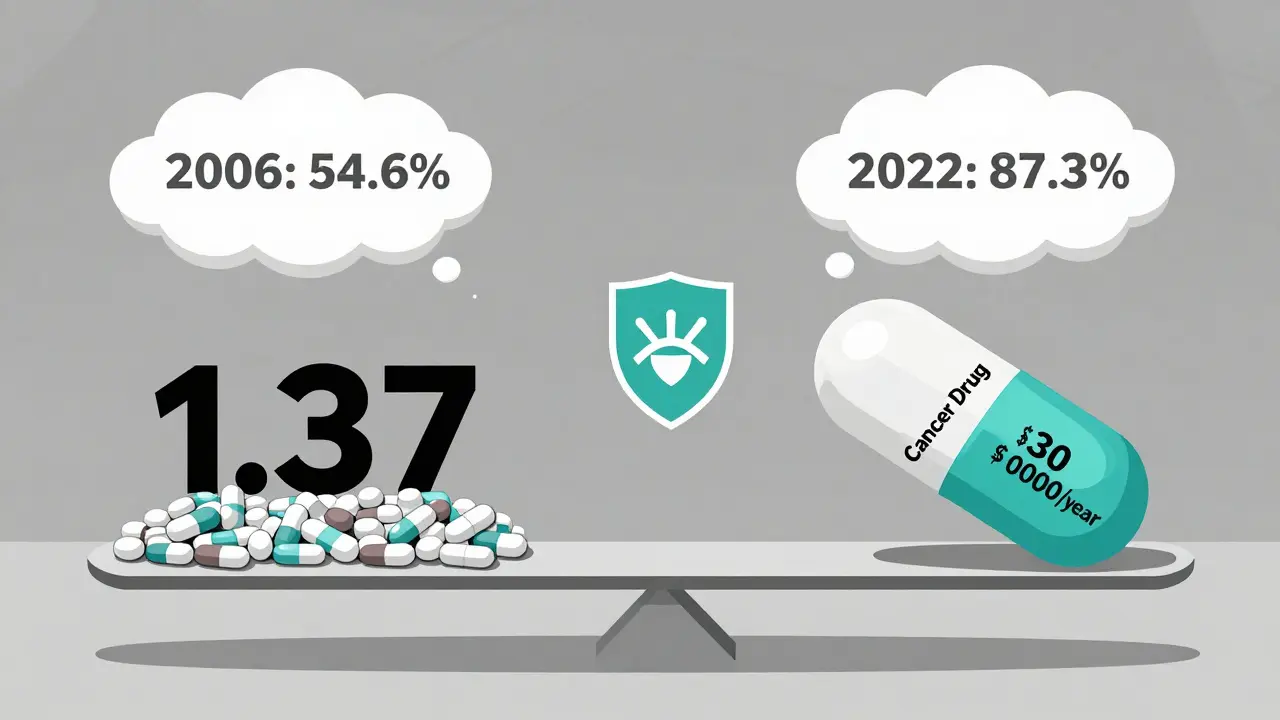
And it works. In 2022, 87.3% of all Part D prescriptions were for generics. That’s up from just 54.6% when the program started in 2006. The shift didn’t happen because patients suddenly preferred generics. It happened because the system made them the obvious choice.
The Hidden Math: What Generics Really Save
The numbers speak louder than opinions. According to the Medicare Payment Advisory Commission (MedPAC), Part D plans pay an average of $18.75 per generic prescription. For brand-name drugs? $156.42. That’s an 88% cost difference. Multiply that by over 2 billion prescriptions filled annually under Part D, and you get a savings of more than $1.37 trillion since 2006.
But here’s the twist: generics make up only 24.1% of total Part D spending. Brand-name drugs, which account for just 12.7% of prescriptions, soak up 75.9% of the money. Why? Because a few high-cost drugs - like those for cancer, multiple sclerosis, or rare diseases - can cost tens of thousands per year. Generics keep those spikes from blowing up the entire program.
The Inflation Reduction Act of 2022 added more pressure. Starting in 2025, beneficiaries won’t pay more than $2,000 out-of-pocket for all their drugs in a year. That cap changes everything. Once you hit it, you pay only $4.15 for a generic and $10.35 for a brand-name drug. Suddenly, the incentive to stick with generics becomes even stronger - especially for people on multiple medications.
Plan Differences Matter - A Lot
Not all Part D plans are created equal. A 2023 CMS report found that 63.2% of beneficiaries would pay more if they switched plans without checking the formulary. Why? Because plans can put the same generic drug in different tiers.
Take amlodipine, a common blood pressure medication. One plan might list it as a Tier 1 preferred generic with a $0 copay. Another might put it in Tier 2 with a $15 copay. Same drug. Same manufacturer. Same chemical. But different cost. That’s because plans negotiate deals with pharmacies and drugmakers. The plan that gets the best discount gets to offer the lower price.
Standalone Prescription Drug Plans (PDPs) tend to have slightly better generic coverage than Medicare Advantage plans with drug coverage (MA-PDs). In 2022, 92.4% of PDPs covered generic drugs, compared to 89.7% of MA-PDs. That’s not a huge gap, but for someone on three or four generics, it can mean hundreds of dollars a year.
What About the Protected Classes?
Some drug categories are off-limits to strict formulary controls. Part D must cover “substantially all” drugs in six protected classes: anti-cancer, anti-psychotic, anti-convulsant, anti-depressant, immunosuppressant, and anti-retroviral drugs. This means plans can’t block access to brand-name versions just because a generic exists.
But here’s the catch: even in these categories, generics are still the go-to. For example, generic versions of antidepressants like sertraline or antiretrovirals like tenofovir are widely used because they work just as well and cost a fraction of the price. The rule doesn’t mean brand-name drugs are preferred - it just means patients can’t be denied them if a generic doesn’t work for them.
Real Stories: Savings and Surprises
On Reddit’s r/Medicare community, users share real experiences. One person wrote: “My blood pressure med costs $0 for the generic (amlodipine) but $45/month for the brand (Norvasc). I switched and saved $540 a year.” Another said: “I got a brand-name drug that cost less than the generic because the manufacturer gave me a coupon - but Part D wouldn’t accept it.”
That second story highlights a flaw: manufacturer coupons don’t count toward your out-of-pocket spending. So if you use one, you’re not getting closer to the $2,000 cap. That’s why some people end up paying more in the long run.
Still, satisfaction is high. According to a 2023 survey, 78.4% of beneficiaries are happy with their plan’s generic coverage. Plans like SilverScript scored 4.6 out of 5 stars for their low-cost generic options. But complaints are common too - especially when plans change formularies mid-year. One in five beneficiary complaints in 2023 were about generics being moved to a higher tier, suddenly making them more expensive.

How to Use This System to Your Advantage
If you’re on Part D, here’s what you need to do:
- Use the Medicare Plan Finder during Open Enrollment (October 15 to December 7). Filter by your exact medications and see which plan has the lowest cost for each one.
- Look for plans with $0 copays on Tier 1 generics at your local pharmacy. In 2024, 42.3% of plans offered this.
- If your doctor prescribes a brand-name drug, ask if a generic is available - and if it’s covered at the same tier.
- If a generic causes side effects, request a coverage determination. CMS approved 78.4% of these requests in 2023.
- Don’t assume your plan won’t change. Review your formulary every year. Even small shifts can cost you hundreds.
People who use the Plan Finder tool save an average of $427 a year compared to those who don’t. That’s not a small amount - it’s enough to cover a month’s worth of groceries or a co-pay for a specialist visit.
What’s Next for Generics in Part D?
Starting January 1, 2025, drug manufacturers will be required to give extra discounts on both brand-name and generic drugs during the initial coverage and catastrophic phases. This is called the Manufacturer Discount Program. Experts predict it will push generic usage past 91% by 2027.
Also, CMS now requires every therapeutic category to have at least one generic drug available without prior authorization. That means no more delays for common medications like statins or metformin. This change alone could prevent thousands of people from skipping doses because of red tape.
The long-term future of Part D depends on generics. The Medicare Trustees Report says the program won’t stay solvent beyond 2093 unless generic use keeps growing at its current rate of 1.2 percentage points per year. Right now, it’s growing faster than that. That’s good news - for the program, for taxpayers, and for the millions of seniors who rely on it.
Why do generic drugs cost so much less than brand-name drugs?
Generic drugs cost less because they don’t need to cover the research, development, and marketing expenses that brand-name drugs do. Once a brand-name drug’s patent expires, other companies can make the same chemical without repeating expensive clinical trials. They just need to prove their version is bioequivalent - meaning it works the same way in the body. That cuts production costs dramatically. In Part D, generics cost plans an average of $18.75 per prescription, while brand-name drugs cost $156.42.
Can I be forced to take a generic drug on Medicare Part D?
No, you can’t be forced. Pharmacists may automatically substitute a generic if your prescription doesn’t say "dispense as written," but you can always ask for the brand-name version. If your doctor says the generic won’t work for you - maybe because of side effects or a medical condition - you can request a coverage determination. In 2023, 78.4% of these requests were approved by CMS.
Why does my generic drug cost more this year than last year?
It’s likely your plan moved the drug to a higher tier. Plans change their formularies every year, sometimes shifting generics from Tier 1 to Tier 2 or 3. That means your copay jumps from $0 to $15 or more. That’s why it’s critical to review your plan every year during Open Enrollment. You might find a different plan that covers your meds at the same low cost.
Do all Medicare Part D plans cover the same generics?
No. Each plan creates its own formulary, so coverage varies. One plan might cover a generic version of your medication with a $0 copay, while another might not cover it at all or put it in a high tier. The law requires plans to include at least two drugs in each of 148 therapeutic categories, but they don’t have to cover every generic in those categories. That’s why comparing plans using the Medicare Plan Finder is essential.
How does the $2,000 out-of-pocket cap in 2025 affect generic use?
The $2,000 cap makes generics even more valuable. Once you hit that limit, you pay only $4.15 for a generic and $10.35 for a brand-name drug. That means if you’re on multiple medications, especially expensive ones, sticking with generics helps you reach the cap faster - and then you pay almost nothing for the rest of the year. It’s a powerful incentive to choose generics, especially for people with chronic conditions.