Many people think asthma and COPD are the same thing - both make you wheeze and struggle to breathe. But they’re not. They’re two different diseases with different causes, different patterns, and very different treatments. Getting the diagnosis right matters because the wrong treatment can make things worse. If you’ve been told you have one but aren’t improving, it might be the other.
What’s Really Happening in Your Lungs?
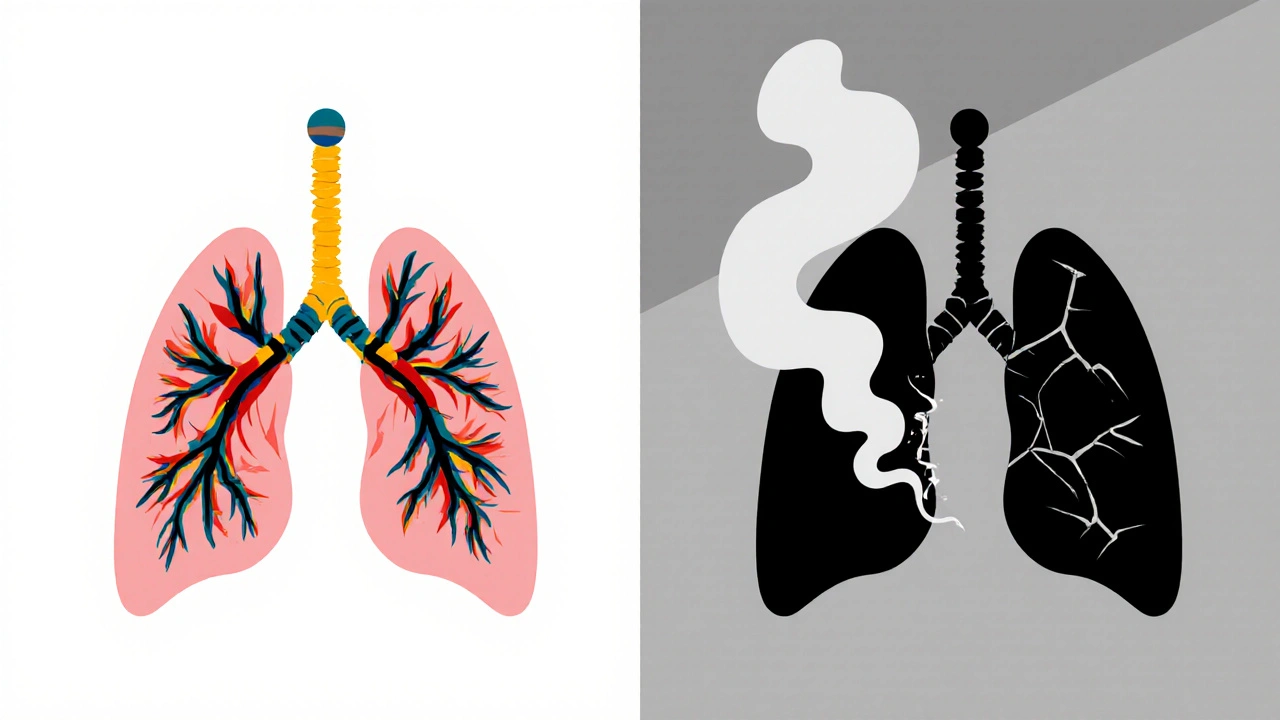
Asthma is an inflammatory condition where your airways react strongly to triggers like pollen, cold air, or exercise. The muscles around your airways tighten, swelling and mucus build up - and suddenly, breathing feels like trying to suck air through a straw. The good news? That narrowing usually reverses. Between attacks, many people feel completely normal.
COPD is different. It’s not a reaction - it’s damage. Years of smoking or long-term exposure to irritants like smoke or pollution destroy the air sacs in your lungs (emphysema) and inflame the airways (chronic bronchitis). The damage doesn’t heal. Your lungs lose elasticity, and air gets trapped. Even when you’re not coughing or wheezing, your lungs are working harder than they should.
Symptoms: When It’s Asthma vs. When It’s COPD
Both cause shortness of breath, coughing, and wheezing. But the timing and nature tell the story.
- Asthma: Symptoms come in waves. You might feel fine for weeks, then wake up at 3 a.m. with chest tightness and wheezing. Coughing is often dry. Nighttime symptoms are common. Triggers are clear - you know what sets it off.
- COPD: Symptoms are constant. You’ve had a morning cough with phlegm for years. Walking up the stairs leaves you winded. You’re not just wheezing - you’re gasping, even at rest. Cyanosis - a bluish tint around your lips or fingernails - shows up in advanced cases because your body isn’t getting enough oxygen.
One key clue: 73% of asthma patients have a dry cough, while 87% of COPD patients produce thick mucus daily. If you’ve been spitting up phlegm for years, it’s not likely just asthma.
Who Gets It and When?
Asthma often starts in childhood. Half of all cases are diagnosed before age 10. It’s common in kids with allergies - think eczema or hay fever. Genetics play a big role. If your parents have asthma, you’re more likely to get it.
COPD almost always shows up after age 40. Nine out of ten cases are linked to smoking. Even if you quit decades ago, the damage lingers. It’s rare to be diagnosed under 40 unless you’ve had heavy exposure to smoke, dust, or chemicals.
There’s one twist: 15-25% of people with obstructive lung disease have both. That’s called Asthma-COPD Overlap Syndrome (ACOS). These patients often have a history of childhood asthma, then started smoking later. Their symptoms are worse than either condition alone, and they end up in the ER more often.
How Doctors Tell Them Apart
It’s not just about symptoms. Doctors use tests to see what’s really going on.
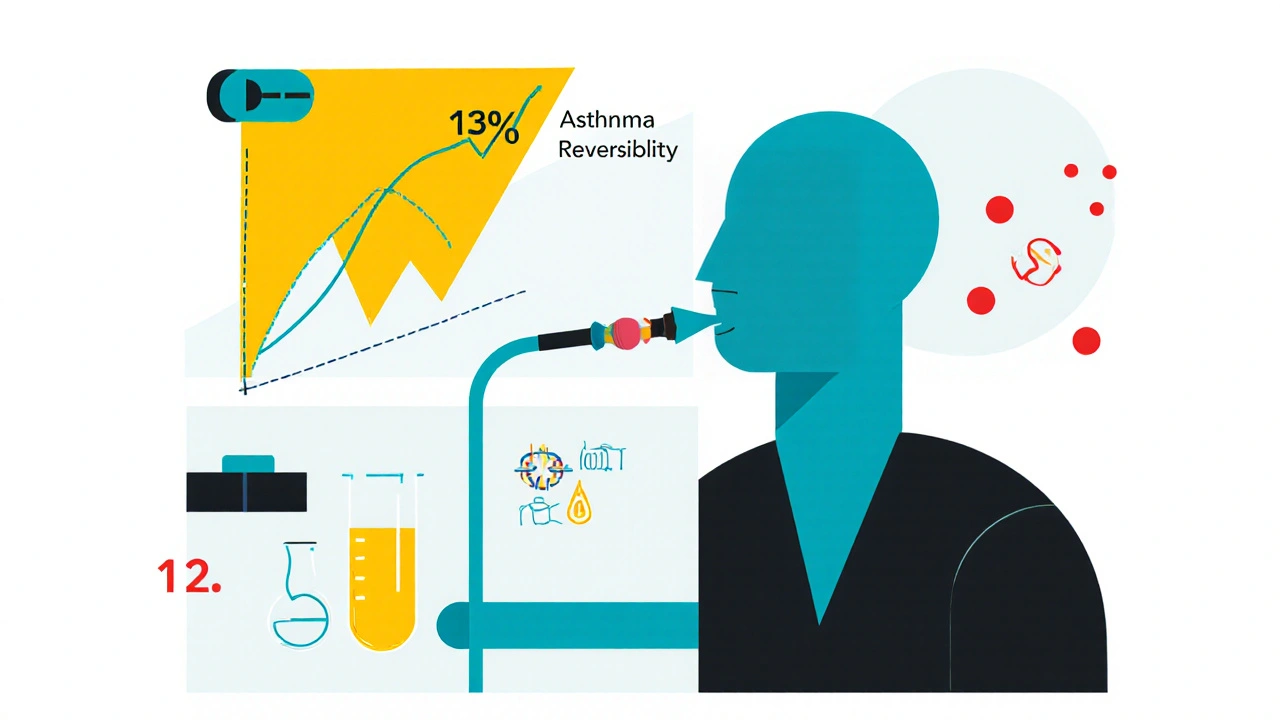
The gold standard is spirometry - a simple breathing test. You blow hard into a tube. The machine measures how much air you can force out in one second (FEV1). Then you inhale a bronchodilator (like albuterol) and try again.
- Asthma: After the inhaler, your FEV1 improves by 12% or more. That’s reversibility. About 95% of asthma patients show this.
- COPD: Improvement is usually less than 12%. The airflow blockage is permanent. Only about 15% of COPD patients show meaningful reversibility.
Another tool: fractional exhaled nitric oxide (FeNO). This test measures inflammation in your airways. Asthma patients often have high levels - above 50 ppb - because their inflammation is driven by eosinophils. COPD patients usually have levels below 25 ppb. Blood tests for eosinophils help too: counts above 300 cells/μL suggest asthma or ACOS; below 100 points to COPD.
High-resolution CT scans show the structural damage. 75% of COPD patients have visible emphysema - holes in the lung tissue. Only 5% of asthma patients show this.
Treatment: One Size Does Not Fit Both
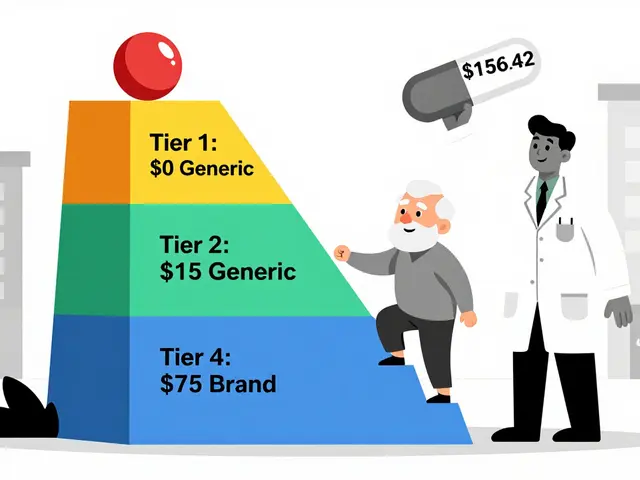
Asthma treatment is about controlling inflammation and preventing attacks. The first step is usually a rescue inhaler - albuterol - for quick relief. If symptoms happen more than twice a week, you’ll move to daily inhaled corticosteroids (ICS). For severe cases with high eosinophils, biologics like mepolizumab or omalizumab target specific immune pathways. 89% of asthma patients achieve good control with the right plan.
COPD treatment is about opening airways and slowing decline. Bronchodilators - long-acting ones (LABAs and LAMAs) - are the foundation. Steroids? Only if you’re having frequent flare-ups. You won’t get biologics. You won’t reverse the damage. But you can slow it.
Pulmonary rehab helps both, but differently. COPD patients gain real functional improvement - 54 meters farther on a 6-minute walk test after rehab. Asthma patients? They barely move the needle - only 12 meters - because their baseline function is already good between attacks.
Prognosis: What to Expect Long-Term
Asthma has a strong outlook. 92% of people with moderate asthma survive at least 10 years. Deaths are rare now - about 3,500 per year in the U.S. - thanks to better medications and awareness.
COPD is more serious. It’s the fourth leading cause of death in the U.S., killing 152,000 people a year. Even with treatment, only 78% of moderate COPD patients survive 10 years. The disease keeps progressing. Hospitalizations for flare-ups happen 7 times more often than in asthma.
Smoking changes everything. If you have COPD and quit, your decline slows by 50%. If you have asthma and smoke? You’re more likely to develop COPD later. Smoking doesn’t cause asthma - but it makes it worse and increases the risk of permanent lung damage.
What If You’re Still Not Sure?
One in three people over 40 with breathing problems get the wrong diagnosis. That’s why testing matters. If you’ve been on asthma meds for years and still feel tired, cough constantly, or get winded easily - ask for a full lung evaluation. Check your FEV1 reversibility. Get an FeNO test. Ask about eosinophil counts.
And if you’re over 40, have a long smoking history, and now have chronic cough and shortness of breath - don’t assume it’s just “smoker’s cough.” That could be COPD. Early diagnosis means you can start treatments that slow the damage.
Bottom Line
Asthma and COPD look similar on the surface - but they’re not the same disease. Asthma is about reversible inflammation. COPD is about irreversible damage. Treatment for one won’t work for the other. And if you have both - ACOS - you need a tailored plan.
Don’t guess. Get tested. Know your numbers. Your lungs are working harder than you think - and the right treatment can change everything.
Can asthma turn into COPD?
Not directly - but long-term uncontrolled asthma, especially in smokers, can lead to permanent airway changes that look like COPD. About 15-20% of people with asthma for over 20 years develop fixed airflow obstruction. This is called asthma-COPD overlap, not asthma turning into COPD. The damage comes from inflammation and smoking, not from asthma itself.
Is COPD only caused by smoking?
Mostly, yes. About 90% of COPD cases are linked to cigarette smoking. But non-smokers can get it too - from long-term exposure to air pollution, chemical fumes, dust, or secondhand smoke. In some parts of the world, burning biomass for cooking is a major cause. Genetics also play a small role - a rare condition called alpha-1 antitrypsin deficiency can cause COPD even in non-smokers.
Can I use my asthma inhaler if I have COPD?
Short-acting bronchodilators like albuterol can help relieve sudden symptoms in COPD, but they’re not the main treatment. COPD needs long-acting inhalers (LABAs, LAMAs) to keep airways open all day. Steroid inhalers (ICS) are only added if you have frequent flare-ups. Using an asthma inhaler alone won’t slow COPD progression - and relying on it too much can delay the right treatment.
Why do some people with asthma need biologics?
Biologics target specific parts of the immune system that drive severe asthma. They’re for people with high eosinophil levels, frequent attacks, and poor control despite using high-dose steroids. These drugs - like mepolizumab or dupilumab - reduce inflammation at the source. They’re not for COPD because COPD inflammation is caused by different cells and doesn’t respond to these targeted therapies.
How do I know if I have asthma-COPD overlap (ACOS)?
If you have a history of asthma since childhood or young adulthood, then started smoking or developed persistent breathing problems after 40, you might have ACOS. Signs include frequent flare-ups, needing multiple inhalers, and having both reversible airflow limitation (like asthma) and fixed obstruction (like COPD). Blood tests showing high eosinophils and low reversibility on spirometry help confirm it. A pulmonologist can run the right tests to tell.



![Buy Generic Lexapro (Escitalopram) Online Cheap-Safe UK Options, Prices, and Checks [2025]](/uploads/2025/09/thumbnail-buy-generic-lexapro-escitalopram-online-cheap-safe-uk-options-prices-and-checks.webp)
Dana Oralkhan
November 20, 2025 AT 22:06I’ve been living with asthma since I was 6, and this post hit home. I used to think my constant fatigue was just ‘being tired’-turns out it was uncontrolled inflammation. Got my FeNO test last year and learned I’m eosinophil-high. Started on a biologic, and now I can hike without gasping. If you’re still struggling despite meds? Ask for the test. You’re not overreacting-you’re just not being heard yet.
Also, shoutout to anyone who’s had to explain to their doctor that ‘it’s not just allergies’-you’re not crazy. This stuff matters.
Ron and Gill Day
November 22, 2025 AT 10:16Ugh. Another ‘asthma vs COPD’ infodump. Like anyone reading this doesn’t already know the basics. And why are we still using spirometry like it’s 1998? We’ve got AI-driven lung imaging now. This is basic med school stuff-why is this even a post? Lazy content farming.
Alyssa Torres
November 22, 2025 AT 23:04OMG I CRIED READING THIS. 😭
My mom had COPD. She smoked for 40 years, quit at 62, but by then it was too late. She’d sit on the porch every morning coughing up that thick mucus-no one ever told us it wasn’t just ‘smoker’s cough.’ I didn’t know the difference between asthma and COPD until she was in the hospital for the 4th time. This post? It’s the education we should’ve gotten in high school.
To anyone with a parent or grandparent who’s always ‘out of breath’-don’t ignore it. Get the test. Don’t wait until they’re on oxygen.
I’m sharing this with my entire family. Thank you.
Summer Joy
November 24, 2025 AT 03:28Okay but like… why are we still pretending asthma and COPD are separate? 🤡
It’s all just ‘lungs being trash’ and Big Pharma sells different inhalers to different labels. I’ve been on 7 different meds in 5 years and still wheeze. They just keep slapping new names on the same broken machine.
Also-biologics cost $30K a year. You think I’m gonna get that? 😂
Also also-did you know 80% of ‘COPD’ patients were misdiagnosed as asthma first? The system is rigged. 🧠💥
Aruna Urban Planner
November 25, 2025 AT 12:16From a public health perspective, the diagnostic delay in low-resource settings remains a critical gap. Spirometry is underutilized in rural India due to infrastructure constraints, leading to misclassification. The biomarkers referenced-FeNO, eosinophil counts-are not routinely available outside tertiary care centers. Without scalable, low-cost diagnostics, the distinction between asthma and COPD remains theoretical for the majority. Policy-level intervention is needed to integrate point-of-care pulmonary diagnostics into primary care pathways.
Also, ACOS prevalence in South Asia is underreported due to overlapping risk profiles (indoor air pollution + childhood asthma). This requires region-specific epidemiological frameworks.
Nicole Ziegler
November 27, 2025 AT 01:04Bharat Alasandi
November 27, 2025 AT 18:38Kristi Bennardo
November 28, 2025 AT 23:29This article is dangerously oversimplified. The assumption that FEV1 reversibility is a definitive diagnostic criterion ignores the heterogeneity of obstructive lung disease. Many COPD patients exhibit partial reversibility, and some asthmatics develop fixed obstruction over time. The arbitrary cutoffs of 12% and 50 ppb lack robust clinical validation in real-world populations. This kind of reductive content fuels diagnostic nihilism and delays appropriate care.
Additionally, the assertion that ‘biologics are not for COPD’ is outdated. Emerging trials show efficacy in eosinophilic COPD phenotypes. This is not 2010 anymore.
Shiv Karan Singh
November 29, 2025 AT 19:42Also, ‘biologics’? That’s just fancy word for ‘expensive placebo’. I’ve seen people spend $100K and still end up on oxygen. Wake up people.
Ravi boy
December 1, 2025 AT 18:34Matthew Karrs
December 3, 2025 AT 02:43Did you know the EPA and WHO data on air pollution is manipulated to downplay COPD rates? The real cause of ‘COPD’ is government-approved particulate emissions from power plants and diesel trucks. Smoking is a scapegoat. Look at the cities with zero smokers but high COPD rates-LA, Beijing, Delhi. It’s not the cigarettes. It’s the air.
And why do they always say ‘90% of COPD is from smoking’? Because if you admit it’s environmental, they’d have to sue the corporations. But that’s too expensive. So they blame the victim.
Also-why are biologics only for asthma? Because they’re too profitable to test on ‘smokers’.
Dana Oralkhan
December 3, 2025 AT 08:34Thank you for saying this. I had a pulmonologist tell me I was ‘too young for COPD’ when I was 32 and had a 20-pack-year history. I pushed back, got the CT scan-it showed early emphysema. I was diagnosed with ACOS. That’s when I realized: doctors don’t always know. You have to advocate.
And yes-air pollution matters. I live in LA. My asthma flares worse on bad air days than pollen. We need better data on environmental triggers. It’s not just about smoking.