When treating osteoarthritis, Cartidin is the brand name for diacerein, a disease‑modifying drug that targets cartilage breakdown and inflammation. Unlike classic painkillers, diacerein tries to slow the damage that leads to joint pain. Patients often wonder how it stacks up against over‑the‑counter pain relievers, supplements, and injectable therapies. Below you’ll find a side‑by‑side look that helps you decide if Cartidin belongs in your OA toolkit.
Key Takeaways
- Cartidin (diacerein) works by inhibiting inflammatory cytokines and protecting cartilage, while most alternatives focus on symptom relief.
- Typical dose is 50mg twice daily; it takes 4-6 weeks to feel benefits.
- Common side effects are mild diarrhea and liver‑enzyme changes; serious adverse events are rare.
- NSAIDs (ibuprofen, naproxen) act fast but carry GI, cardiovascular, and kidney risks with long‑term use.
- Supplements (glucosamine, chondroitin) have mixed evidence; they are safe but may offer modest symptom aid.
- Injectables (hyaluronic acid, corticosteroids) provide short‑term pain relief and can be combined with oral options.
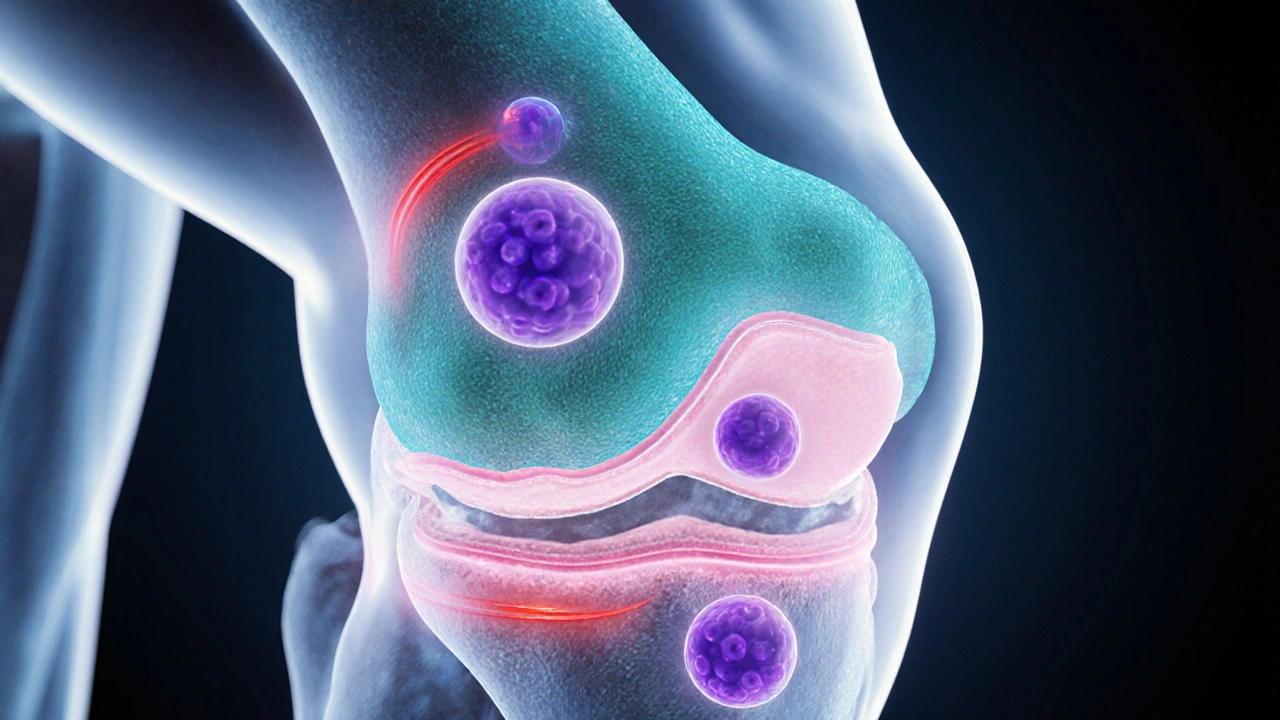
How Cartidin (Diacerein) Works
Diacerein belongs to a class called disease‑modifying osteoarthritis drugs (DMOADs). It blocks the production of interleukin‑1β, a molecule that drives cartilage degradation. By reducing this inflammatory cascade, diacerein helps preserve the extracellular matrix of the joint. The drug is taken orally, usually 50mg two times a day, and noticeable symptom improvement often appears after a month of consistent use. Because it targets the disease process rather than just pain, it’s sometimes positioned as a “slow‑acting” option.
Major Alternatives on the Market
Below are the most common alternatives patients consider, each with its own mechanism and risk profile.
- Ibuprofen is an NSAID that inhibits cyclooxygenase (COX‑1/COX‑2) enzymes, lowering prostaglandin‑driven inflammation.
- Naproxen works similarly to ibuprofen but has a longer half‑life, allowing twice‑daily dosing.
- Glucosamine is a naturally occurring amino‑sugar that serves as a building block for cartilage, often marketed as a joint‑support supplement.
- Chondroitin is a sulfated glycosaminoglycan that helps retain water in cartilage, commonly paired with glucosamine.
- Hyaluronic Acid Injection provides visco‑elastic lubrication to the joint space, improving shock absorption.
- Corticosteroid Injection delivers a potent anti‑inflammatory steroid directly into the joint, offering rapid pain relief.
- Physical Therapy combines targeted exercises, manual therapy, and education to improve joint stability and muscle strength.
Comparison Table: Cartidin vs Common Alternatives
| Attribute | Cartidin (Diacerein) | Ibuprofen / Naproxen (NSAIDs) | Glucosamine & Chondroitin | Hyaluronic Acid Injection | Corticosteroid Injection | Physical Therapy |
|---|---|---|---|---|---|---|
| Mechanism | Inhibits IL‑1β, protects cartilage | COX inhibition, reduces prostaglandins | Provides cartilage precursors | Restores joint synovial fluid viscosity | Suppresses local inflammation | Improves muscle support, joint biomechanics |
| Typical Dose | 50mg twice daily | 200‑400mg every 4‑6h (ibuprofen) or 250‑500mg twice daily (naproxen) | 1500mg glucosamine + 1200mg chondroitin daily | Single 20‑40mg injection, repeat as needed | 5‑10mg corticosteroid per injection | 2‑3 sessions per week, duration 6‑12weeks |
| Onset of Relief | 4‑6weeks | 30‑60minutes | 4‑12weeks (if any) | 1‑2weeks | Immediate to 24hours | 2‑4weeks |
| Common Side Effects | Diarrhea, mild liver‑enzyme rise | Stomach upset, heartburn, increased CV risk | Generally well‑tolerated, occasional GI upset | Injection site pain, rare infection | Joint swelling, cartilage thinning with repeated use | Muscle soreness, temporary increase in pain |
| Prescription Status | Prescription | OTC (low dose) / Prescription (high dose) | OTC | Prescription | Prescription | Referral required |
| Cost (US$ per month) | ~$120‑$180 | ~$10‑$30 | ~$30‑$50 | ~$250‑$350 per injection | ~$120‑$200 per injection | ~$300‑$600 for full program |
When Cartidin Makes Sense
If you’ve been on NSAIDs for years and are worried about stomach ulcers or cardiovascular strain, Cartidin offers a slower but safer way to address the root cause of cartilage loss. It’s also a good option for people who need continuous pain control without the jittery feeling that some NSAIDs cause.
- Diagnosed moderate OA in knee or hip with persistent pain despite OTC NSAIDs.
- History of GI bleeding or high blood‑pressure that makes long‑term NSAID use risky.
- Desire for a disease‑modifying approach rather than just symptom masking.
Because the drug can affect liver enzymes, regular blood‑work every 2-3months is recommended. If you have pre‑existing liver disease, discuss alternatives with your physician.

Scenarios Where Alternatives Might Edge Out Cartidin
Cartidin isn’t a magic bullet. Its delayed onset and prescription requirement mean it’s not ideal for someone needing rapid pain relief before a marathon or a short‑term flare‑up. In those cases, consider these options:
- Ibuprofen or naproxen for fast, short‑term relief-but limit use to a few weeks if you have heart or kidney concerns.
- Glucosamine/chondroitin if you prefer a gentle, OTC supplement with minimal side effects.
- Hyaluronic acid injections for people who want improved joint lubrication without daily pills.
- Corticosteroid shots for acute inflammation spikes, keeping frequency under three per year to avoid joint damage.
- Physical therapy as a cornerstone for long‑term joint health, especially after surgery or to delay the need for medication altogether.
Practical Tips for Getting the Most Out of Your Choice
- Start with a clear goal: rapid pain relief vs. disease modification.
- Check contraindications: liver disease for Cartidin, stomach ulcer risk for NSAIDs, allergy to shellfish for glucosamine (derived from crustacean shells).
- Discuss dosing schedules with your doctor; some patients split Cartidin doses to reduce GI upset.
- Combine modalities wisely: a low‑dose NSAID can bridge the gap while Cartidin builds effect.
- Monitor outcomes: use a pain diary and joint function score (e.g., WOMAC) every month.
- Re‑evaluate every 6months; if no improvement, consider switching or adding an injectable.
Common Questions About Cartidin and Its Alternatives
Frequently Asked Questions
How long does it take to feel relief with Cartidin?
Most patients notice a gradual reduction in pain after 4‑6weeks of consistent dosing. Full disease‑modifying effects may take 3‑6months.
Can I take Cartidin together with an NSAID?
Yes, many doctors prescribe a low‑dose ibuprofen to cover the first few weeks while Cartidin builds its effect. Always follow your prescriber’s guidance to avoid stomach irritation.
What monitoring is required for Cartidin?
Baseline liver function tests are recommended, followed by repeat tests every 2-3months. If enzymes rise more than three times the upper limit, stop the drug and consult your doctor.
Are glucosamine and chondroitin effective?
Research shows mixed results. Some patients report modest pain relief, especially when both are taken together, but the effect is generally milder than prescription options.
When should I consider an injection instead of oral medication?
If oral drugs cause side effects or don’t give enough relief, an intra‑articular injection (hyaluronic acid or corticosteroid) can target the joint directly. Discuss timing and frequency with your orthopaedic specialist.
Bottom Line: Pick the Tool That Matches Your Needs
Cartidin sits in a niche of slower‑acting, cartilage‑protecting drugs. It shines for people who can tolerate a few weeks of waiting and want to address the disease itself rather than just mask pain. If immediate relief is your priority, NSAIDs or a short course of corticosteroid injection will likely serve you better. Supplements offer a safe, low‑cost adjunct, and physical therapy remains the foundation for long‑term joint health. Use the comparison table, weigh the side‑effect profile, and talk to a healthcare professional to build a plan that fits your lifestyle and medical history.






Chidi Anslem
October 3, 2025 AT 16:04Cartidin’s approach of protecting cartilage rather than just dulling pain is a refreshing shift in OA management. It respects the body’s natural repair mechanisms while still offering measurable relief after a few weeks. For patients wary of the gastrointestinal toll of NSAIDs, this slower‑acting option provides a viable middle ground. Of course, the delayed onset means adherence is key; missing doses can reset the modest gains you’ve earned.
Holly Hayes
October 8, 2025 AT 07:10if u keep popping ibuprofen u are basically inviting stomach ulcers lol
Penn Shade
October 12, 2025 AT 22:17Based on the pharmacodynamics, diacerein directly inhibits IL‑1β, which differentiates it from NSAIDs that merely block COX enzymes. This mechanistic distinction translates into a potential disease‑modifying effect rather than transient analgesia.
Jennifer Banash
October 17, 2025 AT 13:24Indeed, the narrative of Cartidin unfolds as a saga of cautious optimism, wherein the protagonist-our joint cartilage-receives a protective mantle against relentless inflammatory onslaughts. Yet, the plot thickens, for the drug’s latency in delivering symptomatic respite may test the patience of even the most steadfast adherents.
Stephen Gachie
October 22, 2025 AT 04:30one might contemplate the epistemic humility required when embracing a therapy that promises structural preservation yet demands temporal forbearance. the mind, in its quest for immediacy, often undervalues such longitudinal virtues.
Sara Spitzer
October 26, 2025 AT 18:37Well the evidence on glucosamine is as shaky as a cheap chair and the side‑effects of NSAIDs are not something to dismiss. You can’t just ignore the GI risk when you’re on ibuprofen daily.
Jennifer Pavlik
October 31, 2025 AT 09:44Choosing the right OA treatment starts with understanding your personal goals. If you want to slow joint damage, Cartidin fits that aim. It works on the root cause by stopping inflammatory signals. It does not give instant pain relief like ibuprofen does. That means you have to be patient for a few weeks. During that time keep a pain diary to see any changes. Write down your activity level and how your knee feels each day. Share this diary with your doctor at each visit. If you notice steady improvement, you are on the right track. If nothing changes after six weeks, discuss alternatives with your physician. Some people add a low‑dose NSAID to bridge the gap while Cartidin builds effect. Remember to get liver function tests every few months because of possible enzyme changes. Drinking plenty of water can help with mild diarrhea. Pair the medication with regular physical therapy to strengthen surrounding muscles. A balanced approach often yields the best long‑term results. Stay committed and you may keep your joints healthier for years to come.
Jacob Miller
November 5, 2025 AT 00:50Sure, the science sounds solid, but most patients don’t have the luxury to wait six weeks for a modest benefit.
Anshul Gandhi
November 9, 2025 AT 15:57Don’t be fooled by the pharma narrative; the delayed onset is a deliberate design to keep you dependent on repeat prescriptions while they line their pockets.
Emily Wang
November 14, 2025 AT 07:04Rise above that manipulation and take charge of your joint health; consistency with Cartidin, combined with targeted exercises, can empower you to reclaim mobility.
Hayden Kuhtze
November 18, 2025 AT 22:10Ah, the ever‑so‑tragic plight of the layperson confronting the “shaky chair” of glucosamine research-how utterly unexpected.
Craig Hoffman
November 23, 2025 AT 13:17yeah right…
Terry Duke
November 28, 2025 AT 04:24What a great point! Keeping the cartilage safe is essential, and with patience, you’ll likely see those small gains turn into meaningful relief, so stay the course and track your progress diligently!