Medication Trade-Off Calculator
Understand Your Options
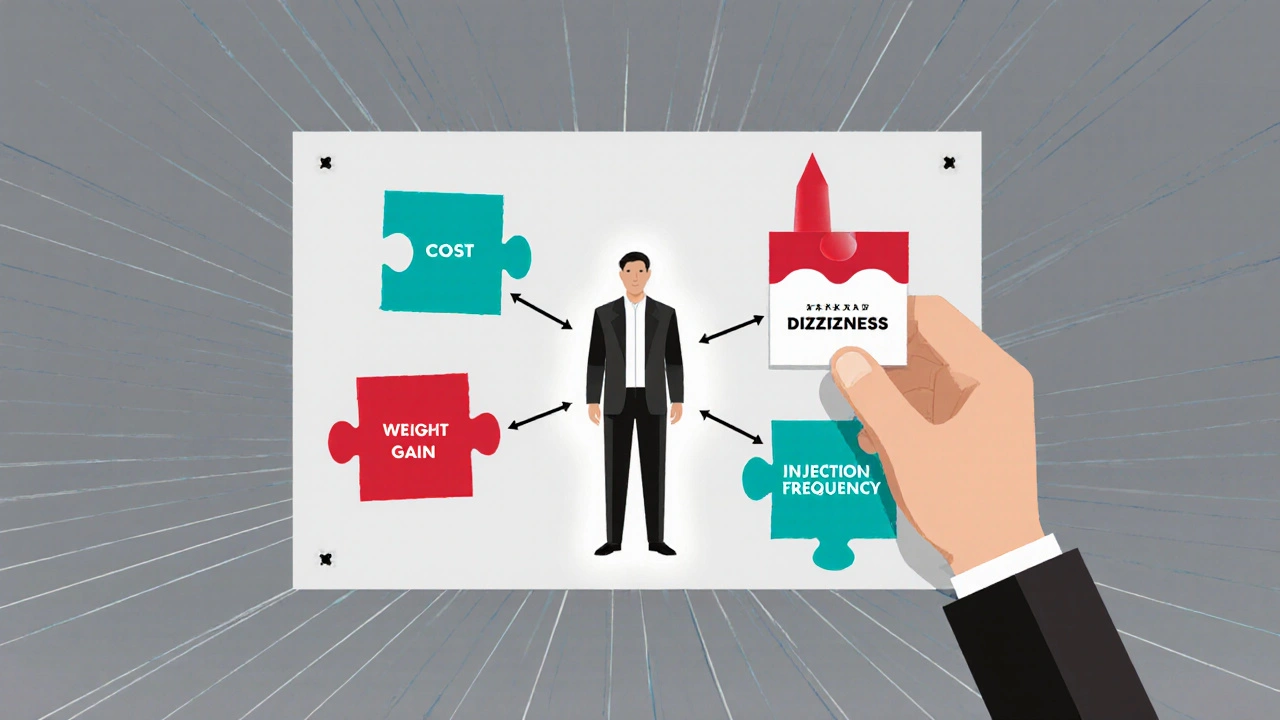
Compare medications by entering side effect probabilities. See how your priorities impact the best choice for you.
Medication A
Medication B
What Matters Most To You?
Choose the side effect that matters most to your daily life. This will determine which medication is best for you.
Why Switching Medications Feels So Overwhelming
Imagine your doctor says it’s time to switch your blood pressure pill. You’ve been on it for two years. It works. But now there’s a new option-maybe cheaper, maybe fewer side effects. But what if the new one causes dizziness? Or weight gain? Or worse, something you can’t even name? You leave the office feeling confused, not empowered. You’re not alone. Medication switching is one of the most stressful moments in chronic care, and too often, patients are left to guess what’s best.
Here’s the truth: most people don’t switch medications because their doctor told them to. They switch because they’re tired of side effects, scared of long-term risks, or just plain worn out by the daily routine. A 2022 study in JAMA Internal Medicine found that between 25% and 50% of patients stop their meds within the first year-not because they didn’t work, but because they didn’t understand the trade-offs. That’s not noncompliance. That’s a system failure.
What Are Decision Aids, Really?
A decision aid isn’t just a pamphlet. It’s not a website with a list of pros and cons. It’s a tool designed to help you, the patient, figure out what matters most to you-not just what the data says. These tools walk you through the real numbers: Out of 100 people like you, how many will avoid a heart attack? How many will get a rash? How many will feel nauseous every morning?
They use simple visuals-like icon arrays showing 100 little people, some colored red for side effects, some green for benefits. You see it. You don’t just hear it. One veteran in a VA forum said, “Seeing 3 out of 100 people bleed on the new drug made me pause. I’d heard ‘low risk’ before. But seeing three little red dots? That stuck.”
These tools also ask you to rank what matters: Is taking one pill a day more important than avoiding weight gain? Is cost more urgent than avoiding drowsiness? You pick. The tool doesn’t push you toward one answer. It just shows you what each choice means, and then lets you decide.
How Decision Aids Beat Old-School Advice
Traditional doctor visits often go like this: “We’re switching you to Med B. It’s better.” No numbers. No visuals. No chance to say, “But I can’t handle dizziness-I drive for a living.”
Decision aids change that. A 2022 review of 18 studies showed patients who used these tools remembered 32% more about their options six months later. They also felt less conflicted-28% less stress about making the wrong choice. That’s huge. When you understand the trade-offs, you’re not just following orders. You’re making a choice you can live with.
Take diabetes meds. There are six or seven common options. Some cause weight loss. Some cause GI issues. Some cost $500 a month. Without a decision aid, patients often pick based on what their friend took-or what their doctor mentioned first. With a decision aid, they see side effect probabilities side-by-side: “Med A: 30% chance of weight gain. Med B: 15%. Med C: 5%, but you’ll need to inject it daily.” That’s not just info. That’s power.
Where Decision Aids Fall Short
They’re not magic. And they’re not for everyone.
First, they take time. A 2023 study found doctors needed 7 to 12 extra minutes per visit to use them well. In a busy clinic, that’s hard to squeeze in. Many doctors say they’d love to use them-but their schedule won’t allow it.
Second, they can overwhelm. Some patients look at a table with six columns of percentages and just shut down. One Mayo Clinic user said, “It felt like I was taking a math test. I just wanted a simple answer.” That’s why good tools let you go slow, revisit sections, and even pause to talk with your provider.
Third, they’re useless in emergencies. If you’re having a stroke and need to switch anticoagulants right now, no decision aid helps. And if someone has severe memory issues-like advanced dementia-these tools won’t work. The brain needs to process numbers and trade-offs. Not everyone can.
And here’s a quiet danger: some patients think the tool is telling them what to do. One patient told a researcher, “The app said Med B was ‘recommended.’ So I took it.” But the tool didn’t recommend. It showed options. That’s a big difference.
Real Stories: When Decision Aids Changed Outcomes
There’s a woman in Ohio who was on an antidepressant that made her feel like a zombie. Her doctor suggested switching. She didn’t want to. She’d tried three before. But then she used a decision aid that showed her the odds: “This new drug has a 12% chance of nausea, but only a 4% chance of weight gain.” She’d gained 30 pounds on her last med. That 4% mattered more than the nausea. She switched. Lost 15 pounds in six months. Said she felt like herself again.
Another man, 68, was on warfarin. He hated the blood tests. The decision aid showed him: “DOACs have 3 bleeding events per 100 people per year. Warfarin has 8.” He chose the DOAC. No more monthly trips to the lab. He said, “It wasn’t about being safer. It was about being free.”
But not all stories end well. One patient used a decision aid to switch from metformin to a newer drug. The tool showed a 5% chance of pancreatitis. He thought, “5% is low. I’m fine.” He didn’t realize 5% of 100 people is five people-and one of them could be him. He ended up in the ER. The tool didn’t fail. But he didn’t ask his doctor to explain what “5%” meant in his context. That’s the gap.
How to Use a Decision Aid the Right Way
If your doctor suggests one, here’s how to make it work:
- Ask for it ahead of time. Don’t wait until the appointment. Say: “Can I get the decision aid for this switch before we talk? I want to think about it.”
- Use it alone first. Don’t let your partner or kid answer for you. This is your body, your life.
- Write down what matters most. Is cost the biggest worry? Sleep? Energy? Write it down. Then see which option matches.
- Bring your notes to the appointment. Say: “I saw that Med X has a 20% chance of dizziness. I can’t work if I’m dizzy. Is that still the best option?”
- Ask: “What’s the worst that could happen?” Not just the side effect-but what happens if it does? Can you manage it? Do you need to go to the hospital?
Who’s Using These Tools Right Now?
They’re not just in fancy hospitals. The VA uses them for mental health meds, blood thinners, and diabetes drugs. Mayo Clinic has 15 decision aids online for free. The Ottawa Hospital’s library has 42, in 12 languages, and meets accessibility standards so people with vision or hearing loss can use them too.
Medicare Advantage plans now have to offer shared decision-making tools for high-cost drugs-so you’ll see more of them in 2025. But adoption is still uneven. In VA clinics, 68% of providers use them. In regular primary care? Only 29%. Why? No funding. No training. No time.
Still, the trend is clear: if you’re switching meds for a condition where multiple options exist-like depression, diabetes, or high blood pressure-you deserve better than a 30-second explanation.
What’s Next for Decision Aids?
AI is starting to personalize them. Intermountain Healthcare launched a tool in early 2024 that adjusts how it shows risks based on how you learn. If you’re a visual person, it shows icons. If you like numbers, it shows charts. If you’re in a hurry, it gives you the bottom line first.
The FDA is pushing for stricter rules too. In 2024, they proposed that all digital decision aids must be tested on real patients-including older adults, non-native English speakers, and people with low health literacy. No more “one-size-fits-all” tools.
But here’s the big question: will they last? Only 38% of hospitals have money set aside to update them. Medications change fast. A decision aid made in 2022 might be outdated by 2025. If they’re not kept current, they become dangerous.
Final Thought: You’re Not Just a Patient. You’re a Partner.
Switching meds shouldn’t feel like a gamble. You shouldn’t have to trust your doctor’s word alone. Decision aids don’t replace your doctor. They give you the tools to talk to them as an equal. You’re not just listening. You’re choosing.
Next time you’re asked to switch, ask: “Is there a decision aid for this?” If they say no, ask why. If they say yes, use it. Then ask again: “What does this mean for me?”
Because your health isn’t a statistic. It’s your life.
What exactly is a medication decision aid?
A medication decision aid is a structured tool-often digital-that helps patients understand the benefits, risks, and side effects of switching from one medication to another. It uses clear numbers, visuals like icon arrays, and interactive questions to help you match your personal values (like cost, dosing frequency, or fear of weight gain) with your treatment options. It doesn’t tell you what to do-it helps you decide for yourself.
Are decision aids only for serious conditions like diabetes or heart disease?
No. They’re used for any situation where there’s more than one valid option and the choice depends on personal priorities. That includes antidepressants, blood pressure meds, cholesterol drugs, and even pain relievers. The key is whether the options have different side effects, costs, or routines-not how serious the condition is.
Can I use a decision aid without my doctor’s approval?
Yes. Many are free and publicly available-from the VA, Mayo Clinic, or Ottawa Hospital. But they’re designed to be used with your doctor, not instead of them. Bring what you learn to your appointment. It helps your doctor understand your concerns and tailor advice better.
Do decision aids work for older adults or people with memory problems?
They’re less effective for people with severe cognitive impairment-like advanced dementia-because they require understanding probabilities and making trade-offs. But for most older adults with normal thinking skills, they work well. The best tools are designed with large fonts, simple language, and audio options to support accessibility.
Why don’t all doctors use decision aids?
Time and training. Most clinics are rushed. Adding a 10-minute tool to a 15-minute visit is hard. Also, many doctors weren’t trained in how to use them. They’re not magic buttons-they need practice. But adoption is growing, especially in VA hospitals and systems with funding for patient-centered care.
Are decision aids free to use?
Yes. The most trusted ones-from the VA, Mayo Clinic, and Ottawa Hospital-are free and open to the public. Some commercial tools exist, but they’re usually tied to insurance plans. Stick to the academic or government ones. They’re evidence-based, regularly updated, and don’t push specific brands.
How do I know if a decision aid is reliable?
Look for the source. Trusted ones come from major hospitals (Mayo, Ottawa, VA), universities, or government health agencies. They cite evidence from clinical trials and update regularly. Avoid tools from drug companies or websites that don’t list their sources. If it says “sponsored by Pfizer,” be cautious.
What if I still feel unsure after using a decision aid?
That’s normal. Decision aids don’t eliminate doubt-they help you understand it. If you’re still unsure, ask your doctor: “Can we wait a week and revisit this?” or “Can you help me weigh the risks again?” You don’t have to decide in one visit. Good decisions take time.







Dade Hughston
October 31, 2025 AT 21:48Jim Peddle
November 2, 2025 AT 16:45S Love
November 2, 2025 AT 19:36Pritesh Mehta
November 3, 2025 AT 22:51Billy Tiger
November 5, 2025 AT 06:03Katie Ring
November 6, 2025 AT 18:27Adarsha Foundation
November 7, 2025 AT 14:56Alex Sherman
November 9, 2025 AT 05:13Oliver Myers
November 11, 2025 AT 02:23