Every year, millions of people in the U.S. reach for an OTC painkiller, antacid, or allergy pill without thinking twice. But here’s the thing: not every symptom needs a pharmacy trip. And not every OTC pill is safer than a prescription. Knowing when to use OTC medications versus when to call your doctor can save you money, time, and even risk.
What Exactly Is an OTC Medication?
OTC medications are drugs you can buy without a doctor’s note. They’re on the shelf next to toothpaste and gum. Common examples include ibuprofen for headaches, loratadine for allergies, and omeprazole for heartburn. These aren’t weak drugs - they’re FDA-approved and tested for safety when used as directed.
But here’s what most people don’t realize: OTC doesn’t mean harmless. Taking too much acetaminophen can wreck your liver. Mixing naproxen with blood pressure meds can spike your risk of kidney damage. The FDA keeps a list of over 800 active ingredients approved for OTC use, and they’re in more than 100,000 products. That’s a lot of choices - and a lot of room for confusion.
When Prescription Medications Are Necessary
Prescription drugs are for conditions that need more than a quick fix. Think high blood pressure, diabetes, asthma, thyroid issues, or chronic migraines. These aren’t symptoms you can self-diagnose reliably. They require monitoring, lab tests, and adjustments over time.
For example, if you’re on a prescription beta-blocker for heart rhythm issues, switching to an OTC decongestant could raise your blood pressure dangerously. Or if you have frequent acid reflux that doesn’t improve with OTC omeprazole after two weeks, you might have GERD - and need a stronger dose or a different drug entirely. That’s where your doctor comes in.
Prescription drugs often have higher potency. Take hydrocortisone cream: OTC is 1%, prescription is 2.5%. That extra strength matters for stubborn eczema or poison ivy. Same with ranitidine - OTC is 75 mg, prescription can be 150 mg or 300 mg. Higher dose isn’t always better, but sometimes it’s the only way to get control.
OTC Medications That Work - When Used Right
For mild, short-term issues, OTC meds are perfect. Here’s the rule: if your symptoms started slowly, are mild, and you’ve had them before, OTC is fine.
- Headaches: Ibuprofen or acetaminophen works for tension headaches or occasional migraines - as long as they’re not happening more than 10 days a month. If you’re hitting the bottle every other day, you’re at risk for rebound headaches.
- Allergies: Cetirizine (Zyrtec) or fexofenadine (Allegra) start working in under an hour. They’re great for seasonal sneezing, itchy eyes, or runny nose. But if you’re wheezing or your throat swells, that’s not an allergy - that’s an emergency. Get help.
- Heartburn: OTC esomeprazole (Nexium) takes 1-2 days to build up in your system. If you expect instant relief like you got from a prescription version, you’ll be disappointed. Don’t give up after one dose.
- Cough and cold: Dextromethorphan for cough, pseudoephedrine for congestion - these help you sleep and function. But if your cough lasts more than 10 days or you’re coughing up green phlegm, it’s not a cold. It’s a bacterial infection. You need antibiotics - and those are prescription.
The Rx-to-OTC Switch: What’s Changed?
Over the last 15 years, more prescription drugs have moved to the OTC shelf. Why? Because safety data proved they’re safe for self-use. Fexofenadine (Allegra), adapalene (Differin for acne), and esomeprazole (Nexium) all started as prescriptions. Now you can grab them at the checkout.
This trend is accelerating. In April 2023, the FDA approved the first OTC epinephrine auto-injector - the same device used for anaphylaxis. Before, you needed a script. Now, anyone with a known severe allergy can buy it without a doctor’s visit. That’s a huge win for safety.
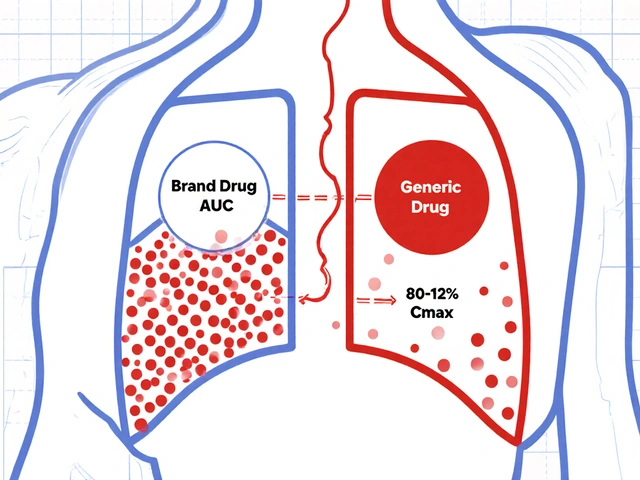
But don’t assume all switches are equal. Just because a drug is OTC doesn’t mean it’s right for everyone. The OTC version of a drug might have a lower dose, slower release, or different formulation than the prescription one. Always check the label.

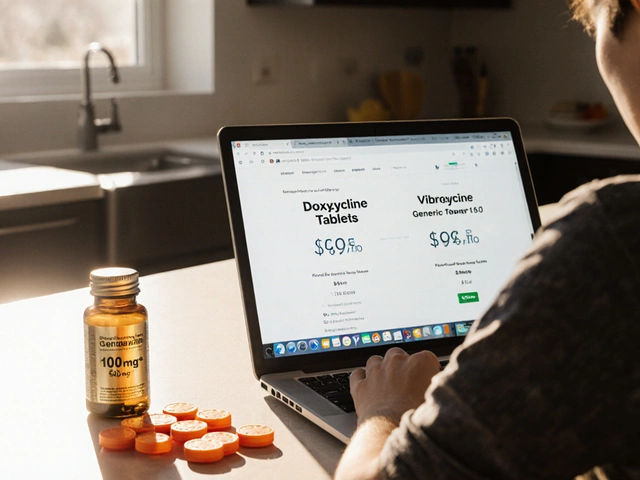
Cost Isn’t Always What You Think
Many assume OTC is cheaper. Sometimes it is. A 100-tablet bottle of store-brand ibuprofen 200 mg costs around $4. Brand-name Advil? $15. Big difference.
But here’s the twist: if you have insurance, your prescription might be cheaper. A 30-day supply of lisinopril for high blood pressure might cost $5 with insurance, while buying OTC supplements that claim to lower BP could cost $40 a month and do nothing. Medicare Part D often covers generics at low copays - sometimes lower than the OTC price.
And don’t forget: if you’re taking OTC meds daily for months and they’re not working, you’re wasting money. That $4 bottle of antacid every week adds up to $208 a year. If it’s masking something serious, you’re risking your health - and paying more in the long run.
When to Stop Self-Treating and Call a Doctor
OTC meds are tools, not solutions. Here’s when to stop using them and get help:
- Symptoms last more than 7-10 days without improvement
- Pain gets worse instead of better
- You have new symptoms - fever, rash, swelling, trouble breathing
- You’re taking more than the recommended dose
- You’re on other medications (even supplements)
- You’re over 65 or pregnant
For migraines, experts say OTC painkillers are fine for mild attacks under 10 days a month. But if you’re having them weekly, or they come with nausea, light sensitivity, or aura, you need a prescription triptan. OTC meds take longer to work - often too long for a severe attack.
Pharmacists Are Your Secret Weapon
You don’t need to guess. Every pharmacy has a licensed pharmacist on staff. They’re trained to help you pick the right OTC product, spot dangerous interactions, and tell you when you need a doctor.
Eighty-nine percent of community pharmacists say they counsel patients on OTC vs. prescription choices during routine visits. Ask them: “Is this safe to take with my other meds?” or “Should I be seeing a doctor for this?”
They’ll know if the OTC version of your old prescription has a different release time. They’ll warn you about alcohol interactions with NSAIDs. They’ll tell you if that “natural remedy” you bought online is useless - or dangerous.
What’s Coming Next?
The line between OTC and prescription is blurring. By 2030, experts predict 20-25 more drugs will switch from prescription to OTC - including birth control pills, asthma inhalers, and stronger anti-inflammatories.
That’s good news for access. But it also means you’ll need to be smarter. Just because it’s on the shelf doesn’t mean it’s right for you. The same active ingredient can have different effects based on dosage, timing, and your health history.
For example, a new OTC migraine treatment is being developed with a faster-acting form of sumatriptan. It’s not a replacement for the prescription version - it’s a tool for milder cases. Knowing the difference matters.
Final Rule: Listen to Your Body, Not the Label
OTC medications are powerful. They’ve helped millions manage everyday discomforts safely. But they’re not magic. They don’t fix root causes. They mask symptoms - sometimes for the better, sometimes dangerously.
Use them when your symptoms are mild, clear, and temporary. If you’re unsure, wait 24-48 hours. If it’s not better, or it’s getting worse, see a professional. Don’t wait until you’re in the ER because you thought a $4 pill would fix a $10,000 problem.
Medication isn’t about price. It’s about safety. And sometimes, the best choice isn’t what’s on the shelf - it’s what’s in your doctor’s prescription pad.
Can I take OTC painkillers every day?
No. Taking OTC painkillers like ibuprofen or naproxen daily for more than 10 days a month can lead to rebound headaches, stomach ulcers, or kidney damage. Acetaminophen daily can harm your liver, especially if you drink alcohol. If you need daily pain relief, talk to your doctor - you may have an underlying condition that needs treatment, not just masking.
Is OTC the same as prescription strength?
Not always. Some OTC versions have lower doses or slower-release formulas. For example, OTC omeprazole is 20 mg, while prescription can be 40 mg. OTC cetirizine is 10 mg, but prescription versions may include higher doses or combinations with decongestants. Always check the active ingredient and dosage on the label.
Can I switch from a prescription to OTC without asking my doctor?
Don’t. Even if the active ingredient is the same, the dosage, timing, or formulation may differ. Your doctor prescribed a specific version for your condition. Switching without advice could mean under-treating your issue or missing side effects. Always consult your provider before making the switch.
Are OTC medications safe for seniors?
Many OTC meds are risky for people over 65. NSAIDs like ibuprofen increase the risk of bleeding and kidney problems in older adults. Antihistamines like diphenhydramine (Benadryl) can cause confusion, dizziness, and falls. Always check with a pharmacist or doctor before giving OTC drugs to seniors - even “mild” ones.
Why do some OTC meds take days to work?
Some OTC drugs, like proton pump inhibitors (omeprazole, esomeprazole), need time to build up in your system to reduce acid production. They’re not fast-acting like antacids. If you take them for heartburn and don’t feel relief after 2-3 days, it’s not working - and you should see a doctor. Don’t keep taking more; you might be masking something serious.
Can I use OTC meds during pregnancy?
Some are safe in moderation - like acetaminophen for headaches or prenatal-safe antacids. But NSAIDs like ibuprofen and naproxen should be avoided after 20 weeks of pregnancy. Always check with your OB-GYN before taking any OTC drug while pregnant. What’s safe for others isn’t always safe for you.
What’s the biggest mistake people make with OTC meds?
Taking multiple OTC products that contain the same active ingredient. For example, taking Tylenol for pain and a cold medicine that also has acetaminophen - and doubling your dose. That’s how liver damage happens. Always read the “Active Ingredients” section on every bottle, even if it’s from different brands.
What to Do Next
Next time you reach for an OTC bottle, pause. Ask yourself: Is this a one-time fix? Or am I hiding a problem? If it’s the latter, don’t wait. Talk to your pharmacist or doctor. Keep a symptom diary - note when it started, how bad it is, and what you took. That info helps your provider make better decisions.
And remember: just because something is easy to buy doesn’t mean it’s easy to use safely. Your body isn’t a vending machine. Treat your health like you’d treat your car - with regular checkups, not just when the warning light flashes.




Alex Ramos
November 11, 2025 AT 03:32Just had to laugh at the part about OTC epinephrine auto-injectors going OTC - took me 3 years to stop panicking every time I saw someone pull one out in public. Now I just nod like I know what I’m doing. 😅 Honestly, this article nailed it: OTC doesn’t mean ‘no consequences.’ I used to crush ibuprofen like candy during finals week. Ended up with gastritis. Now I keep a symptom journal. Best decision ever. Thanks for the reminder that pills aren’t candy.
Amie Wilde
November 12, 2025 AT 13:59OTC meds are fine if you’re not dumb. Stop mixing stuff. Read labels. Done.
Gary Hattis
November 14, 2025 AT 02:11As someone who grew up in a household where ‘if it’s on the shelf, it’s fine’ was the mantra, this hit different. My abuela used to give me Tums for everything - headaches, stomachaches, even ‘bad vibes.’ Turns out, she was just trying to keep me quiet. But here’s the thing: in my community, pharmacists are the real MVPs. They know your name, your meds, your kid’s allergies. I’ve had them tell me, ‘bro, that’s not a cold, that’s your heart acting up.’ No doctor visit needed. Just a $2 consultation and a side-eye. We need more of this. The system’s broken, but the pharmacist’s counter? Still sacred ground.
Esperanza Decor
November 14, 2025 AT 12:19Okay but why is no one talking about how the FDA approves OTC drugs based on corporate lobbying, not public health? Like, yes, fexofenadine is safe - but only if you’re under 65, not diabetic, not on antidepressants, and not breathing through your nose. The system is rigged. They push things OTC because insurance won’t cover them anymore, and they want you to pay out of pocket. And don’t get me started on ‘natural remedies’ sold next to the ibuprofen. That’s not healthcare, that’s capitalism with a smiley face. I’ve seen people spend $80 a month on ‘immune boosters’ while ignoring their actual prescription meds. This isn’t empowerment - it’s exploitation dressed up as convenience.
Deepa Lakshminarasimhan
November 16, 2025 AT 10:22They’re hiding something. Why did they make epinephrine OTC? So you don’t go to the ER and they don’t have to pay for it. Same with birth control pills coming OTC - they don’t want you seeing a doctor, they want you buying it like candy. And what about the side effects they don’t tell you? I read a study once - it said OTC NSAIDs increase risk of sudden cardiac death in people over 50. But no one talks about that. They just want you to buy it. They don’t care if you die. It’s all about profit. The system is a scam. Always has been.
Erica Cruz
November 17, 2025 AT 21:13Wow. A 2000-word essay on ‘don’t take too much Tylenol.’ Groundbreaking. I’m shocked this isn’t on the front page of The Lancet. Truly, the pinnacle of medical journalism. Also, ‘pharmacists are your secret weapon’? No. They’re overworked, underpaid, and paid by the chain to upsell you on probiotics and vitamin D. This article reads like a corporate whitepaper written by a marketing intern who Googled ‘pharmacology 101’ for 45 minutes. You’re not empowering people - you’re gaslighting them into thinking they’re safe because they didn’t pay $120 for a prescription.
Johnson Abraham
November 19, 2025 AT 10:16lol otc meds are fine until u get kidney fail. i used to take 4 advil a day for back pain. then i had to go to er for 3 days. now i just lay on the floor and cry. thanks for nothing, big pharma. also, why is everyone so scared of doctors? just go. they’re not scary. unless u have a 2000 dollar bill. then they’re scary.
Shante Ajadeen
November 20, 2025 AT 08:27Really appreciate this. I’m a nurse, and I see so many people suffering because they’re scared of the cost or embarrassed to ask for help. You’re right - the pharmacist is your best friend. I always tell my patients: ‘If you’re not sure, ask. Even if it’s dumb.’ There’s no such thing as a dumb question when it comes to your body. And if you’ve been taking that antacid for months? Yeah, go see someone. It’s not weak. It’s smart. You’re not failing - you’re just choosing to take care of yourself better. Keep going.