Topical steroids are one of the most common treatments for eczema, psoriasis, and other inflamed skin conditions. Millions of people use them every year - and most get relief without issues. But if you use them the wrong way, especially for too long or on sensitive areas, your skin can start to thin. This isn’t rare. It’s preventable. And knowing how to use them properly makes all the difference.
What Are Topical Steroids and Why Are They Used?
Topical corticosteroids are creams, ointments, gels, or lotions applied directly to the skin to calm redness, itching, and swelling. They work by blocking the body’s inflammatory response right where it’s needed. Unlike oral steroids that affect your whole body, topical versions mostly stay on the skin. Skin cells break them down before much gets into your bloodstream, which makes them much safer for long-term use - if used correctly.
They’re not a cure. They’re a tool to control flares. For someone with severe eczema, a strong steroid cream can clear up a flare in under a week. But if you keep using it after the rash is gone, you’re not helping - you’re risking damage.
Not All Steroids Are the Same
There are seven levels of potency, from mild (like over-the-counter hydrocortisone) to super-potent (like clobetasol). The strength you need depends on your condition, where it is, and how bad it is.
- Mild (Class VI-VII): Hydrocortisone 1%. Safe for face, eyelids, groin, and babies. Used for mild rashes.
- Moderate (Class IV-V): Triamcinolone, mometasone. Good for body folds, arms, legs. Often used for moderate eczema.
- Strong to Super-Potent (Class I-III): Clobetasol, betamethasone. Only for thick skin - palms, soles, scalp. Never on the face or genitals unless a doctor says so.
The vehicle matters too. Ointments are greasy but more powerful because they lock moisture in. Creams are lighter, better for weepy skin. Gels and foams are great for hairy areas like the scalp. Using the wrong form can make treatment less effective - or increase side effects.
How Much Should You Use? The Fingertip Unit Rule
Most people use too little or too much. And both cause problems.
A fingertip unit (FTU) is the amount of cream or ointment squeezed from a tube along the length of an adult’s index finger - from the tip to the first crease. One FTU covers an area about the size of two adult hands.
- One arm: 3 FTUs
- One leg: 6 FTUs
- One hand (front and back): 1 FTU
- Face and neck: 2.5 FTUs
- Entire back: 14 FTUs
Doctors say: “A thin layer, rubbed in until it disappears.” If you can see a white layer sitting on top, you’re using too much. Too little means the flare won’t clear - and you’ll keep applying it longer, increasing your risk of side effects.
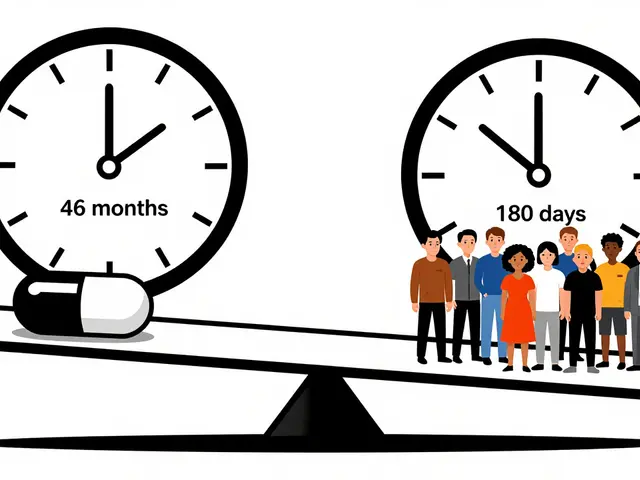
How Long Is Too Long?
Here’s the hard truth: long-term use = higher risk of skin thinning.
Super-potent steroids should never be used for more than two weeks without a doctor’s supervision. Even moderate ones shouldn’t go beyond four weeks on the same spot. After that, you need to step down - switch to a weaker steroid or a non-steroid alternative like tacrolimus or crisaborole.
Why? Because your skin doesn’t bounce back easily once it thins. Thinning (atrophy) looks like transparent, wrinkled skin that bruises easily. Stretch marks (striae) can appear even without weight gain. In extreme cases, blood vessels become visible, and wounds heal slowly.
And here’s something many don’t realize: using too little can be just as dangerous as using too much. If you don’t use enough to control the inflammation, your eczema keeps flaring. You end up applying steroid more often, for longer - which increases the chance of side effects. It’s a cycle.

Where You Apply Matters More Than You Think
Your skin is thicker in some places, thinner in others. That’s why potency guidelines exist.
Never use anything stronger than mild hydrocortisone on your face - especially around the eyes. Prolonged use here can cause cataracts, glaucoma, or perioral dermatitis - a red, bumpy rash around the mouth. The groin, armpits, and breasts are also high-risk zones. Even moderate steroids can cause thinning there.
On the other hand, thick skin on the palms and soles can handle stronger steroids. That’s why doctors prescribe clobetasol for stubborn hand eczema - but only for short bursts.
What Happens When You Stop?
Sometimes, people stop using steroids suddenly - especially after long-term use. That’s when withdrawal can happen.
Symptoms include burning, redness, itching, and swelling that’s worse than the original flare. This isn’t an allergy. It’s your skin reacting to the sudden absence of the drug. It’s called topical steroid withdrawal (TSW). It’s not officially recognized by all medical bodies, but thousands of patients report it - especially those who used strong steroids on the face for months or years without medical oversight.
The fix? Tapering. Don’t quit cold turkey. Gradually reduce frequency - use it every other day, then twice a week, then stop. Switch to a lower potency. Combine with emollients. Work with your doctor. This reduces the shock to your skin.
How to Use Them With Moisturizers
Moisturizers aren’t optional. They’re part of the treatment. But timing matters.
Apply your steroid first - on clean, dry skin. Wait 20 to 30 minutes. Then apply your moisturizer. If you put moisturizer on first, it blocks the steroid from being absorbed. You’re wasting the medicine. And if you mix them in your hand? You’re diluting it. That’s a common mistake.
Also, wash your hands after applying - unless you’re treating your hands. Otherwise, you risk spreading the steroid to other areas, like your eyes.
What Are the Alternatives?
Non-steroid options exist - and they’re growing in use.
- Calcineurin inhibitors (tacrolimus, pimecrolimus): Good for face and sensitive skin. No skin thinning. But they can cause burning at first.
- Crisaborole: A non-steroid ointment for mild-to-moderate eczema. Safe for kids over 2.
- PDE4 inhibitors: Newer, less irritating, but more expensive.
They’re not perfect. They cost more. Insurance doesn’t always cover them. But for long-term maintenance - especially on the face - they’re often the smarter choice.
Many dermatologists now use a “step-down” approach: start with a strong steroid to get control, then switch to a non-steroid or weaker steroid to keep things calm.
Real Stories, Real Risks
One woman in Belfast used clobetasol on her face for six months to treat a stubborn rash. When she stopped, her skin turned bright red, burned constantly, and peeled. She spent months recovering. Another man applied super-potent steroid to his inner thighs for years. He ended up with visible stretch marks and thin skin that tore easily.
But the success stories are everywhere too. A teenager with severe eczema used a moderate steroid for two weeks, then switched to a moisturizer and a low-potency cream twice a week. His skin stayed clear for a year. No thinning. No flare-ups.
The difference? Guidance. Discipline. Knowing when to stop.
What Should You Do?
1. Follow your doctor’s instructions exactly. Don’t guess. Don’t use leftover tubes from last year.
2. Use the fingertip unit. Measure it. Don’t just squeeze.
3. Never use strong steroids on the face, eyelids, or genitals. Unless your doctor writes it down - don’t do it.
4. Stop after 2-4 weeks. If it’s not better, see your doctor. Don’t keep using it.
5. Use moisturizers - but wait 20-30 minutes after the steroid.
6. Ask about non-steroid options if you need long-term control.
Topical steroids are powerful. They’ve helped millions. But they’re not harmless. Skin thinning isn’t a myth. It’s a real, documented risk - and it’s preventable.
The goal isn’t to avoid steroids. It’s to use them smartly. Short. Strong. Then stop. That’s how you get relief - without the damage.
Can topical steroids cause permanent skin thinning?
Yes, if used incorrectly - especially high-potency steroids on thin skin (face, groin, armpits) for more than a few weeks. Once skin atrophy occurs, it doesn’t always fully reverse. The earlier you stop and get help, the better your chances of recovery. Long-term damage like visible blood vessels or stretch marks may remain.
Is it safe to use hydrocortisone cream every day?
Over-the-counter hydrocortisone (1%) is low potency and generally safe for short-term use - up to 7 days. But using it daily for weeks or months, even mild, can still cause thinning, especially on the face or in skin folds. It’s not meant for chronic daily use. If you need it every day, talk to your doctor. There are better long-term options.
Why do some people say steroids make their skin worse after stopping?
This is called topical steroid withdrawal (TSW). It happens mostly after long-term, unsupervised use of strong steroids. The skin becomes dependent on the drug to suppress inflammation. When you stop, the inflammation rebounds - often worse than before. Symptoms include burning, redness, flaking, and intense itching. Tapering off slowly under medical supervision reduces this risk.
Can I use steroid cream on my baby’s face?
Only mild hydrocortisone 1%, and only for a few days at a time. Babies’ skin is thin and absorbs more. Never use anything stronger without a pediatric dermatologist’s approval. Always pair it with fragrance-free moisturizers. If the rash doesn’t improve in 3-5 days, see a doctor - don’t keep applying.
Are non-steroid creams better than steroids?
They’re safer for long-term use, especially on sensitive skin. But they don’t work as fast or as strongly as steroids. For a sudden, severe flare, steroids are still the gold standard. Non-steroids are better for maintenance - keeping skin calm between flares. Many doctors use both: steroids to get control, non-steroids to keep it.
How do I know if my steroid cream is too strong?
If you’re using it on your face, eyelids, or genitals and it’s not labeled as mild, it’s probably too strong. Also, if your skin looks thinner, more wrinkled, or bruised easily after a few weeks - stop and see your doctor. Strong steroids should only be used on thick skin (palms, soles) and for short periods. If you’re unsure, ask your pharmacist or doctor to confirm the potency class.





Peter Aultman
November 13, 2025 AT 04:21Used clobetasol on my elbows for a month because the eczema wouldn’t quit. Skin looked like crepe paper after. Stopped cold turkey and it got worse. Took 6 months to recover. Never doing that again. Just use moisturizer now.
Jane Johnson
November 14, 2025 AT 18:26While your information is technically accurate, it ignores the psychological dependency many patients develop. The fear of flare-ups drives continued use-even when medically contraindicated. This is not merely a pharmacological issue; it is a behavioral one.
Sean Hwang
November 15, 2025 AT 22:50FTU rule saved my life. I used to just squeeze out a whole line like toothpaste. Turns out I was using 10x more than needed. Once I started measuring, my rash cleared in 3 days and no thinning. Seriously, try it.
Barry Sanders
November 17, 2025 AT 02:09Wow. Another ‘just follow your doctor’ sermon. What about the people whose doctors don’t know this stuff? Or worse-give them clobetasol for their face? This isn’t education. It’s damage control after the fact.
Chris Ashley
November 17, 2025 AT 04:43Bro I used hydrocortisone on my neck every day for 2 years. Now my skin looks like a crumpled paper bag. I didn’t even realize it was happening until my girlfriend said ‘why does your neck look like that?’
kshitij pandey
November 17, 2025 AT 05:01In India, many people use steroid creams like magic lotion. Grandmas apply them to babies for rashes. No one knows about potency levels. This post is needed everywhere. Thank you for explaining FTU-it’s a game changer.
Brittany C
November 17, 2025 AT 06:30The pharmacokinetic profile of topical corticosteroids is highly dependent on vehicle composition, stratum corneum integrity, and occlusion. Misapplication leads to increased percutaneous absorption, which elevates systemic exposure risk-even with low-potency agents.
Sean Evans
November 18, 2025 AT 12:07STOP USING STEROIDS. 😡 I used them for acne. Now my face is a red, burning mess. Doctors don’t warn you. They just hand out tubes like candy. This is medical negligence. 🤬
Anjan Patel
November 18, 2025 AT 17:03Everyone thinks they’re smart until they’re the one with the thin, translucent skin on their eyelids. I watched my sister go through TSW for 18 months. She cried every night. This isn’t a ‘lifestyle tip.’ It’s a tragedy waiting to happen.
Scarlett Walker
November 19, 2025 AT 14:28I switched to crisaborole after my dermatologist scared me with pictures of skin atrophy. It burns at first but worth it. My skin hasn’t looked this good since I was 16. No steroids. No fear.
Hrudananda Rath
November 21, 2025 AT 05:43One must acknowledge the epistemological vacuum in contemporary dermatological pedagogy. The dissemination of such information remains confined to academic journals, while the lay populace remains tragically ignorant of the biochemical consequences of topical glucocorticoid administration.
Brian Bell
November 22, 2025 AT 18:37FTU rule is legit. I thought I was being careful. Turns out I was using 4x too much. Now I measure like a scientist. Skin is calm. No drama. 🙌
Nathan Hsu
November 23, 2025 AT 09:16Let me be clear: The use of topical corticosteroids, particularly in pediatric populations, demands rigorous adherence to clinical guidelines, as the integumentary system of the young is disproportionately susceptible to iatrogenic atrophy due to increased transdermal permeability and immature metabolic pathways.
Ashley Durance
November 23, 2025 AT 18:14Most people don’t even know what ‘potency class’ means. They grab whatever’s on the shelf. This isn’t ignorance-it’s negligence. And now we’re seeing whole generations with permanently damaged skin.
Scott Saleska
November 24, 2025 AT 02:36Actually, you missed something important. Even if you use the right amount and stop on time, some people still get thinning because of genetics. I’ve seen it. My cousin used hydrocortisone for three weeks on her wrists and now she has permanent stretch marks. It’s not always about how you use it-it’s who you are.