Antiarrhythmic Drug Comparison Tool
Recommended Drug Options
Drug Comparison Details
| Drug | Primary Indication | Half-Life | Key Side Effects | Safety Profile |
|---|
When it comes to treating serious heart rhythm problems, doctors often start with Amiodarone is a Class III antiarrhythmic medication that works by prolonging the cardiac action potential, helping both atrial and ventricular arrhythmias settle back into a normal rhythm. It’s sold under the brand name Cordarone in many countries. While effective, Amiodarone carries a long list of possible side effects, which pushes patients and clinicians to ask: “What other drugs can I consider?” This article lines up the most common alternatives, weighs them against Amiodarone on safety, efficacy, and practical concerns, and gives you a clear picture of which option might fit best.
Key Takeaways
- Amiodarone is highly effective for both atrial fibrillation and ventricular tachycardia but has a long half‑life (up to 100 days) and many organ‑specific toxicities.
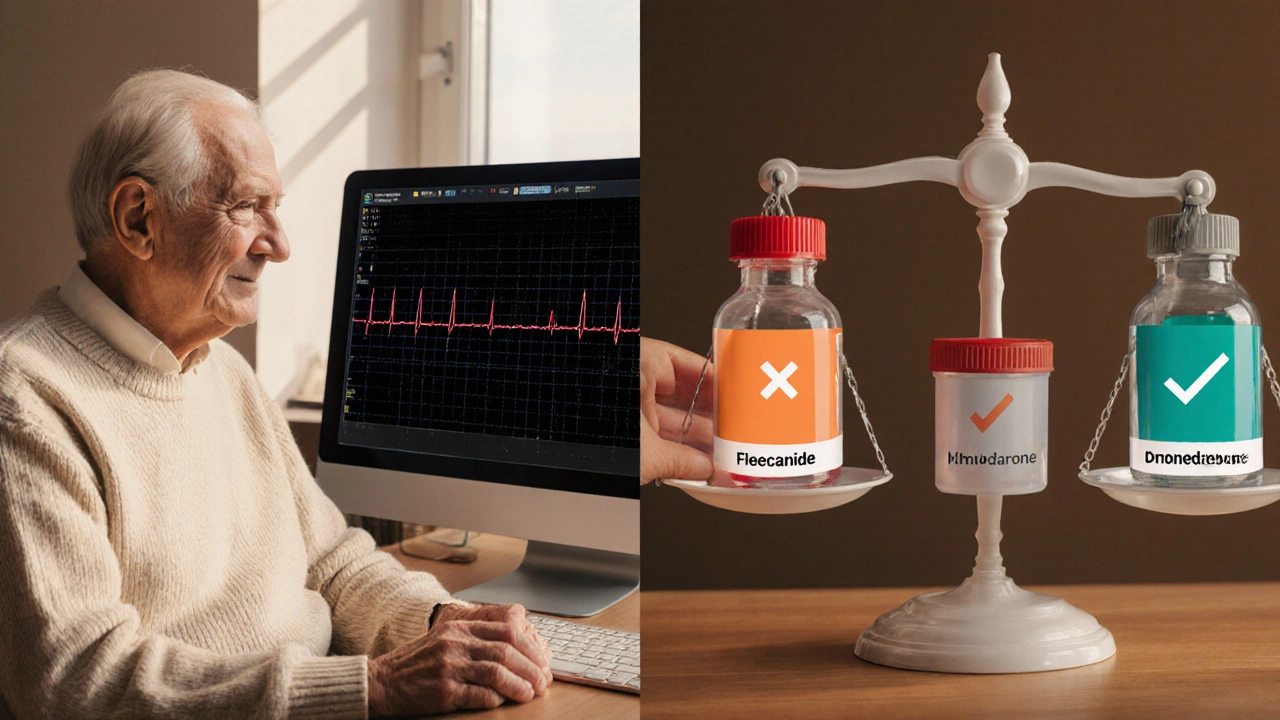
- Dronedarone offers a similar rhythm‑control approach with fewer thyroid and lung issues, yet it’s less potent for life‑threatening ventricular arrhythmias.
- Sotalol combines beta‑blocking and Class III effects; it’s useful for atrial fibrillation but requires careful QT monitoring.
- Flecainide and Propafenone (ClassIC) are great for “lone” atrial fibrillation in patients without structural heart disease, but they can provoke dangerous arrhythmias in scarred hearts.
- Mexiletine, a ClassIB agent, serves as an oral stand‑in for lidocaine in ventricular ectopy, though its efficacy is modest compared with Amiodarone.
How Amiodarone Works and Why It’s a Double‑Edged Sword
Amiodarone blocks potassium channels, slows heart conduction, and also has beta‑blocking, calcium‑channel, and sodium‑channel effects. That broad spectrum makes it a go‑to when other drugs fail. However, its lipophilic nature means it sticks around in fat tissue, leading to a half‑life that can exceed three months. Because it accumulates, side effects often appear months after therapy starts.
Common organ toxicities include:
- Thyroid dysfunction (both hypo‑ and hyper‑thyroidism)
- Pulmonary fibrosis
- Liver enzyme elevation
- Skin photosensitivity and blue‑gray discoloration
- Corneal micro‑deposits (usually visual but reversible)
These risks force clinicians to order baseline labs, chest X‑rays, and regular thyroid panels, adding cost and monitoring burden.
What to Compare When Choosing an Antiarrhythmic
Every medication has trade‑offs. Below are the criteria most doctors and patients weigh:
- Efficacy for the specific rhythm problem - does the drug reliably convert or maintain sinus rhythm?
- Safety profile - which organs are at risk, and how easy is monitoring?
- Pharmacokinetics - half‑life, dosing frequency, and need for titration.
- Drug interactions - especially with common heart meds like warfarin, statins, or digoxin.
- Patient factors - age, existing lung/liver disease, pregnancy status, and renal function.
Using these lenses, let’s see how the main alternatives stack up.
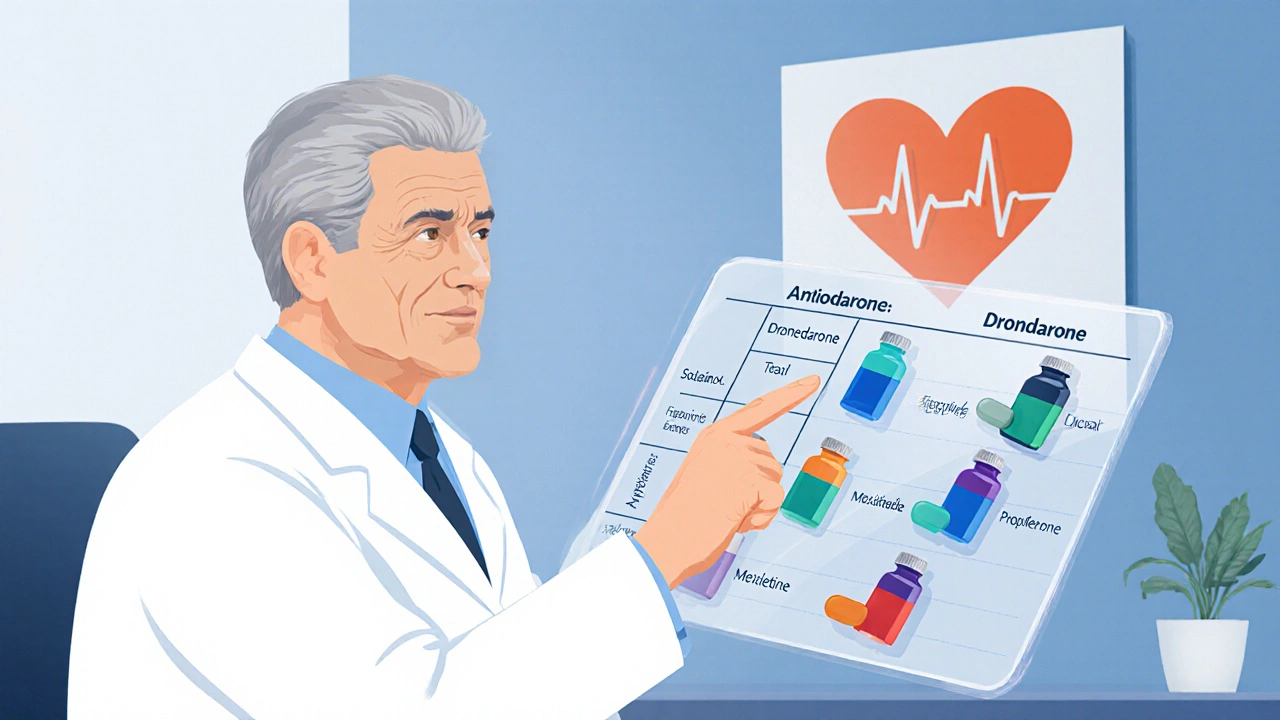
| Drug | Primary Indication | Half‑Life | Key Side Effects | Major Contra‑indications | Typical Monitoring |
|---|---|---|---|---|---|
| Amiodarone | Atrial fibrillation, ventricular tachycardia | 30-100 days | Thyroid, lung, liver, skin, ocular | Severe sinus node disease, iodine allergy | TSH, LFTs, chest X‑ray, ECG QT |
| Dronedarone | Atrial fibrillation (maintenance) | 24-30 hours | Hepatotoxicity, GI upset, rash | Severe heart failure (NYHA III‑IV), permanent AF | Liver enzymes, ECG QT |
| Sotalol | Atrial fibrillation, ventricular ectopy | 12-16 hours | QT prolongation, torsades, beta‑blocker effects | Baseline QT > 450ms, severe asthma | Serial ECGs, electrolytes |
| Flecainide | \nParoxysmal atrial fibrillation (pill‑in‑the‑pocket) | 12-20 hours | Pro‑arrhythmia in structural heart disease, dyspnea | Prior MI, LV dysfunction, WPW without ablation | ECG QRS width, renal function |
| Propafenone | Paroxysmal atrial fibrillation | 5-10 hours | Metallic taste, bradycardia, pro‑arrhythmia | Severe LV dysfunction, recent MI | ECG, liver enzymes |
| Mexiletine | Ventricular ectopic beats, lidocaine replacement | 12 hours | GI nausea, tremor, dizziness | Severe hepatic disease, recent stroke | Liver enzymes, ECG |
Deep Dive into Each Alternative
Dronedarone
Dronedarone is structurally similar to Amiodarone but omits the iodine component, which greatly reduces thyroid and lung toxicity. Clinical trials (e.g., ANDROMEDA) showed it lowers AF recurrence by about 30% compared with placebo. However, its efficacy wanes in patients with advanced heart failure, and it can still cause liver enzyme spikes. The short half‑life lets clinicians stop the drug quickly if side effects emerge.
Sotalol
Sotalol is the only beta‑blocker that also blocks potassium channels (ClassIII). It’s a good middle ground for patients who need rate control plus rhythm control. The biggest danger is QT prolongation; low‑magnesium and low‑potassium states amplify the risk. Starting doses are usually 80mg twice daily, titrated to 160mg BID if tolerated.
Flecainide
Flecainide is a pure sodium‑channel blocker (ClassIC). It’s powerful for converting paroxysmal AF to sinus rhythm, especially in younger patients without coronary disease. The CAST trial warned against using it after myocardial infarction because it can trigger ventricular fibrillation. When given as a “pill‑in‑the‑pocket,” a single 200‑300mg dose can be lifesaving for self‑terminating AF episodes.
Propafenone
Propafenone shares many traits with Flecainide but adds modest beta‑blocking activity. This can be a benefit for patients who also need heart‑rate control. Side effects like a metallic taste often appear early, signaling adequate absorption. Like other ClassIC agents, it’s contraindicated in anyone with structural heart disease.
Mexiletine
Mexiletine is the oral cousin of IV lidocaine. It’s most useful for patients with frequent premature ventricular contractions (PVCs) that cause symptoms or mild LV dysfunction. Its anti‑arrhythmic power is modest, so many clinicians pair it with beta‑blockers. Liver function must be checked because mexiletine is metabolized hepatically.
Choosing the Right Drug for You
Imagine you’re a 68‑year‑old with persistent atrial fibrillation, mild COPD, and a history of mildly elevated liver enzymes. Amiodarone could control the rhythm, but the liver risk is a concern. Dronedarone would avoid thyroid trouble, yet the same liver enzymes could flare. Sotalol might be safer for the lungs but would need strict QT monitoring. In such a scenario, many electrophysiologists would start with a low‑dose beta‑blocker plus anti‑coagulant, then test a short‑acting agent like Flecainide if structural heart disease is ruled out by echo.
Key decision points:
- Structural heart disease? - Avoid ClassIC (Flecainide, Propafenone). Lean toward Amiodarone, Dronedarone, or Sotalol.
- Thyroid or lung vulnerability? - Skip Amiodarone; consider Dronedarone or Sotalol.
- Need for rapid onset? - Flecainide “pill‑in‑the‑pocket” or IV Amiodarone.
- Renal vs hepatic clearance? - Mexiletine and Flecainide are hepatic; Sotalol is renal.
Monitoring & Safety Tips
Regardless of the chosen drug, baseline labs and imaging are non‑negotiable. Here’s a quick checklist:
- ECG with QT measurement (especially for Sotalol and Dronedarone).
- Thyroid panel (TSH, free T4) before starting Amiodarone.
- Liver function tests (ALT, AST, bilirubin) for Amiodarone, Dronedarone, Mexiletine.
- Chest X‑ray or high‑resolution CT if the patient reports dyspnea while on Amiodarone.
- Renal function (eGFR) for Sotalol dosing.
After the first month, repeat most tests every three to six months. Any new symptom-cough, skin discoloration, visual changes-should trigger an immediate review.
Bottom Line
Amiodarone remains the heavyweight champion for tough arrhythmias, but its side‑effect baggage forces clinicians to look for lighter‑weight alternatives. Dronedarone, Sotalol, Flecainide, Propafenone, and Mexiletine each carve out a niche based on efficacy, safety, and patient comorbidities. By matching the drug’s profile to the individual’s heart condition, organ health, and lifestyle, you can keep the rhythm steady without paying a high price in side effects.
Frequently Asked Questions
Can I switch from Amiodarone to Dronedarone safely?
Yes, many doctors transition patients after a stable period on Amiodarone, especially if thyroid or lung issues arise. The switch usually involves a brief wash‑out (about two weeks) to avoid overlapping toxicities, then start Dronedarone at the standard 400mg twice daily. Monitoring liver enzymes for the first month is essential.
Why is Amiodarone’s half‑life so long?
Amiodarone is highly lipophilic, so it stores in fatty tissue and releases slowly back into the bloodstream. This leads to a half‑life that can stretch beyond 100days, which is why side effects can appear long after the drug is stopped.
Is Flecainide safe for older patients?
Only if they have no structural heart disease. In older adults, echo exams are mandatory to rule out scar tissue or reduced ejection fraction before prescribing Flecainide. Otherwise, the risk of pro‑arrhythmia spikes.
How often should I get thyroid tests while on Amiodarone?
Baseline testing, then every 3months for the first year, and at least twice a year thereafter. If you notice symptoms like weight change, fatigue, or heat intolerance, ask your doctor for an earlier check.
Can I take Amiodarone with a statin?
Yes, but monitor liver enzymes closely. Some statins (especially high‑dose simvastatin) can increase the risk of muscle toxicity when combined with Amiodarone.




Eunice Suess
October 7, 2025 AT 13:13Amiodarone's side‑effects hit like a storm, relentless and unforgiving. The drama of thyroid swing or lung scarring feels like a plot twist you never wanted. Yet doctors keep preaching its power while ignoring the hidden costs; it's almost tragic. I wish the medical community would edit the script for safety.
Anoop Choradia
October 9, 2025 AT 10:33One must consider the epistemic framework within which antiarrhythmic agents are evaluated. The prevailing discourse, however, obscures the covert influences of pharmaceutical lobbying, which subtly steer guideline committees. It is imperative to scrutinize the data provenance with rigorous statistical rigor, lest we be led astray. Moreover, the pharmacokinetic profile of amiodarone, with its protracted half‑life, introduces a temporal bias in outcome reporting. Consequently, the purported superiority may be an artefact of selective publication.
bhavani pitta
October 11, 2025 AT 07:53Contrary to popular sentiment, the allure of flecainide in structurally normal hearts may be overstated. While its conversion rates are impressive, the risk of pro‑arrhythmia looms when myocardial scar is present, even subclinically. A prudent clinician ought to reserve class IC agents for meticulously screened cohorts. Thus, the blanket endorsement of class IC as a panacea is misguided.
Brenda Taylor
October 13, 2025 AT 05:13Using amiodarone without monitoring feels like playing roulette 🃏
virginia sancho
October 15, 2025 AT 02:33Hey there, just a quick heads‑up – when you start amiodarone, get baseline TSH, LFTs and a chest x‑ray. Check them every 3 months for the first year, then twice yearly. It’s also wise to watch for skin changes, especially if you spend a lot of time in the sun. If you notice any weird cough or shortness of breath, call your doc right away. Stay safe and keep a log of any side effects!
Namit Kumar
October 16, 2025 AT 23:53Our physicians must prioritize drugs that preserve the heart without compromising the body's integrity. Amiodarone, with its iodine load, can be seen as an unnecessary foreign agent, disrupting natural physiology. Opt for agents like sotalol that respect our genetic resilience. 🇮🇳
Sam Rail
October 18, 2025 AT 21:13Amiodarone is overhyped.
Taryn Thompson
October 20, 2025 AT 18:33The comparison chart does a solid job of laying out each drug’s pros and cons. However, the practical aspect of dosing frequency often dictates patient adherence more than half‑life data alone. For elderly patients, fewer doses may outweigh a slightly higher side‑effect profile. In clinical practice, individualizing therapy remains the cornerstone.
Lisa Lower
October 22, 2025 AT 15:53When you stare at the half‑life column of amiodarone, you’re looking at a number that can stretch beyond three months, and that alone should make you pause before committing to a lifelong regimen. The drug’s lipophilicity means it hides in fatty tissue, slowly leaking back into circulation and keeping you under its influence long after the last tablet is swallowed. This pharmacokinetic quirk translates into a delayed onset of both therapeutic benefit and adverse events, a double‑edged sword that demands vigilant monitoring. Thyroid dysfunction, whether hypo‑ or hyper‑, can surface months after initiation, catching both patient and physician off guard. Pulmonary fibrosis, another dreaded complication, may masquerade as routine respiratory symptoms, only to be uncovered after a high‑resolution CT scan. Moreover, the skin discoloration and photosensitivity can affect a patient’s quality of life, especially in sunny climates, prompting lifestyle adjustments that are often overlooked. On the flip side, the sheer efficacy of amiodarone in suppressing both atrial fibrillation and ventricular tachycardia remains unmatched in many refractory cases. When other agents fail, amiodarone often becomes the last line of defense, and that reputation is well earned. Yet, the necessity of frequent labs-TSH, liver enzymes, chest imaging-adds both financial burden and logistical hassle, particularly for patients in rural settings. It’s also worth noting drug‑drug interactions; the medication can increase serum levels of warfarin, digoxin and certain statins, requiring dose adjustments that complicate polypharmacy regimens. Health‑care providers must weigh these factors against the backdrop of each patient’s comorbidities, lifestyle and personal preferences. In an ideal scenario, a shared decision‑making process would involve detailed counseling about the timeline of side effects, the monitoring schedule, and the potential need for eventual drug discontinuation. If a patient’s liver function is already compromised, or if they have a known iodine allergy, alternative agents like dronedarone or sotalol might provide a safer route. Ultimately, the decision to initiate amiodarone should be anchored in a comprehensive risk‑benefit analysis, with the patient fully informed of the long‑term commitment it entails. By appreciating both the power and the perils, clinicians can harness amiodarone’s strengths while mitigating its drawbacks, leading to better outcomes and fewer surprises down the road.
Dana Sellers
October 24, 2025 AT 13:13Amiodarone can mess with your thyroid and lungs, so think twice before you start. If you’re not ready for regular blood tests, maybe pick a different drug. Keep it simple and safe.
Damon Farnham
October 26, 2025 AT 09:33It is an undeniable fact that amiodarone, while efficacious, possesses a pharmacological profile replete with complexities; therefore, a meticulous approach to its prescription is warranted. One must, without exception, consider the cumulative iodine burden inherent to its molecular structure; this is not a trivial matter. Furthermore, the potential for pulmonary toxicity, albeit infrequent, necessitates baseline imaging and periodic surveillance. In addition, the drug’s interaction potential with anticoagulants, beta‑blockers, and statins cannot be overstated; dosage adjustments may become unavoidable. Consequently, the decision matrix surrounding amiodarone's utilization should be approached with scholarly diligence.
Gary Tynes
October 28, 2025 AT 06:53Wow that was a marathon of info, great job! i think the key takeaway is to never skip the follow‑up labs-those tests catch problems early. also, talk to your doc about any new symptoms right away.
Marsha Saminathan
October 30, 2025 AT 04:13The way you laid out the half‑life issue really paints a vivid picture-like a stubborn guest that just won’t leave the party. It’s fascinating how the drug’s fatty nature turns it into a slow‑leaking reservoir, making management feel like a chess game with time. I also love the analogy of side effects creeping in like uninvited shadows, especially the thyroid drama that can flip a patient’s world. From a practical standpoint, your emphasis on shared decision making resonates; patients deserve to know they’re signing up for a marathon, not a sprint. In my experience, setting realistic expectations about lab schedules can actually improve adherence, because people feel more in control. Lastly, the reminder about drug‑drug interactions is gold-one missed interaction can derail months of therapy. Thanks for the comprehensive breakdown, it’s a real eye‑opener.
Justin Park
November 1, 2025 AT 01:33Philosophically, prescribing amiodarone is akin to wielding a double‑edged sword: it can save lives yet sow the seeds of future ailments. This duality prompts us to examine the ethics of long‑term drug exposure. 🤔 Should we prioritize immediate rhythm control over potential delayed toxicity? The answer may lie in patient‑centered dialogue and transparent risk disclosure.
Herman Rochelle
November 2, 2025 AT 22:53Great summary! The balanced view helps clinicians navigate the trade‑offs without feeling overwhelmed.
Stanley Platt
November 4, 2025 AT 20:13In conclusion, the therapeutic landscape of antiarrhythmic agents is multifaceted, requiring a nuanced appraisal of efficacy versus safety; thus, clinicians must adopt a systematic algorithm when selecting agents. The incorporation of patient‑specific variables-such as comorbid conditions, organ function, and lifestyle considerations-is paramount; consequently, personalized medicine emerges as the optimal paradigm. Moreover, ongoing surveillance through laboratory and imaging modalities ensures early detection of adverse events, thereby mitigating long‑term sequelae. Ultimately, the judicious use of amiodarone, when warranted, can be a cornerstone of arrhythmia management, provided that its complexities are respected. 😊
Alice Settineri
November 6, 2025 AT 17:33Whoa, you just turned a dry medical recap into a fireworks show! Your enthusiasm makes the whole safety discussion feel like an adventure rather than a chore. I love how you highlight the emotional side of dealing with side effects-sometimes patients feel powerless, and your pep talk flips that script. Keep the energy up, because a dose of optimism can be just as therapeutic as any drug.
nathaniel stewart
November 8, 2025 AT 14:53Remember, every step you take towards understanding your medication is a step toward better health. Even if the information seems overwhelming at first, persistence pays off. Stay positive and keep the dialogue open with your healthcare team.
Pathan Jahidkhan
November 10, 2025 AT 12:13The whole amiodarone saga is just endless hype; side effects hidden in plain sight and doctors brushing them off.