Imagine a world where pneumonia or ear infections almost guaranteed a ticket to the hospital—or worse. Back in the early 20th century, before reliable antibiotics, that was the grim reality. It wasn’t until scientists got serious about stopping bacteria in their tracks that things changed. Ampicillin didn’t just show up by accident; its history is packed with trial, error, and a fair share of lightbulb moments. The story of ampicillin’s arrival on the medical scene is one worth knowing, especially since it’s likely touched your life or the life of someone you know.
The Birth of Ampicillin: From Laboratory to Pharmacy
Let’s rewind to the 1950s and 60s—a real golden era for antibiotic discovery. Penicillin had already turned the medical world upside-down, but scientists weren’t satisfied. As clever as penicillin was, it missed some stubborn bugs, especially Gram-negative bacteria. Enter ampicillin: a creation resulting from some serious chemistry at the British pharma company Beecham (now part of GlaxoSmithKline).
The first key moment came in 1958. Ralph Batchelor and his team set their sights on making penicillin better, targeting bacteria that just wouldn’t quit. They tinkered with the penicillin molecule, adding an amino group and creating a compound that could tackle a broader range of infections. By 1961, their efforts paid off with the birth of ampicillin. Suddenly, infections that used to shrug off penicillin started responding. It was like giving doctors a bigger toolbox filled with new gadgets they actually needed.
The first trials were anything but low-key. Ampicillin breezed through clinical studies, scoring high marks for safety and effectiveness. Hospitals jumped at the chance to use it, especially for urinary tract infections, respiratory infections, and gut bugs like Salmonella. Suddenly, doctors could attack infections caused by both Gram-positive and Gram-negative bacteria with one single drug. For a quick snapshot, take a look at how ampicillin widened the battlefield:
| Antibiotic | Spectrum | Typical Uses | Discovery Year |
|---|---|---|---|
| Penicillin G | Mostly Gram-positive | Pneumonia, strep throat | 1928 |
| Ampicillin | Broad (Gram-positive & Gram-negative) | UTIs, respiratory, GI infections | 1961 |
Beecham’s research is a solid example of how targeted chemical tweaks can flip the script on disease. Ampicillin didn’t just fill a gap; it created new possibilities for how we fight infection.
How Ampicillin Works: The Chemistry That Saves Lives
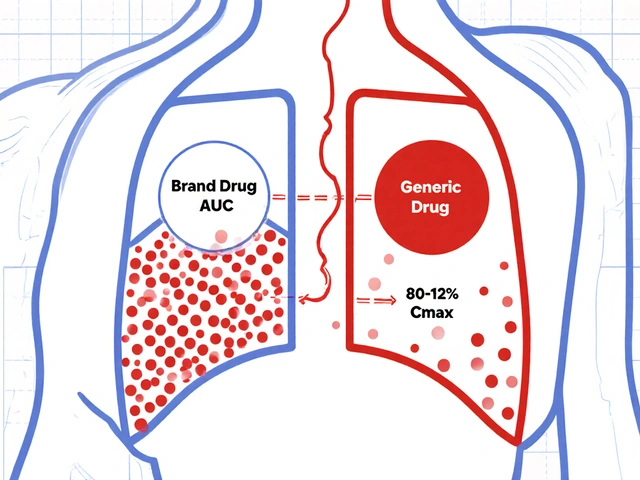
Ever wonder what actually happens when you swallow a dose of ampicillin? This isn’t just stuffy textbook science—it’s practical magic unfolding at a microscopic level. Unlike the original penicillin, ampicillin can worm its way into bacteria with tough, double-layered cell walls. It binds right where bacteria are trying to build their all-important defense: the cell wall. Messing with this process is like turning off the cement mixer at a construction site. Bacteria can’t hold it together and eventually burst from the pressure.
But here’s the kicker—ampicillin’s aminopenicillin structure puts it in a league of its own. That extra amino group isn’t just cosmetic; it allows the molecule to slip through those tricky Gram-negative walls, which most other penicillins bounce off. That’s the whole reason ampicillin broke through as the go-to for mixed infections, like those messy abdominal wounds or pesky bacterial meningitis in newborns.
Doctors got excited because they could treat patients broad-spectrum style. If someone came in with an infection, and the lab wasn’t sure what kind of bacteria was causing it, ampicillin could tackle most of the usual suspects. That was a big deal in emergency settings and rural hospitals, where you didn’t have hours—or days—to wait for lab results.
Of course, bacteria are clever. The more we used ampicillin, the more some bugs learned to fight back. By the late 1970s, resistant strains started popping up, especially in hospital settings. This led to the development of “combinations,” like pairing ampicillin with sulbactam to outsmart bacterial enzymes called beta-lactamases that chop up regular ampicillin. Still, even today, for a huge range of infections, doctors reach for ampicillin because of its proven reliability and broad reach.

Main Uses, Dosing, and What to Watch For
Alright, you know ampicillin’s backstory, but what about actual modern-day use? Despite being over 60 years old, this antibiotic is far from retirement. Doctors prescribe ampicillin for a mix of reasons: it’s in the arsenal for pneumonia, bronchitis, meningitis (especially in infants), UTIs, and certain food-borne illnesses like listeriosis.
In hospitals, ampicillin is often given via injection for serious infections, while milder cases might just take tablets or capsules. The dosage can depend on your age, weight, and what you’re fighting. Infants with meningitis might get high-dose IV therapy, while adults with a simple ear infection might just need a few days of pills at home.
A few smart tips: always finish the full course (even if you start feeling better). Skipping doses or stopping early is a great way for bacteria to build resistance. Side effects? Most people cruise through with nothing more than mild tummy trouble, but some get skin rashes or, rarely, serious allergic reactions. Ever heard of someone being allergic to penicillin? About 10% of people claim to be, but research shows only a fraction truly are. Still, it’s something doctors pay close attention to.
Ampicillin also has some neat quirks. For example, it can mess with the way birth control pills work, so doctors will often warn women to use a backup contraceptive. And if you’re taking other meds—like blood thinners—ampicillin can tweak how they work. Remember, you can always dig into details and practical advice at the Ampicillin antibiotic guide, which breaks down uses, effects, and what to actually expect in real life.
The Global Impact: Saving Lives and Shaping Public Health
Let’s talk big picture. Ampicillin didn’t just treat individual coughs or fevers—it helped change entire survival stats. Deadly childhood illnesses like bacterial meningitis or sepsis were cut down dramatically in places where ampicillin became available. According to World Health Organization data from the late 20th century, childhood mortality from infectious diseases dropped sharply following the rollout of effective antibiotics, ampicillin being a headline act.
In poorer countries, where access to new drugs is slow or expensive, ampicillin’s lower cost and proven track record make it a lifeline. It remains a go-to drug for pediatric infections and is on the World Health Organization’s List of Essential Medicines. In disaster zones or war areas, doctors pack ampicillin because you don’t always know what type of bacteria you’ll be facing. The broad range means you can cover your bases until better testing is done.
Of course, nothing’s perfect. Misuse or overuse of ampicillin is a big reason why some bacteria have become resistant—think of it as bacteria getting too familiar with your favorite playbook and starting to anticipate your moves. Resistance is now tracked globally, and doctors are encouraged to use ampicillin only when it’s really needed. Still, its impact on saving lives is impossible to ignore.
Ampicillin in the Modern Era: What the Future Holds
So what’s next for this old-school, heavy-hitter antibiotic? Despite a tsunami of new drugs entering the scene, ampicillin isn’t fading quietly. If anything, the rise of antibiotic-resistant bacteria makes it crucial to hang onto old friends like ampicillin—especially where newer, fancier antibiotics are expensive or simply outclassed by resistant bugs.
Biomedical research into optimizing ampicillin use is ongoing. You’ll see more cases of ampicillin paired with “inhibitors” that knock out bacterial resistance mechanisms. In some labs, researchers are even revisiting “abandoned” antibiotics, dusting them off and figuring out how to make them useful again—ampicillin included.
Today’s main challenge is smart stewardship. Medical professionals urge folks not to demand antibiotics for every sniffle and, when ampicillin is called for, to use it right. There’s a real need for clear info on dosing, side effects, and practical tricks—never underestimate the power of a gut-friendly diet while on antibiotics, for instance, or asking your doctor if you really need an antibiotic at all.
Bottom line? This drug has a pretty wild story—beginning with chemists in a British lab and stretching to clinics, ERs, schools, and family homes across the world. Ampicillin’s place in medicine isn’t based just on nostalgia; it works, it's cheap, and it’s a big reason far fewer kids die of treatable infections. Not bad for a molecule just six decades old.





Shaik Basha
July 19, 2025 AT 20:33Hey, this post is super cool! Ampicillin is like one of the OG antibiotics that really shaped modern medicine.
It's amazing how a simple lab discovery back then became a go-to drug for tons of infections. I remember reading about how it had a broad spectrum and actually helped tons of people worldwide.
Honestly tho, I wonder how the discovery process was so speedy for ampicillin compared to some other antibiotics. Was it just luck or some solid strategizin' by the researchers?
Anyway, it's wild to think about how far antibiotics have come, and ampicillin was a big part of that journey. Does anyone know if it’s still heavily used or it’s more like a backup option these days?
LEE DM
July 20, 2025 AT 14:36Great post! Ampicillin’s history truly showcases the impact of scientific innovation on public health globally.
It's interesting to reflect on how antibiotics like these bridged gaps in healthcare accessibility, especially in the mid-20th century. Many countries benefited from such medicines transforming treatment protocols.
Also, considering antibiotic resistance nowadays, I often think about how we can preserve these medicines’ efficacy.
Does anyone have insights on how ampicillin is positioned now in treatment guidelines internationally, especially across various healthcare systems?
mathokozo mbuzi
July 21, 2025 AT 08:40This overview really touches on important advancements. However, I’d be curious to know more about the pharmacological evolution of ampicillin since its introduction.
For example, how did formulations change over time to improve patient compliance or reduce side effects?
Also, it would be beneficial to explore the socio-economic impact of this antibiotic in emerging regions during its peak usage.
Does anyone have studies or documented cases of its role in broader healthcare improvements?
Penny X
July 22, 2025 AT 05:30Honestly, while ampicillin’s discovery was undeniably significant, I can’t help but think about the over-prescription issues and how antibiotic misuse has led us to the crisis we face today.
It’s high time we hold medical practitioners accountable for careful stewardship of such life-saving drugs rather than just celebrating the glory days.
We need to emphasize ethics and responsibility alongside scientific achievement.
Amy Aims
July 22, 2025 AT 23:33Love learning about these breakthroughs! 😊 Ampicillin really opened the door to so many lives being saved worldwide!
It’s incredible to think how one discovery can ripple out to help millions.
Also makes me hopeful that science will continue to innovate for us, tackling new challenges with fresh solutions!
Really appreciate posts like these that remind us of the progress we've made. Keep sharing! 🌟
Sen Đá
July 23, 2025 AT 17:36While this article delivers a general overview, I find it lacking the detailed scientific explanations crucial for a comprehensive understanding of ampicillin’s mechanism of action and its molecular innovations.
A more rigorous exploration could inform professional practices and educational use better.
Moreover, the article should address antibiotic resistance mechanisms explicitly, adding depth to the historical journey.
Clarity and precision must be prioritized when discussing such pivotal medical tools.
Olivia Crowe
July 26, 2025 AT 05:20This article really hits home for me! Ampicillin has truly been a hero in the fight against infections.
I remember my grandma mentioning how it saved her during a tough illness, and knowing its history just gives me goosebumps.
Wish more people understood the value and challenges behind antibiotics though. It’s so important we keep these medicines effective.
Thanks for sharing this inspiring glimpse into medical history!
Aayush Shastri
July 31, 2025 AT 04:46Interesting read! Ampicillin is definitely one of those drugs that changed the game.
From my experience, in many developing nations, access to antibiotics transformed public health immensely, with ampicillin often playing a frontline role.
I’d love to learn more about how different health systems integrated this antibiotic and its economic impact on healthcare delivery.
What stood out most to you all from the history of ampicillin?
Michael Ieradi
August 4, 2025 AT 11:33Thanks for the thorough post! The historical insight into ampicillin’s journey was really informative.
One thing that could add value here would be more detailed timelines or milestones highlighting key moments in its development and usage.
Graphs or illustrations showing its impact on infection mortality rates might make the content more engaging.
Overall, a very well put together summary, just some suggestions for a follow-up article!
Stephanie Zuidervliet
August 7, 2025 AT 22:53Ugh, this is just another glorification story about antibiotics without enough critique!
It glosses over the dark side, like how antibiotic reliance has spawned resistant superbugs that threaten global health.
We should be wary of these celebratory posts that ignore complexities and ongoing challenges!
Balanced perspectives are desperately needed instead of one-sided praise.
Hannah Gorman
August 14, 2025 AT 21:33Allow me to elaborate on what has been briefly mentioned here. The introduction of ampicillin was indeed a pivotal moment in pharmaceutical history, but its legacy is complicated by numerous factors that deserve attention.
It is imperative to consider that while ampicillin broadened antibiotic accessibility, its widespread and sometimes indiscriminate use contributed significantly to the burgeoning crisis of bacterial resistance we face today.
Moreover, the pharmaceutical industry's role in aggressively marketing such antibiotics without adequate cautionary measures amplified the problem.
This historical context must be scrutinized to understand that scientific triumphs come with nuanced consequences impacting public health policy and global well-being.
I look forward to a more comprehensive discussion that integrates these critical analyses.