Five years ago, Plaquenil exploded into the headlines for reasons that had nothing to do with its original purpose. But strip out the noise and you find a small white tablet that's been quietly supporting people with stubborn autoimmune diseases for decades. Maybe you’ve seen a friend open a distinctive bottle, or perhaps someone in your family depends on it just to get through the week when the aches make everything feel heavier. Behind this unassuming name, there’s more history, science, and controversy than you might expect.
How Plaquenil Works and Who Needs It
The active ingredient in Plaquenil is hydroxychloroquine. Developed back in the middle of the twentieth century, it started its career as a malaria treatment. If you ask older generations in Belfast, some might actually recall getting it before heading on travels to tropical climates. But over time, doctors noticed something fascinating: folks with rheumatoid arthritis and lupus, who had been prescribed Plaquenil, started feeling less pain and swelling. Joint movement got easier. Flare-ups were less frequent and less intense. Researchers dug deeper, and it turned out Plaquenil has anti-inflammatory effects that tamper down the immune system’s tendency to go haywire in certain people.
Fast forward, and you’ll find Plaquenil on repeat prescriptions for people with systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), and even chronic discoid lupus. It’s rarely the first thing a doctor tries, but when nothing else makes those grinding symptoms budge, Plaquenil can feel like a godsend. To be clear, it doesn't cure these conditions. But it does give people back some quality of life, often keeping things calm enough that they avoid those hospital admissions that hover in the background for anyone living with uncontrolled autoimmune flares.
What’s actually happening in the body? Hydroxychloroquine changes how immune cells talk to each other. It makes these chatty messengers – the cytokines – less likely to trigger the kind of full-blown attack on your own tissues. The result: less swelling, less pain, fewer fevers. It doesn’t work instantly. Most people need to take it for months before noticing the advantages. But for conditions where inflammation is like a slow-burning fuse, that slow-and-steady improvement is sometimes enough to change daily life in quiet but powerful ways.
Here’s a quick peek at who is actually taking Plaquenil right now, based on recent patient registry data:
| Condition | Use Cases | Percent on Plaquenil |
|---|---|---|
| SLE (Lupus) | Chronic joint and skin problems, kidney risk | ~70% |
| Rheumatoid Arthritis | Long-term swelling, joint pain | ~15% |
| Chronic Discoid Lupus | Severe rashes | ~40% |
But it’s not just about the usual suspects. In Belfast, some doctors now quietly add Plaquenil for rare off-label issues — things like sarcoidosis, porphyria cutanea tarda, and even certain forms of chronic urticaria. Sometimes, it feels a bit like a Swiss army knife in the autoimmune toolkit. Of course, every decision is weighed up: Is the benefit worth the potential risk?

Risks and Side Effects: Facts No One Wants to Ignore
The security blanket that Plaquenil offers isn’t without a few holes. If you ask ten people on it how they’re doing, you’ll get ten different stories — and not all of them are rosy. The side effects are usually pretty mild when you compare it to bigger-gun immunosuppressants, but some can be sneaky or downright nasty. By far, the one you hear about most is eye damage, or “retinopathy.” It doesn’t strike overnight, and it isn’t common if you stick to recommended doses. But Permanent loss of vision from Plaquenil can, in rare cases, happen if it’s taken at high doses for too many years. That’s why doctors in the UK and Ireland now insist on yearly eye tests for anyone clocking up more than five years on it. The screening isn’t just a formality. It’s vital.
- Common side effects: headaches, feeling sick, diarrhoea, rashes, stomach pain. Usually, these fade away after a few weeks.
- Serious but rare: retinopathy (eye changes), heart rhythm changes, blood cell problems, severe skin reactions.
The trick is not to quit at the first hurdle. For most people, any stomach upset can be dodged by taking Plaquenil with a proper meal (not just a slice of toast). Splitting the daily dose – say, 200mg in the morning, 200mg at night – can also help. If you ever notice a change in color vision, blurry patches, or visual “shadows,” it’s a red flag to get your eyes checked. Most people will never get anywhere near this. But better safe than sorry, right?
Here are some tips from folks who rely on Plaquenil every day:
- Pair it with food, not just a cuppa. Nausea drops off sharply.
- Keep it at the same time each day. Easy to remember, less likely to skip.
- Stick to all eye check reminders. Write them on your phone, fridge, wherever.
- If you’re on other meds (like methotrexate or steroids), keep the GP in the loop for possible drug overlaps.
- Don’t double up if you forget a dose—just wait ‘til the next one.
Around 1 in 10 people just can’t tolerate Plaquenil at all — either due to severe allergies, relentless stomach upsets, or ongoing vision worries. Luckily, there are alternatives (though each comes with its own baggage). Still, for the majority, Plaquenil remains the workhorse. In fact, during medicine shortages over the last few years — thanks partly to well-publicized but unsupported COVID ‘trials’ — rheumatologists in the UK fought to keep supplies prioritised for the people who genuinely need it. Patients with lupus or RA felt those shortages directly, and the lesson for most was clear: just because a drug gets attention for the wrong reasons, don’t throw out decades of proven benefit for those it was meant to help.
You’ll often hear stories of folks taking Plaquenil for 10, even 20 years, with barely a hiccup. But there’s a good reason every prescription pack comes with a warning leaflet and every year brings that ‘time for your vision test’ reminder. Balancing the good and the bad is the cornerstone. And don’t skip insurance notification — some plans now require proof of regular eye screening before refills.

Plaquenil in 2025: New Uses, Supply, and the Road Ahead
You might think the Plaquenil story is all written by now. Anyone following the news during the COVID-19 pandemic saw its name splashed across headlines for uses that were, to put it nicely, a bit off-label. The gold-standard trials – including one coordinated at the University of Oxford – found *no* benefit in reducing deaths or hospital time from COVID. Afterwards, not only did drug supplies tighten (putting lupus and arthritis patients at risk), but the public conversation also muddied what was once a straightforward medicine.
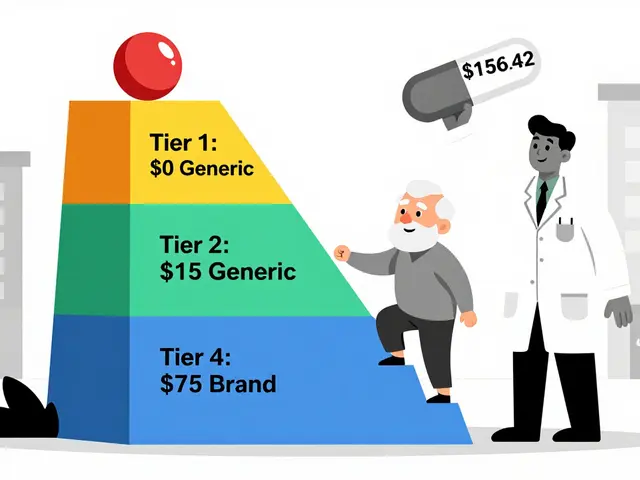
Now, in 2025, supplies in the UK and Ireland have stabilised. The NHS put in tight order systems, and pharmacies get monthly allocations based on actual patient needs. Counterfeit Plaquenil is a real risk if you look for it online, and people have ended up with pills that contain nothing, or worse — active ingredients that don’t belong there. The safest (and only) plan is the official pharmacy route.
What about research? Scientists are poking around new possible uses, though it’s a slow process. A big Irish study last year examined Plaquenil as an add-on for chronic fatigue linked to persistent Lyme disease, but no clear benefit turned up. In the skin world, especially for conditions like lichen planus and some stubborn photosensitive rashes, Plaquenil sometimes stands out when steroid creams fail and the patient just wants something that doesn’t cause weight gain or bone thinning.
Another angle: pregnancy. Rheumatologists and gynaecologists now agree it’s one of the few medicines you can actually keep for lupus and RA in pregnancy. The thinking used to be ‘stop everything, just in case,’ but decades of follow-up now show *continuing* Plaquenil may help prevent miscarriage and serious autoimmune flares. So, for young women especially, that oily green tablet could be the safest compromise going.
Here are a few practical takeaways for anyone newly starting out in 2025:
- Check your starting dose: Standard is 200mg once or twice daily. Don’t adjust unless told by your consultant.
- Eye screening: Baseline within the first year, then every 12 months after five years of continuous use.
- Stay within NHS supply networks. No deals, no online imports.
- If you plan to travel, order ahead. There have been unexpected regional shortages now and then, even in 2024-2025.
- Report any weird side effects, especially vision changes, straight away.
- If you stop, don’t just quit cold turkey. Always talk to your doctor about a safe plan, since sudden flares can be brutal.
The story of Plaquenil is hardly glamorous, but for people slogging through swollen mornings and exhausting fatigue, it’s a lifeline. Beyond the overblown headlines and supply hiccups, it’s still quietly doing its job in rheumatology clinics across Belfast and far beyond. The trick is knowing what it can do, watching for what it can’t, and staying on top of the tests that make safe, long-term use possible. That little white pill matters a lot more than most people realize.





Reynolds Boone
July 18, 2025 AT 16:30I've always been curious about the dual nature of Plaquenil. On one hand, it's praised for its effectiveness in treating autoimmune diseases like lupus and arthritis, but on the other, there's so much debate about its safety and side effects. Does anyone have personal experience with it? Like, how do you balance the benefits with the risks?
Also wondering if the demand stresses the supply chain, causing difficulties for those who truly need it. The article's mention of its persistent demand in 2025 makes me think the medical community must have found some solid middle ground on usage and safety.
Would love to hear from people who have been prescribed Plaquenil recently and how their doctors handled the risks involved!
Clarise Wheller
July 21, 2025 AT 22:10Thank you for sharing this! I think many people underestimate how crucial Plaquenil is for managing conditions like lupus and rheumatoid arthritis. From what I've seen, patients who stick with their prescribed regimens often report significant improvements.
But I totally get the concerns about safety. The side effects can be scary if they're not monitored properly. The article nicely breaks down why it remains popular despite that risk, which I appreciate because it helps foster understanding.
Does anyone know if there are new guidelines or protocols in 2025 that help minimize the side effects now?
Lexi Benson
July 24, 2025 AT 22:00Oh great, another drug that's both a lifesaver and a nightmare. Classic. Seriously, though, it's like people can’t make up their minds about Plaquenil. One day it’s a miracle cure, the next it’s the villain of the pharmaceutical world.
Honestly, with all the hype and demonizing, it’s no surprise the drug remains in high demand. People want what works, even if it comes wrapped in controversy. I’d be curious how it stacks up against newer meds out there in terms of side effects and efficacy.
Anyone seen recent studies? Or is it mostly anecdotal stuff floating around?
Tony Halstead
July 28, 2025 AT 12:53The intricate dance between therapeutic benefits and safety concerns with Plaquenil reveals much about the complexity of pharmacology in autoimmune diseases.
It is fascinating how this drug, despite its vintage status, continues to command significant attention in 2025; perhaps this underscores a lack of equally efficacious alternatives or the unique immunomodulatory characteristics it embodies.
Moreover, the balance of risk-benefit analysis in this context reminds me of the philosophical question: How much risk is acceptable in pursuit of relief and enhanced quality of life? Each patient's decision matrix varies, making shared doctor-patient discussions indispensable.
Would be interesting to explore if any novel formulations or adjunct therapies have emerged to mitigate risks further while preserving efficacy.
Kimberly Newell
August 1, 2025 AT 01:36i'm just glad there's still something out there that helps - dealing with autoimmune stuff is rough, y’all
plaque was a game changer for a family member of mine, but yeah, the side effects made everyone nervous, so lots of check ups and tests to keep an eye on things
does anyone know if they’ve made it any safer lately? or maybe have easier ways to monitor patients without so many blood tests? feels like that would help people stick to treatment better
Matt Laferty
August 7, 2025 AT 10:40Plaquenil’s enduring presence in the pharmacopeia is a testament to its profound utility, despite the layered challenges it presents.
In my experience, this drug walks a precarious tightrope between alleviating the burden of arthritis and lupus symptoms and the looming specter of adverse effects, some quite severe and insidious.
The clinical community continuously grapples with this dichotomy, enforcing stringent monitoring protocols to safeguard patients, which ingeniously balances risk without compromising therapeutic outcomes.
I do hope future iterations or adjunct therapies will alleviate these concerns, yet meanwhile, knowledge and vigilance remain our greatest allies.
Marsha Saminathan
August 10, 2025 AT 06:26It’s amazing how Plaquenil keeps showing up as a staple treatment, isn’t it? I feel like we often forget the emotional rollercoaster patients endure, balancing the hope it offers with the anxiety around potential side effects.
The constant demand just reflects how many folks are searching for relief, even if it's not a perfect solution. I really hope there’s more patient-centered research happening to make these meds less intimidating and more manageable for everyone.
Has anyone here had a moment when Plaquenil dramatically changed their quality of life? I bet those stories might inspire others navigating this tricky terrain.
Millsaps Mcquiston
August 13, 2025 AT 20:51Look, the cold hard truth is this drug has some serious side effects and risks, no sugarcoating it. But for many who have no other options, it’s not a choice but a necessity.
I've seen patients who swear by it, and others who had to quit because of complications. The ongoing demand is alarming though — are we risking too much because nobody wants to deal with the alternatives?
We need better, safer solutions, and faster. Meanwhile, doctors and patients alike have to keep a laser focus on monitoring and communication.
Damon Farnham
August 14, 2025 AT 21:33Honestly, why is this still a hot topic in 2025? Haven't we moved on from Plaquenil? It’s like the pharma industry loves to keep pushing old remedies while actual innovation gets pushed back.
Side effects or not, relying on this stuff is more like a bandage on a bullet wound. We need breakthroughs, not just recycled meds with a facelift.
Anyone else tired of this circus revolving endlessly around a few well-worn pills?
Justin Park
August 17, 2025 AT 05:06I find this whole discussion stimulating, especially because it evokes questions about the ethical balancing act within medicine — how does one prioritize when a drug like Plaquenil both heals and harms?
Is it simply the lesser evil in treating disabling diseases, or could we develop truly holistic treatments that bypass such compromises?
My curiosity extends to how regulatory bodies interpret ongoing demand in the shadow of risks — do they tighten restrictions or lean more into educating the public?
Overall, it’s a fascinating nexus of science, policy, and human experience.
Lexi Benson
August 17, 2025 AT 15:56@Damon Farnham Exactly my thoughts! It’s almost like people want to argue over the same meds every decade without pushing for anything better. Like, are we stuck in some pharmaceutical Groundhog Day?
Plus, Plaquenil's side effects are known but still telegraphed as if they're news. I get the controversy, but maybe focusing more on developing user-friendly monitoring tools or alternatives could make life better for patients.
Anyone else feel like the debates in these articles get stale but the patients don’t?