Every so often, a medication enters the spotlight not just for what it does, but for how it’s made and the controversy that shadows it. Premarin is a perfect example. Walk into any pharmacy in Belfast or beyond, and you’ll probably see a few boxes tucked away on the shelves, prescribed mainly to women facing the never-ending symptoms of menopause. Yet, ask ten people what Premarin actually is, and you’ll probably hear ten wildly different answers, some true, some complete fiction. Believe it or not, the story behind this drug is bigger than just hot flashes and night sweats.
What is Premarin and How Does It Work?
Premarin is a brand name for a type of estrogen therapy, and it stands out because it’s made from a really unique source—pregnant mares’ urine. Yes, as odd as that sounds, the name actually comes from Pregnant Mares’ urine. Pharmaceutical manufacturers collect urine from pregnant horses, process it, and create an estrogen mix, mostly conjugated equine estrogens. The US Food and Drug Administration (FDA) gave it a green light back in 1942, and it’s still among the most commonly prescribed medications for menopausal symptoms.
Women facing menopause often deal with an ugly list of symptoms—hot flashes, vaginal dryness, sleep problems, and even thinning bones. Estrogen levels drop during this time, which is what causes these issues. By giving the body more estrogen, Premarin helps reduce the severity of these symptoms, and there's pretty solid clinical evidence supporting that. Doctors also use it sometimes for treating certain ovarian disorders, and a rare form of prostate cancer in men.
What makes Premarin different from other hormone replacements is its unique mix of estrogens, mostly estrone sulfate and equilin sulfate, among a few others only found in horses. This chemical variety is part of why it works so well for many women—but also part of why it’s become a hot potato topic among doctors, researchers, and animal rights campaigners.
Now, if you’re curious about effectiveness, there’s a chunk of research out there. According to a study from the Women’s Health Initiative (WHI), women on Premarin experienced a reduction in bone fracture risk by over 30%. That’s a number you can’t ignore if osteoporosis is on your radar. The same study showed clear improvement in hot flashes—about 70% of women reported fewer and less intense episodes after three months of use. No magic, just science.
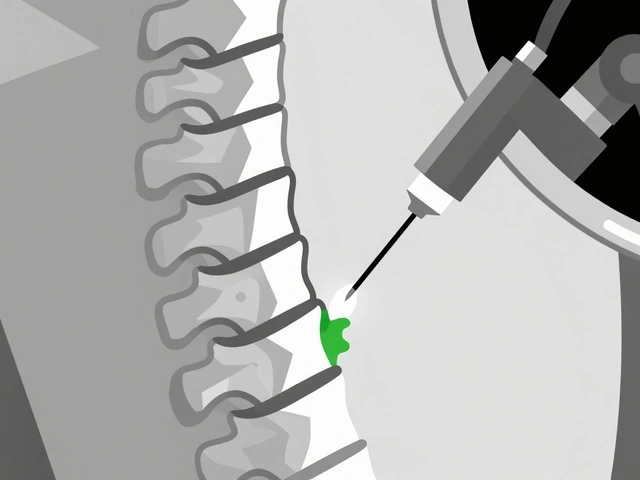
Let’s touch on how it’s taken. Premarin is usually in tablet form, but you’ll also find it as a cream (for vaginal symptoms), or an injection (for medical emergencies or specific conditions). Doses aren’t one-size-fits-all. Doctors usually start with the lowest possible amount and adjust depending on symptoms and how the patient feels.
In the UK and Ireland, Premarin is available by prescription only. The National Institute for Health and Care Excellence (NICE) outlines clear guidelines for who should use hormone therapy, and GP’s here will almost always carry out a personalised risk-benefit discussion first.
People often forget: Premarin isn’t just for women going through menopause naturally. It’s also prescribed after certain types of surgery, like removal of the ovaries or uterus, where natural estrogen levels drop off a cliff. It’s a lifeline for many to maintain their quality of life.

Benefits and Risks: What Does the Science Say?
No drug is perfect, and Premarin is definitely not an exception. Some women will tell you they wouldn’t have survived menopause without it. Others stopped after a month due to side effects. So, what does the actual data say?
First, let’s take a closer look at the positives. Besides easing hot flashes and vaginal dryness, studies have shown Premarin can help prevent osteoporosis-related fractures, as mentioned earlier. Women prescribed estrogen replacement after menopause typically see an increase in bone density within 12-18 months, according to research cited by the NHS. When used within the first few years after menopause starts, there’s evidence it might even have protective effects on heart health—though this is still a hot debate among experts.
There’s also evidence that Premarin can improve mood and help with sleep, though it’s not prescribed solely for those reasons. Some women feel more balanced, less irritable, and report better memory. It’s probably not a magic bullet for mental health, but the improvement in sleep and relief from constant hot flashes makes life a lot easier for many women.
Now, let’s talk side effects. The common stuff includes breast tenderness, bloating, nausea, and headaches, especially in the first few weeks. A small number will notice mild weight gain or changes in period patterns. Sometimes these ease off after your body adjusts, sometimes they don’t, and your GP may need to change your dose or try a different treatment.
The big risks make most people stop in their tracks: blood clots, stroke, certain types of cancer (like breast and endometrial), and heart disease. These risks aren’t the same for everyone. They shoot up if you’re over 60, have a family history of clotting, or combine Premarin with other medications or lifestyle habits like smoking. Because of this, doctors spend time weighing the risks for each person before prescribing it. That’s why you rarely see Premarin given without careful screening first.
| Condition | Estimated Increased Risk (%) | Population Studied | Notes |
|---|---|---|---|
| Blood Clot (DVT/PE) | 2-3x baseline | Women 50–59 | Greatest risk in first year of use |
| Stroke | 20% increase | Postmenopausal Women | Risk higher with age & dose |
| Breast Cancer (after 5 years) | ~25% increase | Long-term users | Data from WHI trial |
| Heart Attack | Neutral/No increase* | Women under 60 | *May be higher risk with age |
Those numbers don’t lie, but they don’t tell the whole story either. For example, the risk of breast cancer rises slightly after five years of continuous use, so most doctors suggest sticking to the smallest effective dose for the shortest possible time. If you have a uterus, using a progestin along with Premarin can help lower the risk of endometrial cancer, which is why combination HRT is often the way to go.
Here’s a practical tip: If you’re using the cream form for vaginal dryness, the risks are significantly lower compared to taking the pills, because less estrogen is absorbed into the bloodstream. So, for people worried about cancer or clot risks but desperate for relief, the cream is often a smart compromise. Always talk with your doctor about the safest options for your situation.
If you want to avoid side effects, make sure your lifestyle is on point—don’t smoke, check your blood pressure, get your cholesterol tested, and stay active. These changes reduce your risk no matter what medication you’re on.
One piece of advice many people overlook is regular follow-up. Have a review with your GP at least once a year if you’re on Premarin. Discuss any changes in your medical history, family history, or even new studies that come out. Hormone therapy isn’t a set-it-and-forget-it treatment—it’s a journey, and your needs will probably change over time.

The Debate: Animal Welfare, Ethics, and New Alternatives
If there’s a medicine that’s sparked lively debate, it’s Premarin. Not just because of side effects, but because of how it’s made. A lot of people still don’t know that farms in North America keep pregnant mares in stalls, collect their urine, and, after they give birth, sell or even slaughter the foals because they can’t all be used for breeding. This reality has pushed animal welfare groups to campaign hard against Premarin production. Some campaigns claim thousands of mares and foals are affected every year, though the drug’s manufacturers argue that standards have improved and facility oversight is stricter than ever. Still, for some, the ethical issues linger no matter what the official story is.
What does this mean for patients and doctors? Well, you’ve got choices. The last two decades have seen the rise of “synthetic” or plant-derived estrogens, like estradiol. These can be produced in a lab, don’t involve horses, and many work just as well for menopausal symptoms, though the chemical profile is a bit different. There’s still ongoing research into whether these newer forms have the same long-term safety data, but they’re becoming more common, especially for people who want to avoid animal-based products.
Here’s the twist: Some gynaecologists still reach for Premarin because, for some women, it simply works better, or they’ve had unwanted side effects from other hormone replacements. The combination of different estrogen molecules found in Premarin isn’t exactly replicated in non-horse versions, so some users genuinely feel the difference. Still, that doesn’t mean it’s the right choice for everyone.
Doctors today will often discuss the ethical and practical trade-offs with their patients. If animal welfare is your top priority, be straightforward about it with your GP—they should be able to suggest alternatives. If nothing else works, most people agree personal wellness and informed consent come first, but at least you’ll have made a choice with your eyes open.
The last thing to consider is cost and availability. In the UK, Premarin is covered under the NHS, but shortages do happen because production is centralised in a few North American facilities. Some women here have gone months without access, so it’s worth asking about back-up prescriptions if you rely on it for daily living.
To wrap it all up, knowledge is everything when it comes to Premarin. Whether you’re thinking about menopause management, caught in the middle of the debate over animal rights, or just trying to make the best health choice for yourself or someone you care about, the most important thing is information. Ask tough questions, dig deep, and don’t just accept the first answer on Google or from a friend. Real answers come from balancing science, ethics, and the reality of everyday life.




Alice Settineri
July 18, 2025 AT 16:30Wow, this article digs into some really juicy stuff about Premarin that I hadn’t considered before. I always thought it was just another hormone replacement therapy, but the controversy and how it’s actually made caught me off guard. Who knew the source of estrogens could stir such debate?
Also, the way the article breaks down myths is refreshing. Too often, discussions around menopause treatments get oversimplified, and voices get lost in the noise. I’m curious—does anyone have personal experiences with Premarin, either positive or negative?
I’d love to hear how it worked for you or if the side effects were as bad as some say. There are plenty of alternatives out there, but Premarin seems to have a complicated backstory worth knowing.
By the way, did you notice any surprising research findings in the article? For me, the new perspectives part really stood out. It’s always cool when science challenges what we thought was true!
Stanley Platt
July 18, 2025 AT 17:04Indeed, this article presents a salient, cogent overview of Premarin's multifaceted dimensions. The historical context coupled with contemporary scientific data provides a comprehensive framework for understanding both clinical efficacy and ethical considerations.
From a medical standpoint, it is imperative to weigh the nuanced risks and benefits that have emerged from longitudinal studies, particularly those examining hormone replacement therapies in diverse patient populations.
This piece notably delineates these aspects with a commendable degree of thoroughness. I encourage readers to approach Premarin’s utility with an informed mind, considering individual health profiles and emerging alternatives in the pharmacological sphere.
An interesting point for further discourse might be how healthcare providers can better communicate the complexities surrounding Premarin to patients, fostering a more transparent shared decision-making process.
Herman Rochelle
July 18, 2025 AT 17:37I've been coaching clients through menopause, and this piece does a good job laying out Premarin's pros and cons. It’s helpful to clear up some of the misconceptions I've encountered, especially about risks that are often overstated.
I always emphasize personalized care, and this article really drives home that point—what might work wonders for one person could be problematic for another. Balancing symptom relief with potential side effects is a tricky task.
One tip I'd add is for patients to keep a detailed symptom diary when starting any hormone therapy. That way, adjustments can be more accurately made by their healthcare providers. Equipping patients with knowledge and action items is key to better outcomes.
It’s refreshing to see a resource that respects the complexity of menopause treatments rather than painting everything with the same brush.
Katheryn Cochrane
July 18, 2025 AT 18:10nathaniel stewart
July 18, 2025 AT 18:44This article does touch on many layers of what Premarin entails, though I do find the debates surrounding it to be somewhat fatigued by repetition over the years. Still, it’s vital to stay informed and to revisit data as new findings emerge.
I found a small typo that might distract some readers—nothing critical but attention to such details would improve clarity. Despite that, it’s encouraging to see such articles challenge myths with evidence rather than fear-mongering.
The side effects discussed are real, but in my experience, many patients tolerate the therapy quite well when monitored closely. I'd urge ongoing dialogue between patients and doctors.
Any thoughts on how insurance coverage affects Premarin accessibility? It’s an angle not always considered but important for patient care.
Pathan Jahidkhan
July 18, 2025 AT 19:34Ah, Premarin, the elixir of changing seasons for womankind! Yet, within this ambrosial tincture lurks a Pandora’s box of controversies and whispered doubts. One wonders if the alchemy of science has outpaced our collective wisdom.
The article intriguingly exposes the paradox: a remedy derived from the mare’s urine, a factual yet poetic origin that stirs both wonder and skepticism.
Is it science serving humanity’s soft needs or the inexorable march of pharmaceutical interests shaping our destinies? These questions linger like shadows in a labyrinth.
Perhaps we must embrace a dialectic approach—questioning not merely with eyes, but with the spirit. Such a treatment embodies both hope and hesitation. What say you, fellows of this discourse?
Dustin Hardage
July 18, 2025 AT 20:07The thoroughness of this guide on Premarin is commendable, providing a balanced view of its pharmacodynamics and patient implications. The consideration of biochemical pathways is particularly useful for understanding potential side effects at a mechanistic level.
However, it would be prudent for future discussions to incorporate more recent randomized control trials to better contextualize risks such as thromboembolic events and breast cancer in current patient cohorts.
Furthermore, the ethical debates over equine derivatives highlight the need for continued innovation in alternative hormone synthesis. Such advancements could alleviate both medical and animal welfare concerns.
Clinicians should remain vigilant, staying abreast of emerging data and tailoring treatments to optimize safety and efficacy.
Leslie Woods
July 18, 2025 AT 20:40This guide raised a lot of questions for me about Premarin's long-term use. I’m curious if the article mentioned anything about recommended duration for therapy and how patients can monitor for side effects without feeling overwhelmed.
As someone who often researches health topics, I appreciate the balanced tone, but I do wonder if there are newer, less invasive alternatives that aren’t discussed as much. Are they truly safer or just not as well studied yet?
It would be great to have some patient stories or firsthand accounts included next time. Sometimes personal experiences help put the clinical information into perspective.
Dipak Pawar
July 18, 2025 AT 21:14Intriguing article indeed; the pharmacological paradigm of equivocal hormone therapies like Premarin persists globally, yet deserves relentless scrutiny.
The biochemical nomenclature, coupled with the socio-medical narratives elucidated herein, reflect a nuanced spectrum of ideological and clinical controversies manifest from the drug’s derivation and application.
Integral to this discourse is a critical assessment of comparative studies vis-à-vis bioidentical hormones, synthetic alternatives, and the ingress of ethnopharmacological practices in menopausal management across diverse cultures.
Could the article have benefited from integrating cross-cultural epidemiological data to enrich contextual understanding? I posit yes.
Jonathan Alvarenga
July 18, 2025 AT 21:47Honestly, I find a lot of the hype about Premarin to be overblown. The article feels like it’s beating a dead horse, rehashing the same controversies that have been around forever without offering much new insight.
There’s definitely a dark side with side effects and the ethical issues, but the narrative often ignores that many women have found real relief through this drug. It’s not some miracle cure, but neither is it the devil everyone likes to paint it as.
Plus, some of the so-called 'myths' the article tackles are obviously rooted in legit concerns and should not be dismissed so easily. I guess we keep circling back to this because there’s no one-size-fits-all answer.
Anyone else feels like the debates drown out the actual patient voices sometimes?
Jim McDermott
July 18, 2025 AT 22:20I found the exploration of the manufacturing process particularly illuminating. It’s unsettling to realize how the extraction of conjugated estrogens from pregnant mares’ urine raises significant ethical and environmental concerns.
This understanding adds a layer of complexity when choosing treatments because it’s not only about efficacy or side effects but also about the origins of the medication.
Has there been any advocacy or movement towards more sustainable or synthetic alternatives that align better with animal welfare principles? Would love to hear if anyone has insights or personal experiences with such options.
Ultimately, discerning patients should have access to transparent information like this to make the best choices for their health and values.
Naomi Ho
July 18, 2025 AT 22:54Thanks for sharing this detailed guide; it's really helped me understand the complexities of Premarin as a menopause treatment. It’s clear there are some serious side effects to watch out for, but also it can be effective when used carefully.
What I wonder though is about the monitoring process—what kind of screening or follow-up tests do patients usually need if they choose Premarin? I didn’t see much on that in the article.
Also, it’d be interesting to know more about interactions with other meds common among menopausal women, like antidepressants or blood thinners.
Has anyone here had experience managing that kind of thing while on Premarin? Any tips or advice?