SGLT2 Inhibitor Bone Risk Assessment Tool
Assess Your Fracture Risk
This tool estimates your fracture risk based on the latest clinical data for SGLT2 inhibitors. Enter your details to see if your current medication is appropriate for your bone health profile.
When you’re managing type 2 diabetes, the goal isn’t just lowering blood sugar-it’s protecting your heart, kidneys, and overall quality of life. SGLT2 inhibitors like canagliflozin, empagliflozin, and dapagliflozin have become go-to options because they do all three. But one question keeps popping up in doctor’s offices and patient forums: Do these drugs increase your risk of breaking a bone?
Why Bone Health Matters with Diabetes Drugs
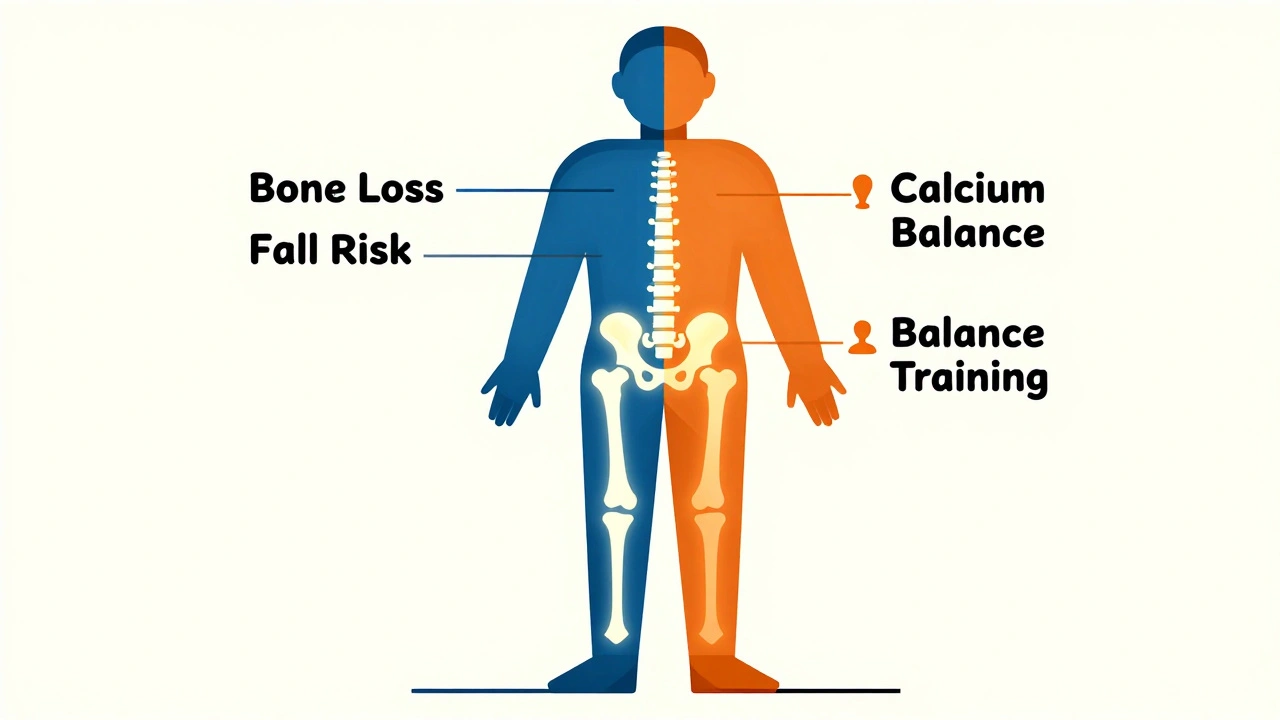
People with type 2 diabetes already have a higher chance of fractures-even if their bones look normal on a scan. High blood sugar weakens bone structure over time. Add in older age, reduced muscle mass, and nerve damage that affects balance, and falls become more likely. So when a new class of diabetes meds came out in 2013, it made sense to watch for side effects that could make things worse.Canagliflozin (Invokana) was the first to raise red flags. In 2015, data from the CANVAS trial showed people taking it had about 26% more fractures than those on placebo. Most of these weren’t from car crashes or sports injuries-they happened when someone just stumbled while standing up or stepped off a curb. The FDA responded in 2016 by adding a warning to the label. It wasn’t just about the drug itself-it was about who was taking it. Many of those affected were older adults with low bone density or a history of falls.
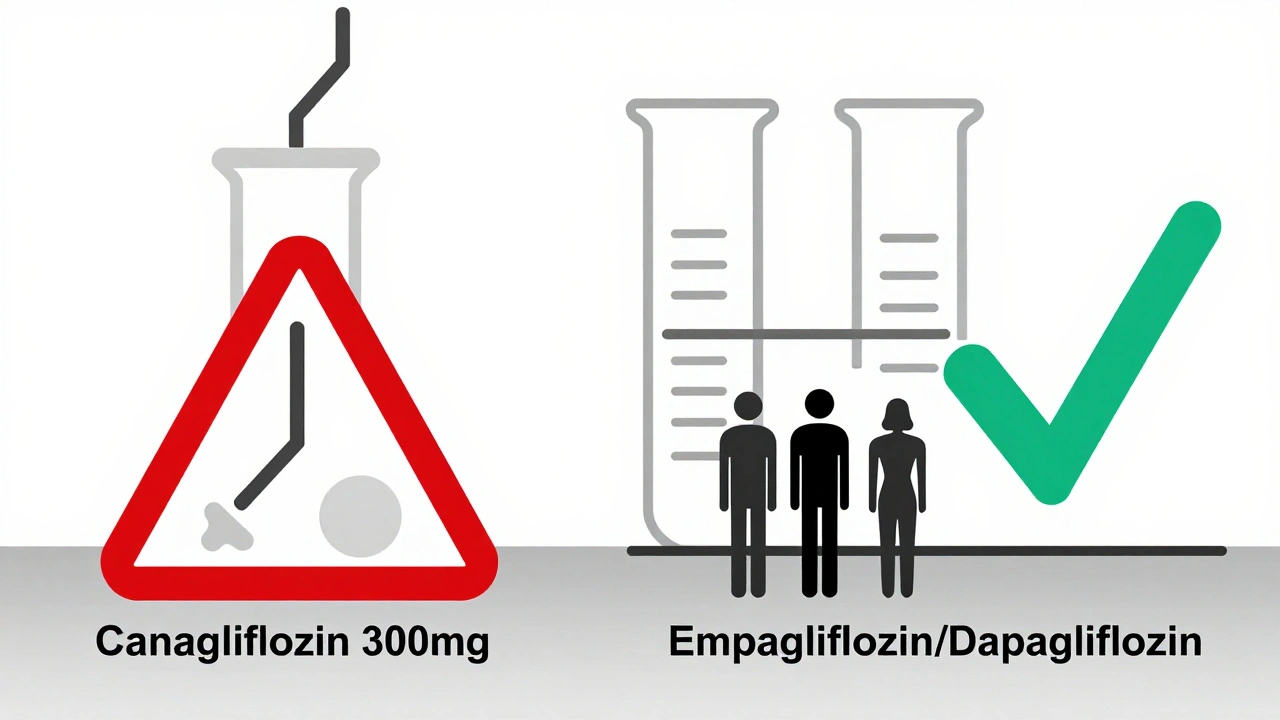
Not All SGLT2 Inhibitors Are the Same
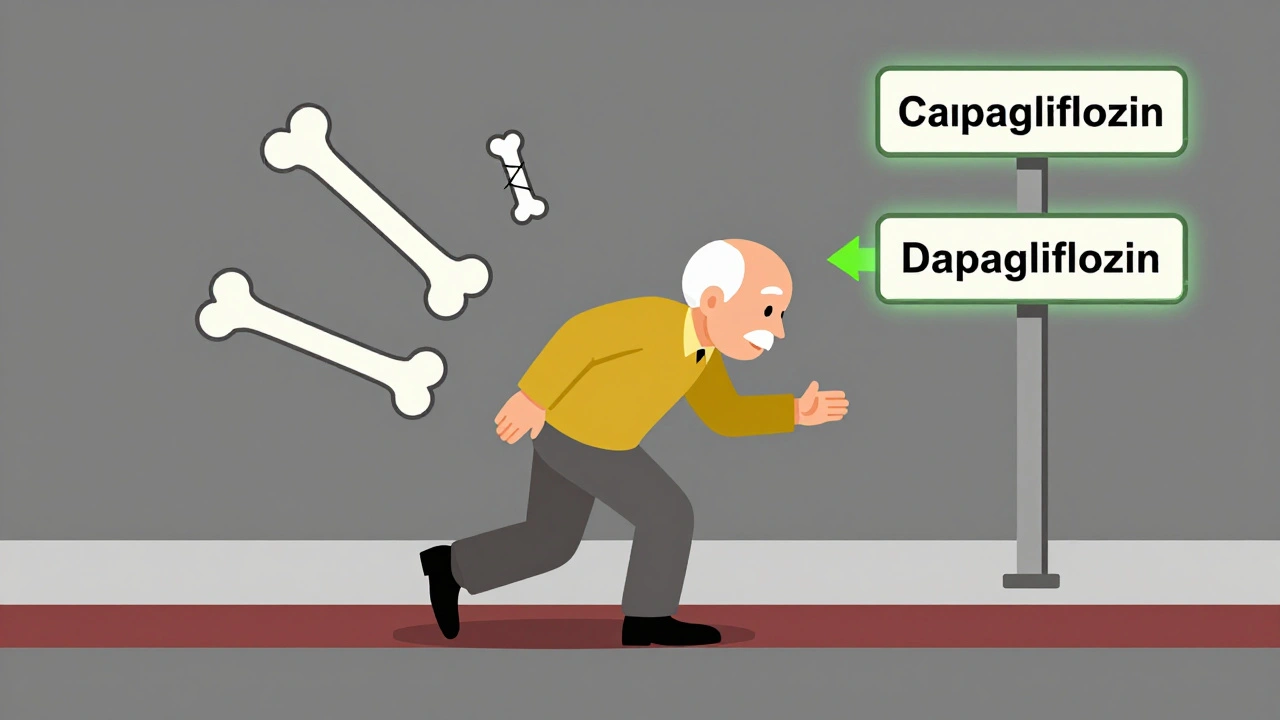
This is where things get important. The problem isn’t the whole class. It’s mostly canagliflozin, especially at the higher 300 mg dose. Studies on empagliflozin (Jardiance) and dapagliflozin (Farxiga) haven’t shown the same risk. In fact, a 2023 meta-analysis of 27 trials involving over 20,000 patients found no overall increase in fractures with SGLT2 inhibitors as a group. The pooled risk? Almost exactly the same as placebo.Why the difference? It comes down to how each drug affects the body. Canagliflozin causes more significant bone mineral density loss-about 1% at the hip and spine over two years, compared to less than half that with empagliflozin. It also lowers estradiol levels in women by nearly 10%, which can weaken bones. It increases phosphate loss in urine, which triggers hormonal shifts that may pull calcium out of bones. And while all SGLT2 inhibitors can cause dizziness from low blood pressure, canagliflozin seems to do it a bit more often, raising fall risk.
Empagliflozin and dapagliflozin don’t show these same patterns. In head-to-head comparisons, their bone effects are either neutral or barely noticeable. That’s why the FDA only updated the label for canagliflozin-and why guidelines from the American Diabetes Association and American Association of Clinical Endocrinologists treat them differently.
Who Should Be Worried?
If you’re a healthy 55-year-old with type 2 diabetes and no history of falls or broken bones, the risk from any SGLT2 inhibitor is likely very low. But if you’re older, have osteoporosis (T-score below -2.5), have had a fracture before, or take steroids or thyroid medicine, you need to think harder.Here’s what endocrinologists are doing in practice:
- Checking bone density (DXA scan) before starting canagliflozin in anyone over 65 or with known bone loss
- Avoiding canagliflozin entirely in people with T-scores below -2.0
- Choosing empagliflozin or dapagliflozin instead for patients with high fracture risk
- Adding calcium and vitamin D if levels are low
- Encouraging balance exercises and removing fall hazards at home
A 2022 survey of 347 endocrinologists found that 82% avoid canagliflozin in patients with osteoporosis. Only 34% do the same for dapagliflozin. That’s not paranoia-it’s precision.
What the Real-World Data Shows
Some doctors worry the clinical trials didn’t last long enough to catch slow bone damage. Dr. Robert Heaney, a leading bone expert, points out that most trials ran only 3-5 years. Bone loss happens over decades. But real-world data is starting to catch up.A 2023 study in the Journal of Parathyroid Disease looked at over 100,000 Medicare patients on SGLT2 inhibitors. It found no link between empagliflozin or dapagliflozin and fractures. Even for canagliflozin, the risk was only elevated in those over 75 with prior fractures. In younger, healthier people, the numbers were nearly identical to other diabetes drugs.
And here’s something surprising: SGLT2 inhibitors might actually be safer than some other diabetes meds. A 2023 study in JAMA Network Open compared fracture rates between SGLT2 inhibitors and GLP-1 agonists like semaglutide. The SGLT2 group had slightly fewer fractures-by about 0.3 per 100 person-years. That’s because GLP-1 drugs cause more nausea and dizziness early on, which can lead to falls.
What to Do If You’re on One of These Drugs
If you’re already taking canagliflozin and haven’t had any issues, don’t panic. But do this:- Ask your doctor if you’ve had a bone density scan in the last two years
- Review your fall history-have you tripped or fallen in the past year?
- Check your vitamin D level. Most people with diabetes are deficient.
- Consider switching to empagliflozin or dapagliflozin if you’re over 70, have osteoporosis, or have had a fracture
- Start balance training-simple things like standing on one foot for 30 seconds, twice a day, can reduce fall risk by up to 40%
Don’t stop your medication without talking to your doctor. The heart and kidney benefits of these drugs are real and life-saving. But you don’t have to accept a higher fracture risk if there’s a safer alternative.
The Bottom Line
SGLT2 inhibitors aren’t all created equal. Canagliflozin carries a small but real increased risk of fractures, especially in older adults with weak bones. Empagliflozin and dapagliflozin do not. The evidence now strongly supports choosing the latter for patients at risk of falls or osteoporosis. For most people, the benefits of these drugs far outweigh the risks-but only if you pick the right one.Diabetes treatment isn’t one-size-fits-all. Your bone health matters as much as your A1c. Ask the right questions. Get the right tests. And make sure your medication fits your whole body-not just your blood sugar.





Declan O Reilly
December 2, 2025 AT 17:50Man, I read this whole thing and just thought - we’re treating diabetes like it’s a spreadsheet when it’s a living, breathing mess of hormones, falls, and midnight snacks. SGLT2s are cool, but no drug fixes a house full of loose rugs and a cat that chases your slippers. Bone density scans? Sure. But also, maybe just teach people to stand on one foot while brushing their teeth. Free, effective, and you won’t need a PhD to do it.
Conor Forde
December 3, 2025 AT 14:49Ohhhh here we go. Another ‘canagliflozin is evil’ panic dressed up as science. Let me guess - the same people who think statins cause impotence and flu shots give you autism are now terrified of a drug that saves kidneys. The FDA warning? A PR stunt. Look at the actual numbers: 26% increase? That’s like saying eating toast increases your risk of being struck by lightning. Meanwhile, empagliflozin gets a free pass because it’s ‘nicer’? Please. It’s all about who funded the trial. #BigPharmaLies
patrick sui
December 5, 2025 AT 01:01Big picture: SGLT2i = net positive for most. But the nuance here is critical. Bone loss isn’t just about BMD - it’s about muscle strength, balance, and vitamin D. I’ve seen patients on dapagliflozin with T-scores of -3.2 who never fell once because they did tai chi 3x/week and took 2000 IU D3 daily. The drug isn’t the villain - the lack of holistic care is. Also, if your doctor hasn’t checked your 25-OH vitamin D in the last year, find a new one. 🙏
Priyam Tomar
December 6, 2025 AT 20:40Everyone’s acting like this is new info. I’ve been telling people since 2016: canagliflozin is a bone crusher. The data’s been there. What’s new is that now even the ADA admits it. But you know what’s worse? Doctors still prescribing it to 70-year-old ladies who can’t get out of a chair without holding onto furniture. If you’re over 65 and your bones are already whispering, don’t be the guy who says ‘I trust my doctor.’ Check your own T-score. Or don’t. But don’t blame me when you break your hip.
Jack Arscott
December 8, 2025 AT 20:35Just switched from cana to jardiance last month. No more dizziness, no more falls. Also my A1c dropped 0.4. 🤩 Life’s good. Don’t panic, just pivot. And maybe get a cane if you’re 70+ and your cat still scares you. 😅
Irving Steinberg
December 10, 2025 AT 03:21So basically if you’re old and broke you shouldn’t take canagliflozin but if you’re young and healthy its fine cool so what about the people in the middle like me who just want to live without being told to do yoga and buy a new pair of shoes every 3 months also why is everyone acting like this is a revelation i’ve been on farxiga for 2 years and my bones are fine
Lydia Zhang
December 10, 2025 AT 23:41Interesting. I’m on canagliflozin. Haven’t fallen. Haven’t broken anything. My doctor didn’t mention any of this. Guess I’m lucky.
Kay Lam
December 11, 2025 AT 16:50I think what’s really missing here is the emotional weight of being told you’re too old, too fragile, too at-risk - and then being handed a pill that’s supposed to save your life but comes with a warning label that feels like a death sentence. It’s not just about bone density scans or vitamin D - it’s about dignity. When you’re 72 and you’ve lived through three divorces and two kids moving away and your knees click like a metronome, the last thing you need is to be treated like a statistic. Maybe the real solution isn’t switching drugs - it’s switching how we talk to people. You don’t need a DXA scan to know you’re worth protecting.
Matt Dean
December 13, 2025 AT 14:14Let me get this straight - you’re telling me the same class of drugs has wildly different effects based on which molecule you pick? And nobody thought to test this before approving them all as ‘interchangeable’? This is why I hate pharma. They don’t care about biology - they care about patents. Canagliflozin was the first. So they got the big label. Then they slapped the same marketing on the others and called it ‘class effect.’ Bullshit. This is why we need real independent research - not industry-funded fluff.
Walker Alvey
December 14, 2025 AT 22:39Wow. So the answer to ‘do these drugs break bones’ is… it depends on which one you take, who you are, and whether your doctor is awake? And we call this medicine? I guess that’s why they pay you $400k a year to sit in a lab and say ‘it’s complicated.’ Meanwhile, I’m just trying to survive my 5th diabetic neuropathy foot ulcer. But hey - at least my A1c is 6.8. Progress, right? 😏
Adrian Barnes
December 15, 2025 AT 04:21While the clinical data presented is methodologically sound and statistically significant, it remains insufficiently contextualized within the broader framework of longitudinal musculoskeletal physiology. The absence of longitudinal biomarker tracking - specifically, serum CTX and P1NP levels - renders the fracture risk assessment inherently incomplete. Furthermore, the reliance on self-reported fall history introduces significant selection bias, particularly in geriatric cohorts with cognitive decline. Until prospective, multicenter trials with dual-energy X-ray absorptiometry (DXA) at 6-month intervals are conducted, any clinical recommendation remains speculative.
Michelle Smyth
December 16, 2025 AT 15:12It’s fascinating how we’ve turned a physiological phenomenon into a moral panic. Canagliflozin’s bone effects? A textbook example of off-target pharmacodynamics. But let’s be honest - the real issue isn’t the drug. It’s that we’ve outsourced patient agency to algorithmic guidelines. If you’re over 65 and your doctor didn’t ask you about your balance, your grip strength, or whether you still climb stairs without holding the railing… you’re not being treated. You’re being categorized. And that’s the real fracture.
Linda Migdal
December 17, 2025 AT 03:49Look - I don’t care what the FDA says or what some Irish guy on Reddit thinks. In America, we don’t let big pharma scare us off life-saving meds. If you’re scared of falling, get a walker. If you’re scared of bone loss, take calcium. Don’t let some overpriced journal tell you to stop taking a drug that keeps your heart from exploding just because you might trip on your rug. We’ve got better things to worry about than whether your hip is 1% less dense. Stay strong, America.