GLP-1 Agonist Gallbladder Risk Checker
Assess Your Gallbladder Risk
This tool estimates your risk of developing gallbladder issues while taking GLP-1 agonists based on key factors identified in medical research.
When you start a GLP-1 agonist like Ozempic or Wegovy for weight loss or diabetes, the goal is clear: lose weight, feel better, lower blood sugar. But for some, a new kind of pain shows up-sharp, persistent, and often after eating. This isn’t just indigestion. It could be your gallbladder screaming for help.
Why GLP-1 Agonists Affect Your Gallbladder
GLP-1 agonists work by slowing down digestion. That’s why you feel full longer and eat less. But that same effect hits your gallbladder too. Normally, when you eat fat, your body releases a hormone called cholecystokinin. That tells your gallbladder to squeeze and dump bile into your intestine to help digest it. GLP-1 drugs block that signal. The gallbladder doesn’t contract. Bile sits there, thickens, and over time, turns into sludge-and then stones.
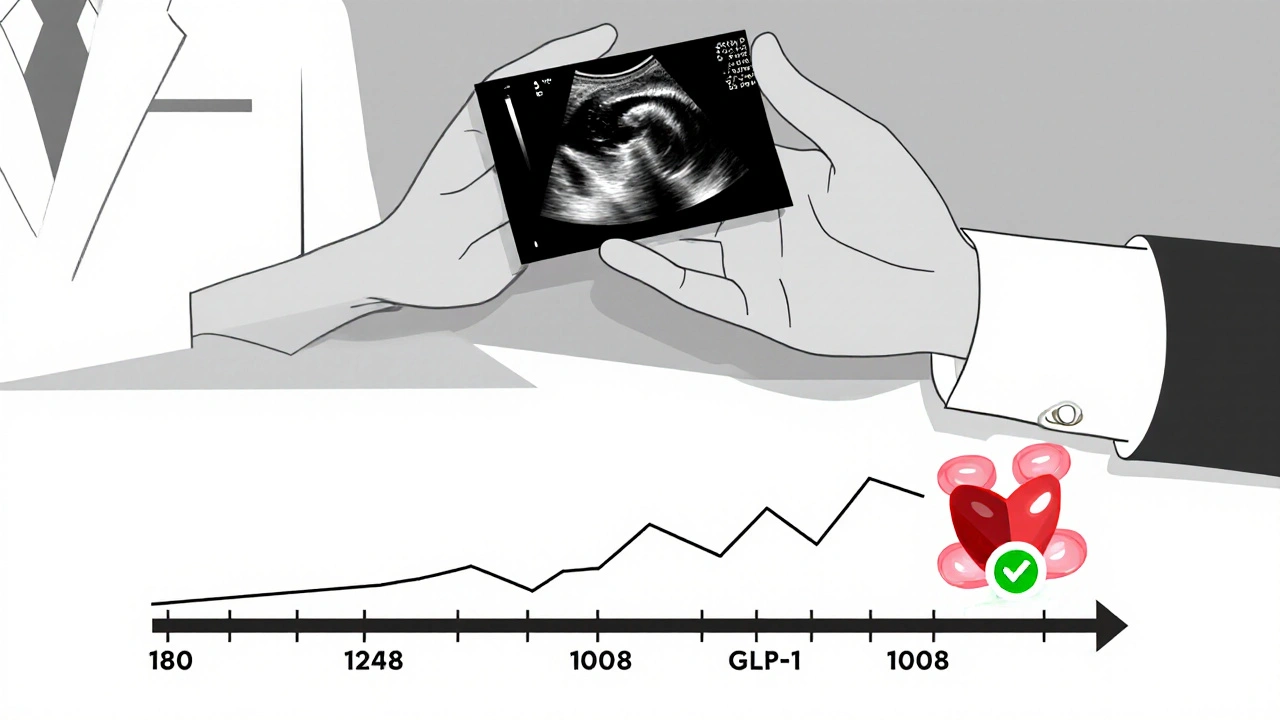
This isn’t a rare side effect. A major 2022 study in JAMA Internal Medicine looked at 56,000 people across 76 trials and found a 37% higher risk of gallbladder problems with GLP-1 drugs. The risk jumps even higher for people using higher doses for weight loss. Liraglutide (Victoza, Saxenda) and semaglutide (Ozempic, Wegovy) carry the biggest risk. Exenatide (Byetta, Bydureon) has a much lower association.
Who’s Most at Risk?
Not everyone on these drugs will get gallstones. But certain people are far more likely to. If you’re a woman over 40, have a BMI over 30, or lost weight quickly-more than 1.5 kg per week-you’re in the danger zone. So is anyone who’s had gallstones before. The data shows rapid weight loss can make existing stones move and block ducts, increasing the chance of infection or inflammation by over four times.
Even more concerning: people who’ve already had their gallbladder removed have almost no risk. That’s because the problem isn’t the drug itself-it’s the gallbladder’s inability to empty properly. No gallbladder? No problem.
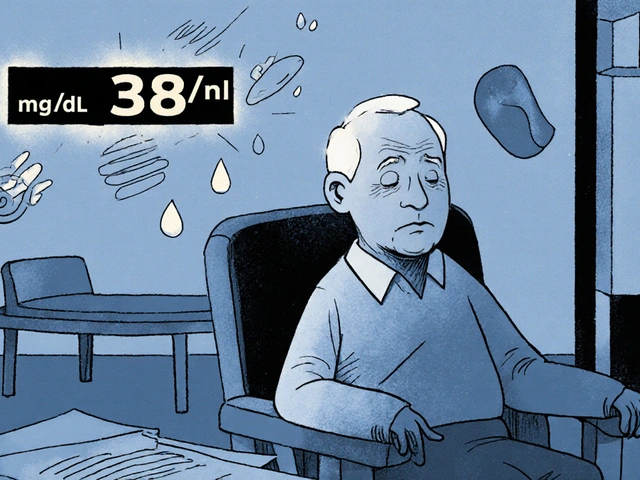
Abdominal Pain Red Flags: What to Watch For
Not all belly pain is serious. But with GLP-1 drugs, certain pain patterns are warning signs you can’t ignore:
- Right upper quadrant pain-that’s the area just under your ribs on the right side. If it lasts more than 30 minutes, especially after eating, it’s a red flag. Studies show this symptom is 89% sensitive for cholecystitis.
- Pain radiating to your right shoulder-this is classic. It happens because the inflamed gallbladder irritates nerves that also serve the shoulder. This sign has 82% specificity.
- Pain after fatty meals-tacos, fried chicken, cheese, butter. If you notice the pain always shows up after these foods, that’s 94% specific for biliary issues.
- Nausea or vomiting with the pain-this isn’t just a bad stomach. It’s your body’s alarm system. The likelihood ratio jumps to 3.8 when this happens together with RUQ pain.
One patient on Reddit wrote: “Started Wegovy six months ago. Lost 30 pounds. Then ate tacos. Three hours later, I was curled up on the floor. ER said gallstones. They took my gallbladder out the next day.” That story isn’t rare. In one patient forum analysis, 11.4% of users reported abdominal pain, and nearly 4% described pain patterns matching biliary colic.

When It Gets Serious
Most gallbladder issues from GLP-1 drugs start between 3 and 9 months after starting the medication. The median time to symptoms? 180 days. And once pain hits, it often escalates fast. In the Woronow case series, 72% of patients needed hospitalization within 72 hours of their first pain. About 75% of those cases ended in surgery-cholecystectomy. That’s removal of the gallbladder. It’s not a minor procedure. Recovery takes weeks. You’ll need to adjust your diet for life.
And here’s the kicker: these events are underreported. The FDA received 1,842 gallbladder-related reports for GLP-1 drugs in 2023-up from 581 in 2021. That’s a 217% jump. But experts believe only 1 in 10 actual cases get reported. So the real number could be much higher.
What Doctors Should Do
The American Association of Clinical Endocrinology recommends a baseline ultrasound for anyone starting a GLP-1 agonist if they have risk factors: female, over 40, BMI >30, rapid weight loss, or past gallstones. It’s a simple, non-invasive test. If stones are already there, the drug might be a bad idea-or at least needs close monitoring.
Doctors should also talk to patients before they start. Not just about nausea or constipation. Talk about gallbladder pain. Give them the red flags. Tell them: “If you get sharp pain under your ribs after eating fat, don’t wait. Get checked.”
And if pain shows up? Stop the drug. Get an ultrasound. Don’t assume it’s just a stomach bug. Delaying diagnosis increases the risk of infection, abscesses, or even pancreatitis.
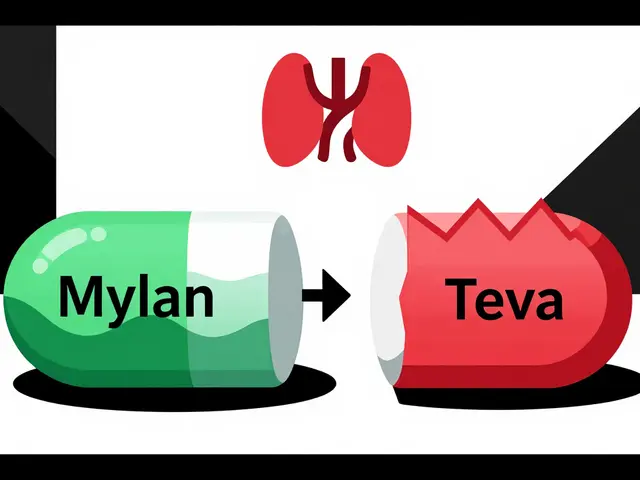
What About Other Weight Loss Drugs?
Not all weight loss medications carry this risk. Orlistat (Xenical) can cause oily stools and gastrointestinal upset, but it doesn’t slow gallbladder emptying. Phentermine-topiramate (Qsymia) has no known link to gallbladder disease. So if you have a history of gallstones or are at high risk, these might be safer alternatives-though they come with their own trade-offs.
The Bigger Picture
GLP-1 agonists are powerful. They reduce heart attacks, strokes, and death in people with diabetes. For many, they’re life-changing. But that doesn’t mean the risks are negligible. As prescriptions for weight loss explode-from 1.2 million in late 2021 to over 6.8 million by late 2023-the number of gallbladder complications will rise too.
Right now, 12.7% of new cholecystectomy patients in 2023 had been on GLP-1 drugs for at least 3 months. That’s up from just 3.2% in 2021. This isn’t a fluke. It’s a growing clinical trend.
Researchers are now testing whether adding ursodeoxycholic acid (UDCA)-a bile acid that helps dissolve stones-can prevent complications. Early trials are underway. But for now, prevention is simple: know the signs, get screened if you’re high-risk, and act fast if pain hits.
What You Can Do Today
- If you’re on a GLP-1 agonist and have risk factors, ask your doctor about a baseline ultrasound.
- Learn the red flags: RUQ pain, shoulder radiation, fatty food triggers, nausea.
- If pain hits, don’t wait. Get an ultrasound. Don’t push through it.
- If you’ve had your gallbladder removed, your risk is minimal-but still mention your meds to your doctor.
- If you’re considering starting one, talk about your gallbladder history. It matters.
These drugs are not magic. They’re powerful tools with real trade-offs. Understanding the risks doesn’t mean avoiding them. It means using them wisely-with your eyes open.



Alex Rose
October 28, 2025 AT 21:59GLP-1 agonists induce cholestasis via CCK suppression, leading to biliary stasis and subsequent lithogenesis. The JAMA Internal Medicine meta-analysis demonstrates a statistically significant RR of 1.37 (95% CI: 1.21–1.55) for cholecystitis and cholelithiasis, particularly with semaglutide dosing >1.0 mg/week. This is not anecdotal-it’s pharmacokinetic inevitability.
Robert Burruss
October 29, 2025 AT 12:23I’ve been thinking about this a lot lately. It’s not just about the drug-it’s about how we treat weight loss like a hack, not a physiological overhaul. We slap on a medication, expect the body to adapt instantly, then act shocked when it rebels. The gallbladder isn’t broken. It’s just been ignored. Maybe we need to ask: why are we forcing our biology into a mold that doesn’t fit?
I’m not saying don’t use these drugs. I’m saying don’t use them like they’re candy. There’s a difference between healing and hijacking.
And honestly? The fact that so many people are getting their gallbladders removed after starting these meds… it’s like we’re treating symptoms as if they’re the enemy. But the body’s screaming for a different approach.
What if the real problem isn’t the gallbladder? What if it’s the speed? The pressure? The cultural obsession with rapid transformation?
I’ve seen people lose 40 pounds in six months and call it a win. But then they’re in the ER three months later. Is that a win? Or just a delay of consequences?
We need to stop glorifying the crash diet mentality-even when it’s wrapped in a prescription bottle.
Maybe the real miracle isn’t the drug. Maybe it’s patience.
And if you’ve had your gallbladder out? You’re not immune. You’re just… different. Your liver now has to compensate. And that’s a whole other burden.
It’s not just about pain. It’s about what we’re willing to sacrifice for a number on a scale.
And we’re not talking about it enough.
Vasudha Menia
October 30, 2025 AT 05:35Oh my goodness, this post gave me chills 😭 I started Ozempic last year and had exactly that taco-induced pain-right under my ribs, like someone was squeezing my insides! I thought it was just gas… until I couldn’t breathe. Thank you for sharing the red flags!! I got my ultrasound and they found 3 stones. Surgery next week. I’m so glad I didn’t ignore it 💙 You saved me from a disaster!
Bryan Heathcote
November 1, 2025 AT 01:08Wait, so if you’ve had your gallbladder removed, you’re basically immune? That’s wild. So the drug isn’t the villain-it’s the organ’s inability to respond. That flips the whole narrative. So maybe the real risk factor isn’t the drug, it’s having a gallbladder at all? 😮
Has anyone looked at bile acid composition changes with long-term GLP-1 use? I’m curious if the bile becomes more lithogenic over time, or if it’s purely stasis.
Snehal Ranjan
November 2, 2025 AT 23:27It is indeed a matter of profound clinical significance that the mechanism of action of GLP-1 agonists interferes with the physiological coordination between digestion and gallbladder motility. The data presented here is compelling and aligns with emerging evidence from Asian populations where biliary disease incidence is rising in parallel with increased GLP-1 prescription rates. I recommend that all healthcare providers in high-risk demographics initiate pre-treatment imaging as standard of care. Prevention is always superior to intervention.
Sabrina Aida
November 3, 2025 AT 03:57So let me get this straight… we’re being told to fear a drug that helps people lose weight and live longer… because sometimes, their gallbladder doesn’t like it? That’s like saying ‘don’t drive cars because sometimes people get whiplash.’ This is the kind of fearmongering that makes people distrust medicine. If you’re going to scare people, at least admit that 95% of users never have a problem.
Also, who funded this study? Pharma? The gallbladder surgeons’ union? Someone’s making money off this panic.
Alanah Marie Cam
November 3, 2025 AT 16:55Thank you for this comprehensive and clinically grounded overview. As a healthcare professional, I appreciate the emphasis on patient education and early intervention. It is critical that individuals on GLP-1 agonists understand the warning signs and are empowered to seek timely care. A simple ultrasound can prevent major surgical intervention and complications. I will be incorporating this guidance into my patient counseling protocols immediately.
prajesh kumar
November 4, 2025 AT 05:29Bro this is life-saving info. I’ve been on Wegovy for 8 months, lost 45 lbs, no issues… but now I’m scared to eat pizza again 😅 I’m booking my ultrasound this week. Better safe than sorry. Thank you for making this so clear. You’re a real one.
Dylan Kane
November 5, 2025 AT 06:55Oh wow, another ‘GLP-1 is dangerous’ article. Let me guess-this was written by a surgeon who’s getting paid per cholecystectomy? Or maybe a diet coach trying to scare people back to kale salads? The data shows these drugs reduce cardiovascular death by 26%. One in ten people get gallstones? So what? That’s less than smoking, less than obesity, less than sitting all day. This is fear porn dressed as medicine.
KC Liu
November 6, 2025 AT 18:281,842 reports to the FDA? That’s a drop in the bucket. You know what’s not reported? The 12 million people who are on these drugs and never had an issue. You know what else isn’t reported? The fact that the FDA’s database is filled with reports from people who ate a greasy burrito and blamed the drug. This is all part of a coordinated campaign to undermine GLP-1 drugs-probably by the keto influencers and Big Gallbladder lobby. They’re scared their $300/month ‘detox’ programs are obsolete.
And why is the author so fixated on ultrasound? Are they pushing a diagnostic equipment company? Just saying…
Shanice Alethia
November 7, 2025 AT 04:01Let’s be real-this isn’t about gallbladders. This is about control. The medical establishment doesn’t want you to lose weight on a pill. They want you to suffer. They want you to eat ‘clean.’ They want you to pay for therapy, supplements, and monthly coaching. This article? It’s a distraction. A smokescreen. Because if you can just take a pill and lose weight… then what’s their business model? 😏
And don’t even get me started on ‘baseline ultrasound.’ That’s a $500 cash grab. You think your doctor really cares? No. They just want to cover their ass. You’re being played.
Do you really think they’d let you take a drug that causes gallstones if it wasn’t profitable? Wake up.