When HIV was first identified in the 1980s, a diagnosis often meant a death sentence. People didn’t just fear the virus-they feared the stigma, the uncertainty, and the daily grind of pills that didn’t always work. Today, that reality has changed. HIV is no longer a death sentence. It’s a manageable condition. And for many, it’s now something you treat with just two injections a year.
How HIV Treatment Has Changed Since 1996
In 1996, the first combination antiretroviral therapy (ART) hit the market. It was a breakthrough, but it came with a heavy cost: up to 20 pills a day, side effects like nausea and nerve damage, and the constant pressure to never miss a dose. One missed pill could let the virus bounce back. For years, that was the norm.
Then came better drugs. By the 2010s, single-pill regimens became standard. Biktarvy, approved in 2018, combined three powerful drugs into one tiny tablet-smaller than a dime and weighing less than half a gram. It worked. It was simple. And for many, it was life-changing.
But even that wasn’t perfect. People still had to remember pills every day. Travel, mental health struggles, or just plain fatigue could derail adherence. And when adherence drops, so does viral suppression. That’s where the real revolution began.
The Rise of Long-Acting Therapies
In 2022, lenacapavir (brand name Sunlenca) became the first capsid inhibitor approved for HIV treatment. Unlike older drugs that target enzymes inside the virus, lenacapavir attacks the virus’s outer shell-the capsid-that holds its genetic material together. It’s like smashing the virus’s protective bubble before it even gets a chance to replicate.
The biggest win? One injection lasts six months.
By January 2025, that single drug got even better. The FDA granted Breakthrough Therapy Designation to a new combo: lenacapavir plus two broadly neutralizing antibodies, teropavimab and zinlirvimab. Together, they form the LTZ regimen-a potential twice-yearly treatment that’s already showing 98.7% viral suppression in clinical trials. That’s higher than daily pills.
And it’s not just treatment. In June 2025, the same drug, now called Yeztugo, was approved for HIV prevention. For people at high risk, two shots a year can reduce infection risk by nearly 100%. The WHO called it “the next best thing to an HIV vaccine.”
How It Compares to Other Treatments
Before LTZ, the closest option was cabotegravir (Apretude), an injectable PrEP given every two months. That meant six visits a year. LTZ cuts that to two.
Here’s how the main options stack up:
| Treatment | Dosing Frequency | Form | Viral Suppression Rate | Key Advantage |
|---|---|---|---|---|
| Biktarvy | Daily | Oral pill | 97.2% | Single tablet, low side effects |
| Cabotegravir (Apretude) | Every 2 months | Injection | 95.8% | Injectable alternative to pills |
| Lenacapavir (Sunlenca) | Every 6 months | Injection | 96.5% | First capsid inhibitor |
| LTZ Regimen (investigational) | Every 6 months | Two injections | 98.7% | Higher suppression, lower injection reactions |
| Yeztugo | Every 6 months | Injection | N/A (for prevention) | Prevents HIV infection |
LTZ doesn’t just work better-it’s better tolerated. Only 12.3% of users reported injection-site reactions, compared to 28.6% with cabotegravir. And 89% of people on LTZ said they felt confident about sticking to their treatment. For daily pill users? Just 63%.

Quality of Life: More Than Just Viral Load
People with HIV aren’t just counting viral copies. They’re counting anxiety, shame, and the weight of daily reminders that they’re different.
One Reddit user, u/HIVWarrior2020, wrote after a year on Sunlenca: “After 12 years of daily pills, the twice-yearly injection has eliminated my treatment-related anxiety completely.” That’s not just a quote-it’s a pattern. The Positive Peers app, used by over 150,000 people with HIV, found that 92% of those on long-acting therapies rated their satisfaction as 8/10 or higher. For daily pill users? Only 76%.
Why? Because treatment isn’t just about health. It’s about freedom. No more hiding pills in your purse. No more panic when you’re away from home. No more explaining to coworkers why you’re always late for lunch.
Injection-site pain? Yes, it happens. About 28% report mild swelling or soreness for a couple of days. But 94% of those people say it’s worth it. “I’d rather have two days of soreness than 365 days of worry,” said one user in a 2025 survey.
Cost and Access: The Big Hurdle
There’s a catch.
Biktarvy costs about $69,000 a year in the U.S. Yeztugo? $45,000. That’s not just expensive-it’s unjust. UNAIDS reported in September 2025 that generic versions could be made for as little as $25 per person per year. That’s one-thousandth of the current price.
Right now, only 17% of U.S. clinics could offer Sunlenca because it needs to be stored at -20°C. By June 2025, after Yeztugo’s approval with a more stable formula, that number jumped to 43%. But in sub-Saharan Africa, less than 2% of people have access to long-acting therapies. Why? No cold chain. No trained staff. No funding.
The WHO’s July 2025 guidelines tried to fix this. They now recommend community health workers-local nurses, volunteers, even trained barbers-administer injections in villages and clinics. It’s simple. It’s scalable. And it’s the only way this breakthrough reaches the people who need it most.
What’s Next? The Future of HIV Care
The LTZ regimen is still under review. Full FDA approval is expected in Q2 2026. But even before then, the writing is on the wall: the future of HIV care is long-acting, injectable, and patient-centered.
Companies like ViiV Healthcare and Merck are racing to catch up. ViiV’s VH-184 and VH-499 look promising, but they don’t match the six-month dosing of lenacapavir. Merck’s doravirine-islatravir combo is a daily two-pill option-better than 20 pills, but still daily.
And while researchers are testing potential cures-like combining antibodies with drugs that wake up dormant virus-those are still years away. For now, the goal isn’t a cure. It’s control. And with LTZ, we’re closer than ever.
By 2030, experts predict 75% of people with HIV in high-income countries will be on long-acting regimens. In low-income countries? Maybe 40%-if the world finally decides that a $25 pill should be as accessible as a $45,000 one.
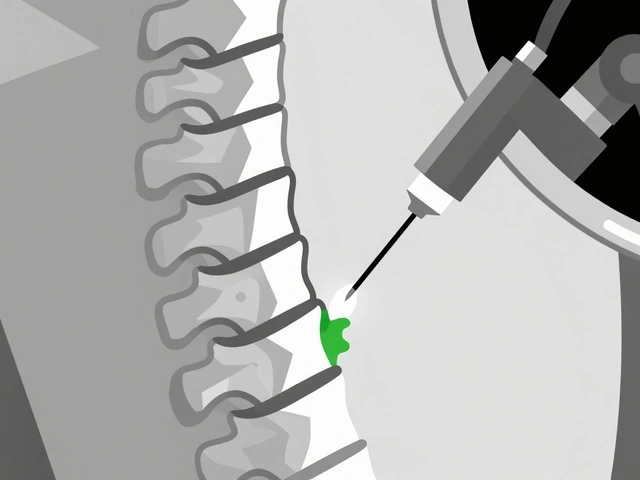
How to Get Started
If you’re living with HIV and thinking about switching:
- Ask your provider if you’re eligible. You need to be virally suppressed for at least 6 months.
- Expect a 4-week overlap with your current pills. This keeps the virus suppressed while your body adjusts.
- Find a clinic that stocks the drug. Storage is tricky-some places still can’t handle the cold chain.
- Plan your injections. Set calendar reminders. Many clinics now use automated text alerts-ask if yours does.
- Track your experience. Use apps like Positive Peers to share how you’re feeling. Your feedback helps others.
And if you’re not HIV-positive but at risk? Talk to your doctor about Yeztugo. Two shots a year could keep you safe. And if you’re in a country where it’s not available yet, push for it. Demand matters.
Final Thoughts
HIV isn’t gone. But it’s no longer the monster it once was. We have tools now that can stop transmission, keep people healthy, and give them back their dignity.
The science is here. The data is clear. The question isn’t whether we can do better-it’s whether we will.
Can you still transmit HIV if you’re on long-acting treatment?
No-not if your viral load is undetectable. Whether you’re on daily pills or twice-yearly injections, consistent treatment that keeps your viral load below 200 copies/mL means you cannot transmit HIV sexually. This is called U=U (Undetectable = Untransmittable), and it’s backed by decades of research.
Are long-acting HIV treatments safe for pregnant women?
Data is still limited, but early studies show lenacapavir is safe in pregnancy. The CDC recommends continuing treatment during pregnancy to prevent mother-to-child transmission. If you’re pregnant and considering a switch, talk to your OB-GYN and HIV specialist. They’ll weigh the benefits of reduced dosing against the need for proven safety data.
What if I miss my injection?
If you miss your injection by a few weeks, your provider may give you a backup oral regimen to prevent viral rebound. Missing by more than two months risks the virus coming back. That’s why clinics now use automated reminders. Some even offer home visits for patients who can’t travel.
Can I switch back to pills if I don’t like injections?
Yes. Switching from long-acting to oral therapy is common and safe. Your provider will guide you through a transition period, usually 4-6 weeks, to ensure your viral load stays suppressed. Many people switch back due to injection discomfort or access issues-not because the treatment failed.
Is there a generic version of lenacapavir yet?
Not yet. Patents protect lenacapavir until at least 2032. But the $25-per-year cost projection from the EATG report in October 2025 shows it’s technically possible. Generic manufacturers are already preparing. If global health agencies push for licensing agreements, affordable versions could appear in low-income countries as early as 2028.
How do I know if I’m a good candidate for long-acting therapy?
You’re likely a good fit if: you’re virally suppressed, you struggle with daily pills, you have mental health challenges that affect adherence, or you want to reduce stigma. Providers also consider your injection tolerance and access to clinics. If you’re unsure, ask for a trial run-some clinics offer a single injection to test comfort before switching fully.
People with HIV aren’t waiting for miracles anymore. They’re living full lives-with fewer pills, fewer visits, and more peace of mind. The tools are here. Now it’s up to us to make sure no one is left behind.




Paul Ong
January 2, 2026 AT 20:34Andy Heinlein
January 4, 2026 AT 15:36gerard najera
January 4, 2026 AT 23:20Stephen Gikuma
January 5, 2026 AT 20:00Bobby Collins
January 7, 2026 AT 09:22Layla Anna
January 9, 2026 AT 00:43Heather Josey
January 10, 2026 AT 16:59Donna Peplinskie
January 11, 2026 AT 03:56Olukayode Oguntulu
January 12, 2026 AT 00:12Bill Medley
January 12, 2026 AT 16:01Richard Thomas
January 12, 2026 AT 18:04Dusty Weeks
January 14, 2026 AT 10:58Sally Denham-Vaughan
January 15, 2026 AT 04:24