When a vertebra in your spine cracks from osteoporosis, trauma, or cancer, the pain can be unbearable. Standing, sitting, even breathing becomes a struggle. For many, traditional treatments like painkillers, braces, and rest don’t cut it. That’s where kyphoplasty and vertebroplasty come in - two minimally invasive procedures that can turn agony into relief in a matter of hours.
What Exactly Are Kyphoplasty and Vertebroplasty?
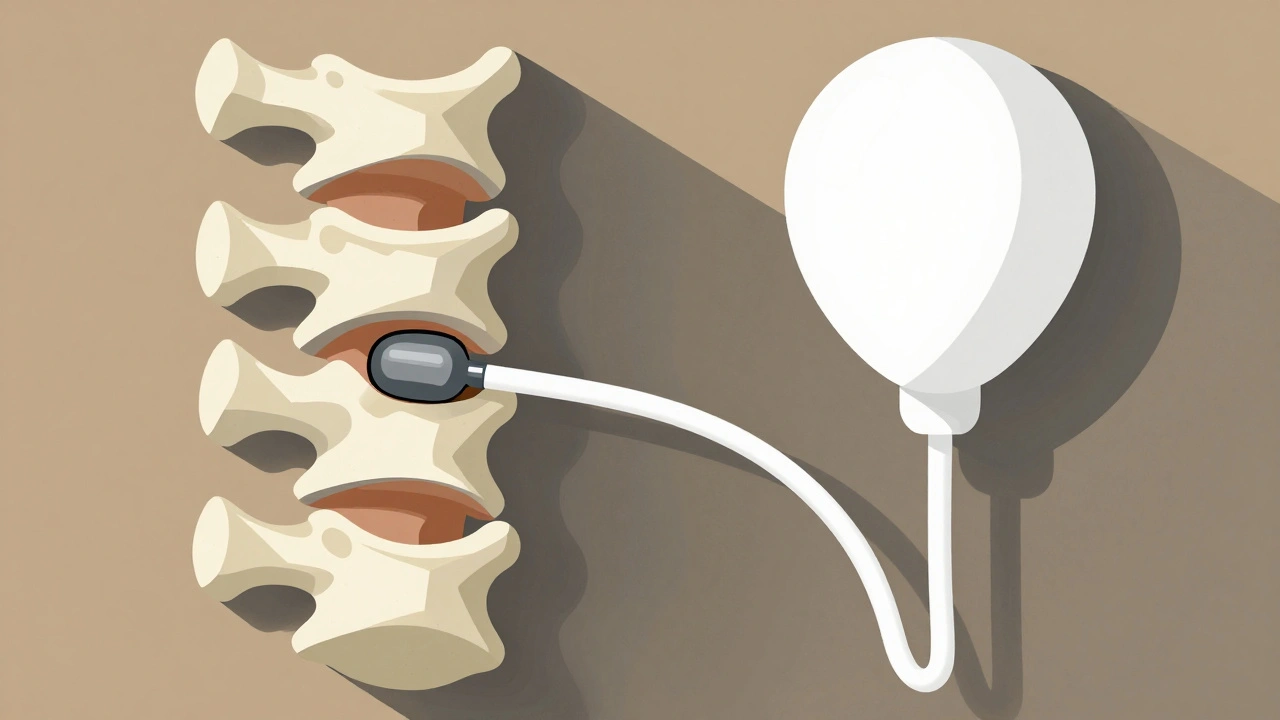
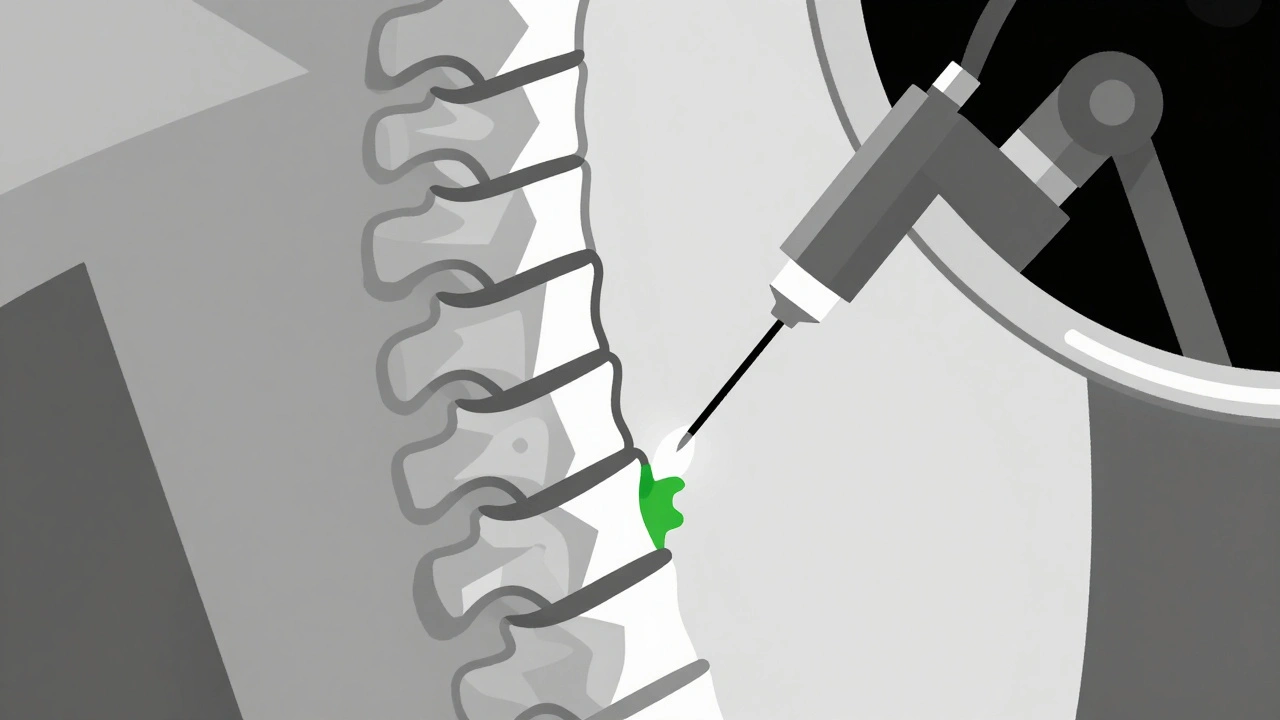
Both procedures are designed to fix broken vertebrae, especially those crushed by osteoporosis. They’re not open surgery. No big cuts. No long hospital stays. Instead, a tiny needle goes through your skin, guided by real-time X-ray imaging, and delivers medical-grade bone cement into the fractured bone. The cement hardens in under 20 minutes, acting like an internal cast that stabilizes the break. The big difference? Kyphoplasty adds a balloon step. Before injecting cement, a small balloon is inserted into the broken vertebra and gently inflated. This lifts the collapsed bone back toward its original height, creating a cavity. Then, the balloon is popped, and cement is pumped in. Vertebroplasty skips the balloon. Cement goes straight in under pressure. Kyphoplasty was developed in the late 1990s as an upgrade to vertebroplasty, which started in France in the 1980s. Today, about 100,000 of these procedures are done each year in the U.S. alone, with kyphoplasty making up roughly two-thirds of them.How They Work: Step by Step
You’ll lie face down on an operating table. Local anesthesia numbs the area, and you’ll get sedation so you’re relaxed but awake. A thin needle is inserted through your back, right into the fractured vertebra. Fluoroscopy - a kind of live X-ray - guides every move. For vertebroplasty: Once the needle is in place, liquid PMMA (polymethylmethacrylate) cement is injected under pressure. It flows into the cracks and porous spaces inside the bone, locking everything in place. The whole thing takes 30 to 60 minutes. For kyphoplasty: After the needle goes in, one or two balloon tamp devices are threaded in. They’re slowly inflated with saline to lift the crushed bone. You might feel a bit of pressure, but not pain. Once the bone is restored as much as possible, the balloons are deflated and removed. Then, cement is injected into the space the balloons left behind. This step adds about 15 minutes to the procedure. In both cases, the cement hardens fast. Most people feel pain relief within hours. Many go home the same day.Which One Is Better? The Real Differences
Let’s cut through the marketing. Both procedures give you about the same pain relief - 85% to 90% of patients report a dramatic drop in pain within 24 hours. Your VAS pain score might drop from an 8 out of 10 to a 1 or 2. But here’s where they diverge:- Height restoration: Kyphoplasty can restore 40% to 60% of lost vertebral height. Vertebroplasty? Almost none. That’s why kyphoplasty is often chosen if you’ve developed a noticeable hunchback (kyphosis).
- Cement leakage: In vertebroplasty, cement leaks out of the bone in 27% to 68% of cases. Most leaks are harmless, but in about 1.1% of cases, it causes serious problems like nerve damage or lung issues. Kyphoplasty reduces that risk to 9% to 33% because the balloon creates a clean cavity for the cement to fill.
- Cost: Kyphoplasty costs about 20% to 30% more. Medicare pays around $3,850 for kyphoplasty versus $2,950 for vertebroplasty. That difference matters in a healthcare system where every dollar counts.
- Long-term height loss: Even though kyphoplasty lifts the bone, studies show that over time - after 500 cycles of normal body weight stress - about 30% of that height gain is lost. So while it looks better on an X-ray right after surgery, the long-term structural benefit isn’t as clear-cut as once thought.
Who Gets Which Procedure?
It’s not one-size-fits-all. Your doctor will look at your X-rays, MRI, and how your fracture looks. Go for kyphoplasty if:- Your vertebra is collapsed by more than 30%
- You have visible spinal curvature (kyphosis)
- You’re concerned about cement leakage risk
- You’re younger, active, and want the best possible spinal alignment
- Your fracture is stable, with little height loss
- You’re older, with multiple fractures, and cost is a bigger concern
- Your main goal is pain relief, not posture correction
What Do Patients Actually Say?
Real people, real experiences. On Healthgrades, kyphoplasty has a 4.6/5 rating. Vertebroplasty sits at 4.4/5. Both are highly rated. One patient on Reddit wrote: "Kyphoplasty felt like flipping a switch. I went from 9/10 pain to 2/10 in hours. I stood up without wincing the next morning." Another, who had vertebroplasty: "The pain dropped from constant 7/10 to occasional 3/10. But my hunchback? Still there." About 10% to 15% of patients say their pain didn’t fully go away. And in 5% to 10% of cases, a new fracture appears in a nearby vertebra within a year. That’s not because the procedure caused it - it’s because osteoporosis keeps weakening the spine. That’s why treating the root cause matters just as much as fixing the break.Recovery and Aftercare
You’ll be monitored for 4 to 6 hours after the procedure. Most people walk the same day. You’ll be told to avoid heavy lifting or twisting for the first week. Normal activities? Usually back within 72 hours. You’ll likely stop using opioid painkillers within a week. Studies show 75% of patients quit them entirely after these procedures. But here’s the catch: the fracture is fixed, but your bones are still weak. Without treating osteoporosis, you’re at high risk for another fracture. That means calcium, vitamin D, and often medications like bisphosphonates or denosumab. Your doctor will refer you to a bone specialist - you can’t skip this part.Who Performs These Procedures?
Interventional radiologists and orthopedic spine surgeons are the main providers. Both need special training. The Society of Interventional Radiology says you need at least 15 to 20 supervised cases to be proficient. Kyphoplasty’s learning curve is a bit steeper - about 25 cases to get it right - because of the balloon manipulation. The procedure isn’t for everyone. It’s not used for old, healed fractures. Your MRI must show bone marrow edema - meaning the fracture is fresh, less than 6 weeks old. If it’s been months, these procedures won’t help.




Christian Landry
December 8, 2025 AT 07:09Katherine Chan
December 9, 2025 AT 23:01Katie Harrison
December 11, 2025 AT 18:59Mona Schmidt
December 12, 2025 AT 13:36Guylaine Lapointe
December 13, 2025 AT 17:46William Umstattd
December 15, 2025 AT 12:19Ajit Kumar Singh
December 15, 2025 AT 14:07Larry Lieberman
December 16, 2025 AT 01:37Sabrina Thurn
December 16, 2025 AT 21:09Simran Chettiar
December 18, 2025 AT 12:17Anna Roh
December 19, 2025 AT 00:50Gilbert Lacasandile
December 20, 2025 AT 14:14