Methadone CYP Interaction Risk Checker
This tool helps clinicians and patients assess the risk of dangerous QT prolongation when taking methadone with other medications. Enter the patient's methadone dose and check for interactions with common CYP inhibitors and other risk factors.
Risk Assessment Results
When someone starts methadone for opioid use disorder, they’re often told it’s safe, effective, and once-daily. But behind that simplicity is a hidden danger: methadone can quietly stretch the heart’s electrical cycle, raising the risk of a deadly arrhythmia called torsade de pointes. And it doesn’t happen because of the dose alone. It happens because of what else the patient is taking.
Why Methadone Is Different
Methadone isn’t like other opioids. While drugs like oxycodone or buprenorphine mainly act on opioid receptors, methadone also blocks the hERG potassium channels in heart cells. This slows down the heart’s recovery phase after each beat, which shows up on an ECG as a prolonged QT interval. That’s not just a number-it’s a warning sign. When the QT interval goes beyond 500 milliseconds, the risk of sudden cardiac death jumps fourfold. The problem? Methadone’s effects aren’t linear. Some people on 60 mg a day have dangerous QT prolongation. Others on 200 mg never do. Why? Because metabolism matters more than dose.How CYP Enzymes Control Methadone Levels
Your liver uses enzymes called cytochrome P450 (CYP) to break down methadone. The big players are CYP3A4 and CYP2B6. If these enzymes are slowed down, methadone builds up in your blood. Even a small increase-say, 30%-can push serum levels into the danger zone. Common medications can do this. Fluoxetine (Prozac), clarithromycin (Biaxin), fluconazole (Diflucan), and valproate (Depakote) are all CYP3A4 or CYP2B6 inhibitors. A 2007 JAMA Internal Medicine study found that nearly 30% of methadone patients had QTc intervals over 460 ms-far above the safe limit. Of those, 12% were taking fluoxetine. Another 6% were on clarithromycin or fluconazole. These aren’t rare cases. They’re predictable. Even more dangerous? Ritonavir. It’s in Paxlovid, the COVID-19 antiviral. Ritonavir is one of the strongest CYP3A4 inhibitors known. If someone on methadone takes Paxlovid, their methadone levels can spike by 50% or more. That’s not theoretical. Emergency departments have seen cases of cardiac arrest after this combo.QT Prolongation Isn’t Just About Dose
Doctors used to think: “If the dose is under 100 mg, we’re safe.” That’s outdated. The 2023 American Society of Addiction Medicine guidelines now recommend ECG monitoring for anyone on more than 50 mg per day. Why? Because studies show QT prolongation can happen even at low doses-if there’s a CYP interaction, low potassium, or liver disease. And potassium? It’s critical. Low potassium (hypokalemia) makes the heart even more sensitive to methadone’s effects. A patient on methadone with a normal QT interval might be fine-until they get the flu, stop eating, and their potassium drops. One day, their ECG shows 510 ms. They collapse. They didn’t overdose. Their heart just couldn’t handle the combo.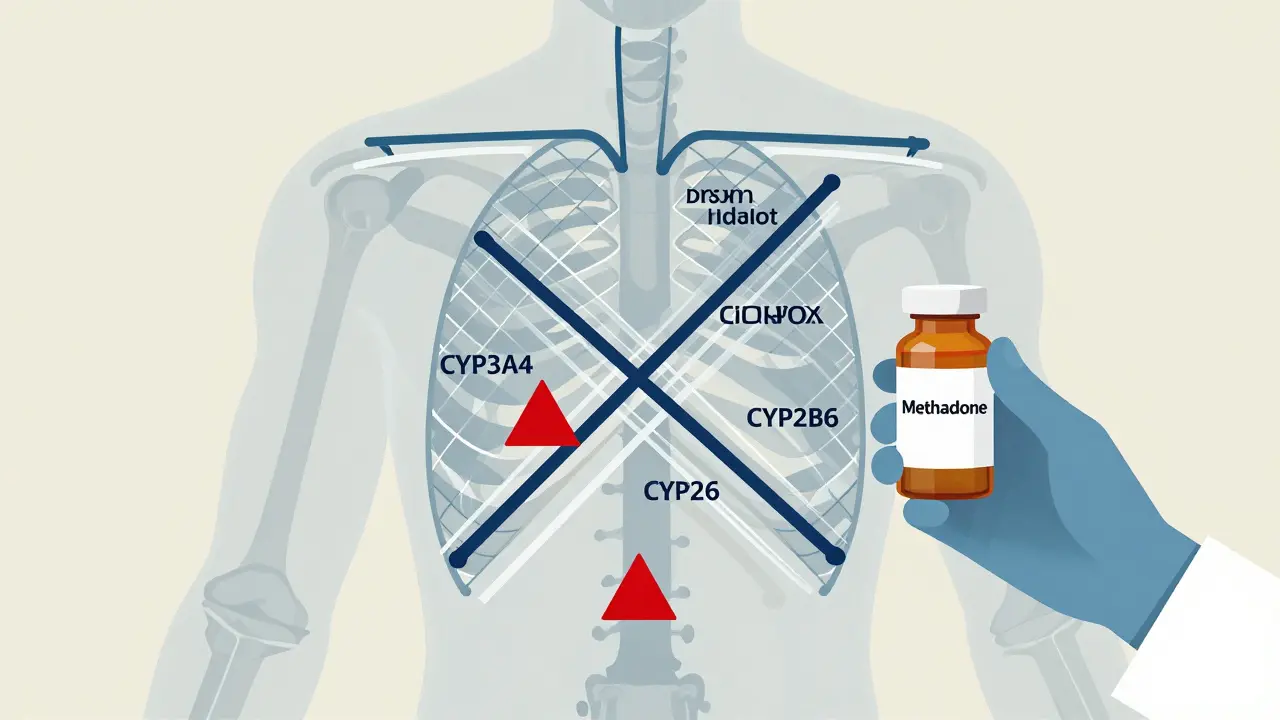
Who’s at Highest Risk?
It’s not just about the drug. It’s about the person. Here’s who needs extra attention:- Women (baseline QT is longer than men’s)
- People over 65
- Those with heart disease, especially prior arrhythmias
- Patients with liver impairment (slows methadone clearance)
- Anyone on multiple QT-prolonging drugs (antipsychotics, antibiotics, antidepressants)
- People with genetic variants in CYP2B6 (slow metabolizers)
What Clinicians Must Do
The old way-prescribe methadone, check liver enzymes, call it a day-is no longer enough. Here’s what works now:- Get a baseline ECG before starting methadone-even if the dose is 20 mg.
- Check electrolytes, especially potassium and magnesium.
- Review every medication the patient takes, including OTC drugs and supplements.
- Recheck ECG after any dose increase and after starting or stopping any new drug.
- Use the Bazett formula to correct QT for heart rate. Don’t trust the machine’s auto-read.
- Keep a list of high-risk drugs to avoid: fluoxetine, clarithromycin, fluconazole, valproate, ritonavir, quetiapine, citalopram, and many others.
Why Buprenorphine Is Gaining Ground
Buprenorphine doesn’t block hERG channels. It doesn’t prolong QT. Studies show less than 2% of buprenorphine patients have QTc over 500 ms-even at high doses. That’s why prescriptions for buprenorphine have grown from 1.4 million in 2016 to over 2.1 million in 2021. It’s not just about convenience. It’s about safety. That doesn’t mean methadone is obsolete. It’s cheaper. It works better for some patients with high opioid tolerance. But it demands more vigilance. If you choose methadone, you’re choosing a drug that needs constant monitoring-not just for overdose, but for heart rhythm.
The Hidden Delay: Methadone’s Long Half-Life
Here’s what many providers miss: methadone sticks around. Its half-life can be 24 to 59 hours. That means if you stop a CYP inhibitor like clarithromycin, methadone levels don’t drop right away. The QT prolongation can linger for days. A patient might feel fine, get their antibiotic stopped, and then-three days later-have a cardiac event. That’s why follow-up ECGs are crucial even after stopping an interacting drug. You can’t assume safety just because the interaction is over.What’s Next?
Researchers are working on a risk-prediction tool (NCT04567812) that factors in genetics, age, sex, liver function, and medication list to estimate QT risk before a single dose is given. It’s still in trials, but early results are promising. Meanwhile, the FDA and EMA have already updated methadone labels to warn about QT prolongation. Patient education materials now include clear warnings about symptoms: dizziness, fainting, palpitations. If a patient on methadone feels their heart skip or flutter, they need to get an ECG-today.Bottom Line
Methadone saves lives. But it can also end them-not from overdose, but from a silent heart rhythm gone wrong. The risk isn’t random. It’s predictable. It’s tied to CYP interactions, electrolyte imbalances, and genetic differences. Ignoring those factors isn’t negligence-it’s dangerous. If you’re prescribing methadone, don’t just look at the dose. Look at the whole picture. The patient’s meds. Their potassium. Their ECG. Their genetics. Their history. Because in methadone therapy, the most dangerous thing isn’t the opioid. It’s the unnoticed interaction.Can methadone cause sudden cardiac death even at low doses?
Yes. While higher doses increase risk, methadone can cause dangerous QT prolongation even at doses below 50 mg per day if combined with CYP inhibitors like fluoxetine, clarithromycin, or fluconazole. A 2023 ASAM guideline lowered the monitoring threshold to 50 mg/day because of this unpredictable risk.
Which drugs should never be taken with methadone?
Drugs that strongly inhibit CYP3A4 or CYP2B6 should be avoided. These include fluoxetine, clarithromycin, fluconazole, ritonavir (in Paxlovid), valproate, and certain antifungals and antivirals. Also avoid other QT-prolonging drugs like citalopram, quetiapine, and certain antibiotics (e.g., moxifloxacin). Always check for interactions before prescribing.
How often should ECGs be done for patients on methadone?
Baseline ECG is required before starting methadone. Repeat ECGs should be done after any dose increase, after starting or stopping any new medication (especially CYP inhibitors), and annually if stable. For patients on doses above 50 mg/day or with risk factors, ECGs every 3-6 months are recommended.
Is buprenorphine safer than methadone for the heart?
Yes. Buprenorphine does not significantly affect the hERG potassium channel and rarely causes QT prolongation. Multiple studies show its cardiac safety profile is far superior to methadone’s. For patients with heart disease, older adults, or those on multiple medications, buprenorphine is often the preferred choice.
Can electrolyte imbalances make methadone more dangerous?
Absolutely. Low potassium (hypokalemia) and low magnesium dramatically increase the risk of torsade de pointes in patients on methadone. Even mild imbalances can tip the balance. Regular blood tests for potassium and magnesium are essential, especially during illness, vomiting, or diuretic use.
Why does methadone’s long half-life make interactions riskier?
Methadone stays in the body for days-even up to six weeks in some cases. So if you stop a CYP inhibitor like fluconazole, methadone levels don’t drop immediately. QT prolongation can persist for days after the interacting drug is gone, meaning a patient might seem fine but remain at high risk. Follow-up ECGs are critical even after stopping other meds.
Are there genetic factors that affect methadone risk?
Yes. Some people have genetic variants in CYP2B6 that make them slow metabolizers of methadone. These individuals clear the drug much slower, leading to higher serum levels even at standard doses. Testing for CYP2B6 polymorphisms isn’t routine yet, but it’s being studied as part of future risk-prediction tools.
If you’re managing someone on methadone, don’t wait for a crisis. Set up a system: baseline ECG, regular labs, drug interaction checks, and patient education. The goal isn’t to scare people off methadone. It’s to make sure it’s used safely-because when done right, it saves lives.





Cassie Widders
January 12, 2026 AT 05:13I had a friend on methadone who got prescribed fluconazole for a yeast infection. She didn’t know it was risky. One morning she passed out in the shower. Scared the hell out of us. ECG showed QT over 500. She’s fine now, but it’s wild how something so common can almost kill you.
Doctors never warned her. Just said ‘take the pill.’
Daniel Pate
January 13, 2026 AT 04:04This is textbook pharmacology buried under bureaucratic indifference. The fact that we’re still treating methadone like it’s just another opioid is criminal. The hERG channel blockade isn’t theoretical-it’s quantifiable, predictable, and documented since the 90s. Why are we still relying on dose thresholds instead of metabolic profiling?
The real issue isn’t methadone. It’s that addiction medicine has been starved of resources and left to operate like a DIY garage project. We monitor liver enzymes but not QT intervals? That’s not negligence-it’s institutional laziness.
And yes, buprenorphine is safer. But it’s also more expensive, harder to access, and stigmatized. So we keep giving people a time bomb and calling it ‘treatment.’
Jose Mecanico
January 14, 2026 AT 09:53I work in a clinic that started using EHR alerts for methadone interactions last year. We caught three cases of fluoxetine + methadone combos before anyone got an ECG. One patient was on 40mg-thought they were fine. Turned out their QT was 498. We switched them to buprenorphine. No drama. No cardiac event.
Small changes, big results. Just need systems in place.
Alex Fortwengler
January 15, 2026 AT 04:01They’re lying to you. Methadone was designed to kill people quietly. The whole opioid epidemic? A cover. Big Pharma knew about the QT risk since the 70s. They pushed it because it’s cheap and addictive-perfect for controlling the poor. Now they’re pretending they just ‘didn’t know’.
Fluconazole? Ritonavir? All part of the plan. They want you dependent, then they want you dead so insurance doesn’t pay for your heart transplant.
Check your meds. Check your ECG. Don’t trust anyone in a white coat.
Also-why are they not talking about the 5G towers? They’re syncing with your potassium levels.
Cecelia Alta
January 16, 2026 AT 16:02Okay but let’s be real-how many people on methadone are also on antidepressants, antifungals, and just… kinda not eating because they’re depressed? It’s not rocket science. It’s basic human behavior.
My cousin was on 70mg, took Zpack for a cold, didn’t tell her provider, and ended up in the ICU. They didn’t even know she was on methadone. She was 28. She had a toddler.
And now? Everyone’s like ‘oh, just get an ECG.’ Like that’s easy when you don’t have insurance, a car, or a phone that works. This isn’t a medical issue. It’s a social justice crisis wrapped in a lab report.
Also, why does no one talk about how the system punishes people for surviving? You get clean, you get monitored like a criminal. You get sick, you get ignored. It’s all so… performative.
And buprenorphine? Yeah, it’s safer. But good luck getting a prescription if you’re not middle class and white. The system’s rigged. Always has been.
Faith Wright
January 17, 2026 AT 07:13Wow. So we’re now treating addiction like it’s a cardiac time bomb? Congrats. We’ve gone from ‘you’re a junkie’ to ‘you’re a walking EKG.’
Meanwhile, the people who need this info the most-those in rural clinics, homeless shelters, jail systems-won’t ever see it. They’ll get their methadone dose, get handed a pamphlet, and be told ‘call if you feel weird.’
And guess what? They won’t. Because ‘weird’ is normal when you’ve been surviving for years.
So yeah, the science is solid. But the system? Still broken. And no, an EHR alert won’t fix that.
gary ysturiz
January 17, 2026 AT 14:50This is exactly why we need more education-not just for doctors, but for patients too. I’ve seen people scared to take anything else because they think every pill is a death sentence. We need clear, simple info: ‘If you’re on methadone, avoid these meds, check your potassium, and get your ECG.’ No jargon. No fear. Just facts.
And if you’re a provider? Don’t wait for a tragedy. Do the work. It’s not hard. It’s just important.
Small steps save lives. Keep pushing for better care.
Jessica Bnouzalim
January 19, 2026 AT 02:36Okay, so… I’m a nurse in a MAT clinic, and I’ve seen this play out three times. One guy? Took clarithromycin for a sinus infection. Didn’t say anything. Three days later, he collapsed walking to the bathroom. QT was 512. He’s okay now. But he cried and said, ‘I didn’t know it could do that.’
We started giving out laminated cards with the bad meds on them. No more ‘I forgot.’ No more ‘I didn’t think it mattered.’
Also-yes, buprenorphine is better. But if you’re someone who needs methadone to stay alive? Don’t feel guilty. Just get checked. Please.
And if you’re on it? Tell your doctor EVERYTHING. Even that CBD oil you take. Even that herbal tea. Even that one time you took a friend’s Xanax. Everything.
It’s not about trust. It’s about survival.
laura manning
January 19, 2026 AT 15:34While the clinical observations presented herein are empirically valid and supported by peer-reviewed literature, the underlying systemic failures in addiction medicine warrant immediate institutional recalibration. The conflation of pharmacokinetic risk with moral judgment continues to impede evidence-based practice. Furthermore, the disproportionate burden of cardiac surveillance falls upon marginalized populations who lack access to diagnostic infrastructure, thereby exacerbating health inequities.
It is imperative that regulatory bodies mandate CYP genotyping as a prerequisite for methadone initiation, and that EHR systems be algorithmically integrated with the FDA’s Adverse Event Reporting System to preempt contraindicated polypharmacy.
Until such structural reforms are enacted, the current paradigm remains not merely suboptimal, but ethically indefensible.