What Exactly Is Constipation?
Constipation isn’t just about not going to the bathroom every day. Medically, it’s defined as having fewer than three bowel movements a week, along with hard stools, straining, or a feeling that you haven’t fully emptied your bowels. It’s one of the most common digestive complaints in the U.S., with over 2.5 million people seeing doctors for it every year. About one in three patients in clinical settings report symptoms, and women over 60 are especially likely to struggle with it.
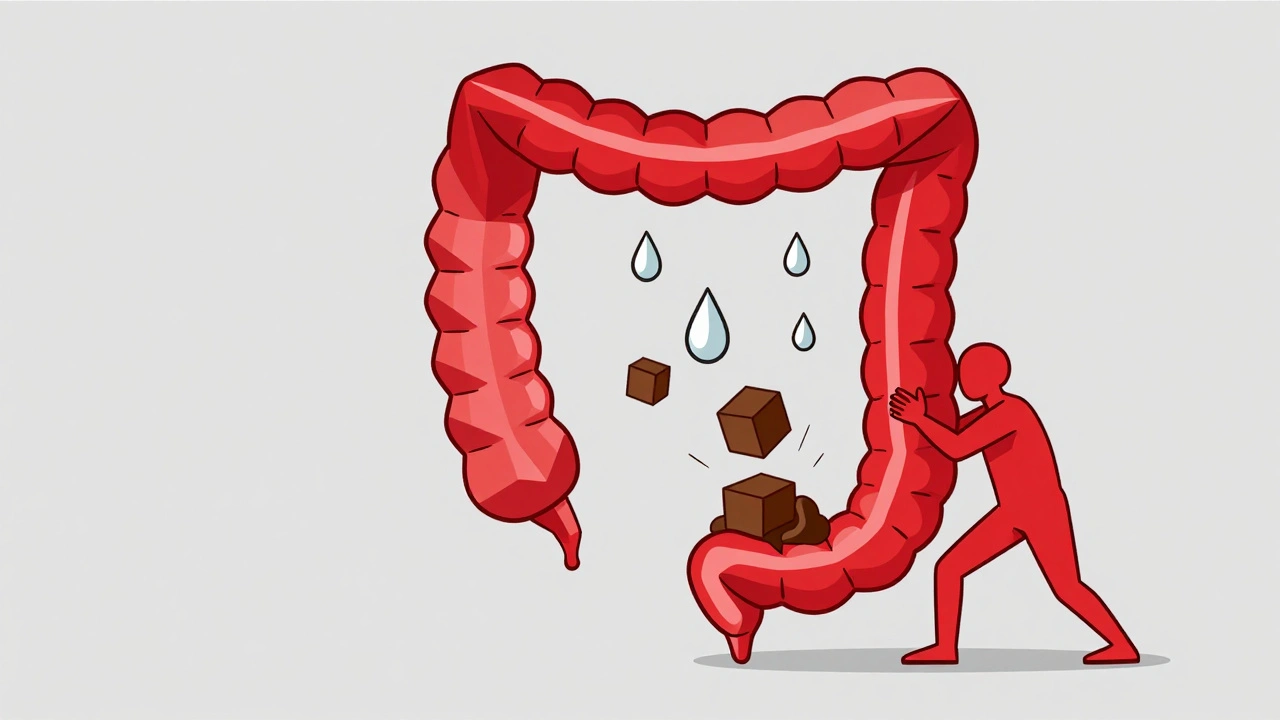
The problem starts when your colon absorbs too much water from waste. Normally, food moves through your digestive tract in 24 to 72 hours. But with constipation, that process slows down-sometimes to over 72 hours. The result? Dry, compacted stool that’s hard to pass. It’s not just uncomfortable; it can lead to hemorrhoids, anal fissures, or even bowel obstruction if left unaddressed.
Why Does Constipation Happen?
Constipation isn’t one thing-it’s a symptom with many roots. Some causes are simple, like not drinking enough water or eating too little fiber. Others are tied to health conditions or medications.
Most people don’t get enough fiber. The average American eats only about 15 grams a day, but experts recommend 25 to 30 grams. That’s a big gap. Without enough fiber, stool loses bulk and moves slower. Dehydration makes it worse. If you’re not drinking 1.5 to 2 liters of water daily, your colon pulls even more water from waste, making stools harder.
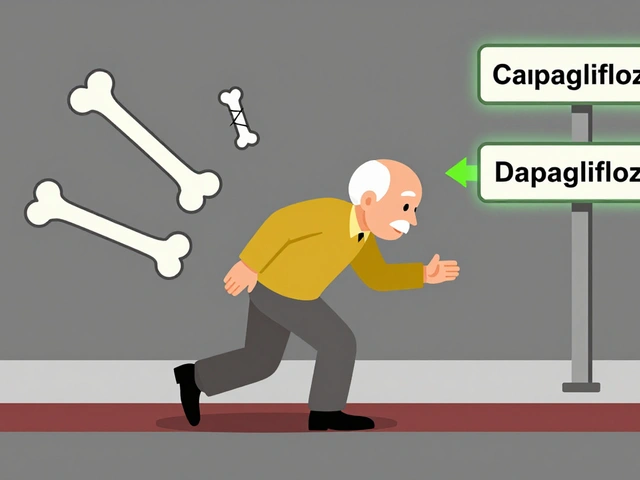
Medications are a major hidden cause. Opioids-used for pain-cause constipation in 40% to 95% of users. Calcium channel blockers (like nifedipine) and tricyclic antidepressants also slow digestion in a large portion of people who take them. Even iron supplements can trigger it.
Underlying health conditions play a big role too. Nearly 60% of people with diabetes have constipation because high blood sugar damages nerves that control bowel movement. Hypothyroidism slows metabolism, including digestion. Neurological conditions like Parkinson’s disease affect up to 80% of patients, and spinal cord injuries can disrupt signals to the colon and rectum.
Age matters. After 60, the risk of constipation goes up by about 1.5% every year. Pelvic floor muscles weaken, and the colon’s natural rhythm slows. Women are more affected than men, likely due to hormonal shifts and pregnancy-related changes.
Types of Constipation-And What They Mean
Not all constipation is the same. Doctors classify it based on what’s actually going wrong in your body.
Normal transit constipation is the most common-about 60% of chronic cases. Your colon moves stool at a normal speed, but you still feel straining, incomplete evacuation, or hard stools. This often responds well to fiber, water, and osmotic laxatives.
Slow transit constipation means stool moves too slowly through the colon. Transit time can exceed 72 hours. This type often needs stronger interventions, like prescription meds or even surgery in rare cases.
Defecatory disorders affect 20% to 50% of people with chronic constipation. The problem isn’t the colon-it’s the pelvic floor. Muscles don’t relax properly when you try to poop. You might push hard but nothing comes out. A balloon expulsion test (where you try to push out a small water-filled balloon) and anorectal manometry can confirm this. Biofeedback therapy helps in 70% to 80% of cases.
Refractory constipation means symptoms stick around even after trying one or more laxatives. About 15% to 20% of patients fall into this group. These cases often need specialized care, including advanced medications or testing for nerve or muscle dysfunction.
Laxatives: What Works and What Doesn’t
Laxatives are the go-to solution for many, but not all are created equal. Using the wrong type-or using them too long-can make things worse.
Bulk-forming laxatives (like psyllium or methylcellulose) add fiber to stool, making it softer and easier to pass. They’re great for normal transit constipation. But here’s the catch: you must drink plenty of water. Without it, they can cause blockages. Take one dose with at least 8 ounces of water, and keep drinking throughout the day.
Osmotic laxatives (like polyethylene glycol, or PEG 3350) pull water into the colon. PEG 3350 is the first-line recommendation from doctors. It’s effective in 65% to 75% of cases, has few side effects, and is safe for long-term use. Dose: 17 grams daily. Lactulose and magnesium hydroxide are also options, but can cause gas or cramping.
Stimulant laxatives (senna, bisacodyl) force the colon to contract. They work fast-usually within 6 to 12 hours. But they’re meant for short-term use only. Using them for more than 12 weeks can lead to “cathartic colon,” where the colon loses its natural ability to move stool. The American Gastroenterological Association advises against using these for more than three months.
Stool softeners (like docusate sodium) are often overprescribed. Studies show they’re only 10% to 15% more effective than a placebo. They’re not a standalone fix. Don’t waste money on them unless you’re combining them with something else.
Prescription options exist for stubborn cases. Lubiprostone, linaclotide, and plecanatide increase fluid secretion in the intestines. They’re used for irritable bowel syndrome with constipation (IBS-C) and refractory cases. Linaclotide works in 45% to 60% of patients. But they’re expensive-linaclotide costs over $1,000 a month without insurance.

Long-Term Management: Beyond Pills
True relief from chronic constipation doesn’t come from popping pills forever. It comes from changing habits-and sticking with them.
Start with fiber, but go slow. Jumping from 15g to 30g of fiber overnight will cause bloating in 30% to 40% of people. Increase by 5g every 3 to 4 days. Focus on soluble fiber: oats, beans, apples, chia seeds, and flaxseed. These absorb water and soften stool better than insoluble fiber like bran.
Hydration is non-negotiable. For every 5g of extra fiber you add, drink an extra 250 to 500mL of water. If you’re taking psyllium, you need at least 2 liters of water daily. Dehydration cancels out fiber’s benefits.
Train your body to go. Sit on the toilet for 10 to 15 minutes after breakfast. That’s when your gastrocolic reflex is strongest-your colon naturally wakes up after eating. Don’t rush. Don’t strain. Just sit. Use a footstool to elevate your feet. This puts your hips at a 35-degree angle, mimicking a squat. Studies show this reduces straining by 60%.
Biofeedback works for pelvic floor issues. If you’ve tried everything and still can’t pass stool easily, you might have a pelvic floor disorder. Biofeedback therapy retrains your muscles using sensors and real-time feedback. It takes 6 to 8 weekly sessions, each costing $100 to $150. But 70% to 80% of people see lasting improvement.
Exercise helps. Walking 20 to 30 minutes a day stimulates bowel motility. Even light activity like gardening or stretching can make a difference. Sedentary lifestyles are a major risk factor.
When to Worry: Red Flags
Constipation is usually harmless. But sometimes, it’s a sign of something serious.
See a doctor right away if you have:
- Unintentional weight loss of 10 pounds or more
- Rectal bleeding or dark, tarry stools
- Change in bowel habits lasting more than 6 weeks
- Family history of colorectal cancer
- New constipation after age 50, especially if you’ve never had it before
These aren’t just “constipation.” They could signal colon cancer, inflammatory bowel disease, or a bowel obstruction. The American College of Gastroenterology says these symptoms require immediate testing-usually a colonoscopy.
Real People, Real Results
One 52-year-old woman struggled with constipation for over 10 years. She tried senna, magnesium, and even enemas. Nothing stuck. Then she made three changes: she started taking 25g of psyllium husk every morning with 2 liters of water, drank coffee right after waking (to trigger her gastrocolic reflex), and sat on the toilet for 10 minutes after breakfast with her feet on a stool. Within eight weeks, she was having regular, easy bowel movements. No laxatives needed.
Another man, 68, had slow transit constipation. His doctor tried PEG 3350, but it wasn’t enough. He added daily walking and a 15-minute squatting routine after meals. After three months, his colon transit time dropped from 90 hours to 48 hours.
These aren’t miracles. They’re science-backed habits. The problem isn’t that people don’t know what to do. It’s that they give up too soon. Fiber and hydration take weeks to show results. Biofeedback isn’t a quick fix. But if you stick with it, most people find lasting relief.
What Doesn’t Work (And Why)
Many people waste time and money on ineffective solutions.
“Laxative dependency” is a myth. You don’t become addicted to osmotic laxatives like PEG 3350. Your colon doesn’t stop working. But if you rely on stimulant laxatives for months, you can damage your colon’s natural movement. That’s not dependency-it’s injury.
Drinking more coffee isn’t a cure. While caffeine can stimulate bowel movement in some people, it doesn’t fix the root cause. If you’re dehydrated, coffee might make constipation worse.
Apple cider vinegar, castor oil, and herbal teas? No solid evidence they help. They might give a short-term push, but they don’t improve long-term function. And castor oil can be dangerous-it’s a strong stimulant laxative with serious side effects.
The biggest mistake? Waiting too long to act. Most people try 3 or more laxatives before finding what works. On average, it takes 14.7 months to get effective relief. That’s over a year of discomfort. Early action saves time, money, and stress.
What’s Next in Constipation Care
Science is moving fast. In 2022, the FDA approved tenapanor (Ibsrela), a new drug that blocks sodium absorption in the gut, increasing fluid and movement. It’s helping people with IBS-C who didn’t respond to other treatments.
Researchers are also studying the gut microbiome. A 2023 NIH project found that people with constipation often have low levels of Bacteroides uniformis, a helpful gut bacteria. Future treatments might include targeted probiotics or prebiotics tailored to individual microbiomes.
And AI is getting involved. A team at Augusta University is testing smartphone apps that analyze how you push during bowel movements. Early results show 85% accuracy in spotting pelvic floor dysfunction-no expensive machines needed.
By 2030, constipation rates are expected to rise 12% due to aging populations and more diabetes cases. That means better, smarter solutions aren’t just nice to have-they’re essential.
Final Takeaways
Constipation is common, but it’s not normal. You don’t have to live with it.
Start with the basics: fiber, water, and regular toilet time. Use osmotic laxatives like PEG 3350 if needed, but avoid stimulants long-term. If that doesn’t work, see a specialist. Pelvic floor therapy, biofeedback, or prescription meds can change your life.
Don’t wait until you’re in pain. Don’t assume it’s just aging. And don’t believe the myths. With the right approach, most people can get back to regular, comfortable bowel movements-without relying on pills forever.



Stephanie Bodde
December 5, 2025 AT 08:25Philip Kristy Wijaya
December 5, 2025 AT 21:48William Chin
December 6, 2025 AT 23:24Ada Maklagina
December 7, 2025 AT 13:21Katie Allan
December 7, 2025 AT 22:07James Moore
December 9, 2025 AT 17:39Chris Brown
December 10, 2025 AT 17:41Stephanie Fiero
December 12, 2025 AT 07:32Laura Saye
December 14, 2025 AT 03:30Michael Dioso
December 15, 2025 AT 13:01Mark Curry
December 16, 2025 AT 10:51aditya dixit
December 16, 2025 AT 13:03