NSAID and Blood Thinner Checker
Check Your Medication Safety
This tool helps you identify if your pain medication is safe to take with blood thinners based on medical research.
More than 12 million Americans over 65 take blood thinners to prevent strokes or clots. Many of them also suffer from arthritis, back pain, or joint inflammation. So they reach for ibuprofen, naproxen, or diclofenac - the same painkillers you can buy off the shelf. But here’s the problem: NSAIDs and blood thinners don’t just mix poorly. They can turn a simple headache into a life-threatening bleed.
Why This Combination Is So Dangerous
NSAIDs like ibuprofen and naproxen work by blocking enzymes called COX-1 and COX-2. These enzymes help your body make prostaglandins - chemicals that cause pain and swelling. But they also help your platelets stick together to form clots and protect your stomach lining. When NSAIDs block them, your blood can’t clot as well, and your stomach becomes more vulnerable to damage. Blood thinners - whether warfarin, apixaban, rivaroxaban, or dabigatran - work differently. They slow down the proteins in your blood that form clots. That’s good if you’re at risk for a stroke or deep vein clot. But when you add an NSAID on top, you’re hitting the same system from two angles. Your platelets are weaker. Your stomach lining is thinner. Your blood takes longer to stop bleeding. The result? A perfect storm for internal bleeding. A 2024 study in Circulation tracked over 200,000 patients on blood thinners. Those who took NSAIDs had more than twice the risk of bleeding compared to those who didn’t. Some NSAIDs were worse than others. Naproxen increased bleeding risk by 4.1 times. Diclofenac? 3.3 times. Even ibuprofen, often thought of as "milder," still raised the risk by nearly 80%.Where the Bleeding Happens - And Why It’s Scary
Most people think of bleeding as a cut that won’t stop. But the real danger with this combo is internal bleeding - the kind you don’t see until it’s too late.- Gastrointestinal bleeding: This is the most common. NSAIDs damage the stomach lining. Blood thinners prevent clots from sealing the damage. The result? Ulcers, vomiting blood, or dark, tarry stools. Risk goes up 2.24 times.
- Intracranial hemorrhage: Bleeding in the brain. This is rare, but deadly. Risk jumps 3.22 times when NSAIDs are taken with anticoagulants.
- Urinary tract bleeding: Blood in urine. Often dismissed as a UTI, but can signal serious internal damage. Risk increases 1.57 times.
- Pulmonary bleeding: Coughing up blood. Less common, but still significantly higher with NSAID use.
Not All Blood Thinners Are the Same
If you’re on a blood thinner, knowing which one you’re taking matters. Warfarin has been around for decades and requires regular blood tests (INR). It interacts badly with NSAIDs - increasing bleeding risk by 3.8 times in some studies. Newer drugs, called DOACs (direct oral anticoagulants), like apixaban, rivaroxaban, and dabigatran, don’t need regular blood tests. They’re easier to use. But they’re not safer when mixed with NSAIDs. Here’s the breakdown:| Anticoagulant | Risk Increase with NSAIDs |
|---|---|
| Warfarin | 3.8 times higher |
| Dabigatran | 2.3 times higher |
| Rivaroxaban | 2.1 times higher |
| Edoxaban | 2.0 times higher |
| Apixaban | 1.9 times higher |
What About Celecoxib? Is It Safer?
Celecoxib is a COX-2 selective NSAID. It doesn’t affect platelets as much as ibuprofen or naproxen. That means it’s less likely to cause stomach ulcers. But it still raises bleeding risk - just not as high. Studies show celecoxib increases bleeding risk by 1.4 times when taken with anticoagulants. That’s better than naproxen’s 4.1 times. But it’s still a 40% increase. And it doesn’t protect you from brain or lung bleeds. So while it’s a slightly better option, it’s still not safe.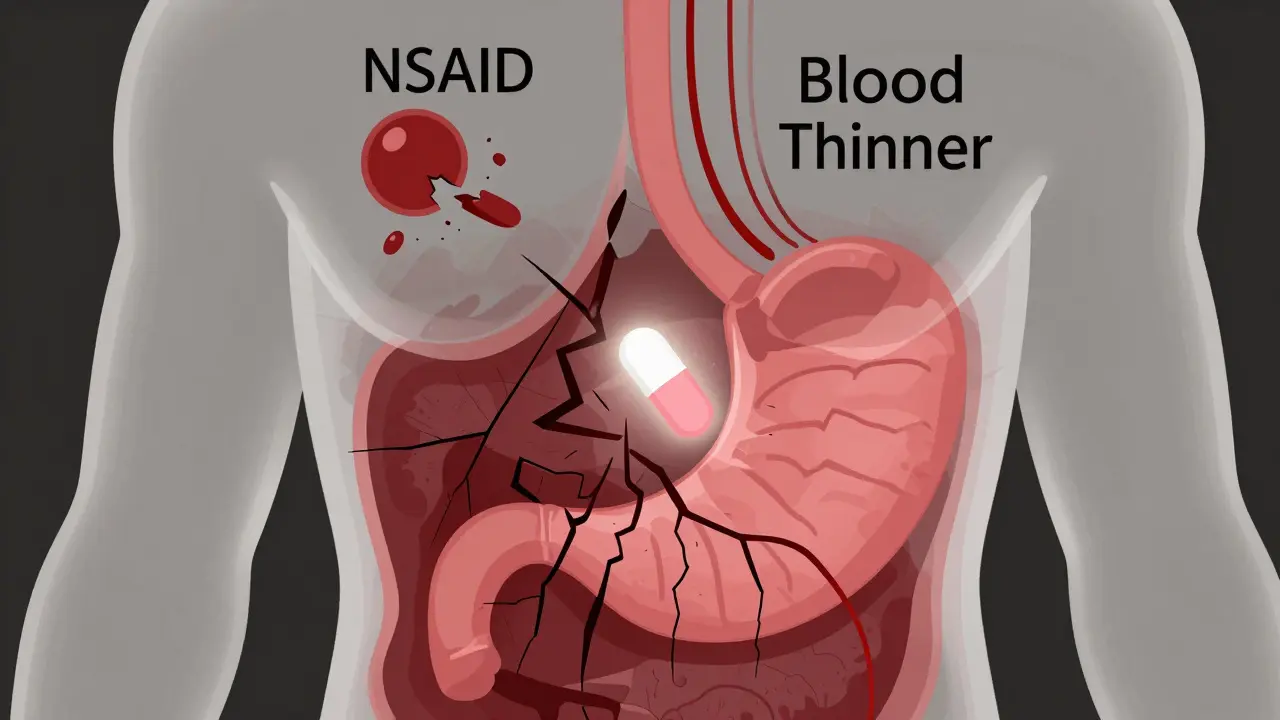
The Only Safe Painkiller: Acetaminophen
If you’re on a blood thinner and need pain relief, acetaminophen (Tylenol) is the only over-the-counter option proven to be safe. At standard doses - up to 4,000 mg per day - it doesn’t interfere with clotting or stomach protection. But it’s not perfect. Too much acetaminophen can damage your liver. If you drink alcohol regularly, have hepatitis, or take other liver-metabolized drugs, even 3,000 mg a day might be risky. Always check with your doctor or pharmacist. A 2023 Cleveland Clinic study followed 300 patients who switched from NSAIDs to acetaminophen for arthritis pain. After four weeks, 68% reported pain was well-controlled. They didn’t need the NSAIDs. Their mobility didn’t suffer. And their bleeding risk dropped to normal.What If You Really Need an NSAID?
Sometimes, a doctor might say: "Use ibuprofen for three days after your dental work." Or: "Take naproxen for a flare-up of gout." If you must use an NSAID - even briefly - follow these rules:- Use the lowest possible dose. For ibuprofen, that’s 200-400 mg, not 600-800 mg.
- Use it for the shortest time. Three days max. Never more than a week.
- Take it with food. This helps protect your stomach.
- Ask for a stomach protector. A proton pump inhibitor (PPI) like pantoprazole 40 mg daily reduces ulcer risk by 70%. Many doctors now prescribe this automatically when NSAIDs are needed.
- Don’t take it with your blood thinner. Space them out by at least 8 hours. Some trials showed this cuts bleeding risk by nearly 30%.
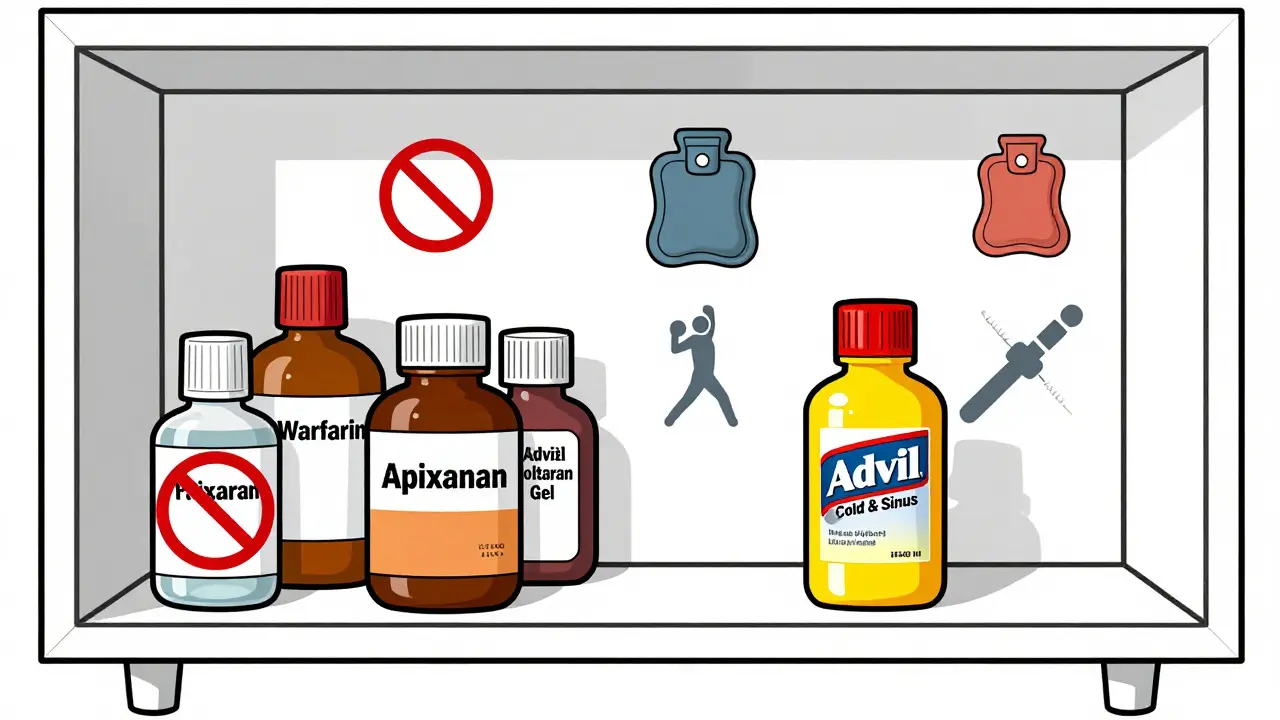
Hidden NSAIDs Are Everywhere
Most people know ibuprofen and naproxen. But many don’t realize NSAIDs are hiding in other medicines.- Advil Cold & Sinus
- Naprosyn (prescription)
- Midol for menstrual pain
- Many "cold and flu" formulas
- Topical gels like Voltaren (diclofenac gel)
What Patients Are Saying
On Reddit’s r/Anticoagulants, over 1,400 patients shared their experiences. 62% admitted using NSAIDs with blood thinners. 38% had bleeding complications: nosebleeds, bruises that wouldn’t fade, or dark stools. One woman wrote: "I took ibuprofen for my knee for two weeks. I passed out from anemia. I didn’t know it was the pills." Another wrote: "My doctor told me to stop NSAIDs. I did. My pain got worse. I started using heat packs and physical therapy. Now I can walk again - and I haven’t bled since." Success stories almost always involve switching to acetaminophen, physical therapy, or alternative pain management - not trying to "get away with" NSAIDs.The Bigger Picture
This isn’t just about individual risk. It’s a public health crisis. In the U.S. alone, NSAID-anticoagulant interactions cause:- 87,000 emergency room visits a year
- 24,000 hospitalizations
- $1.2 billion in annual healthcare costs
What You Should Do Now
If you’re on a blood thinner:- Stop taking any NSAID unless your doctor says it’s absolutely necessary.
- Check every medicine you take - even creams and cold pills - for ibuprofen, naproxen, diclofenac, or ketoprofen.
- Switch to acetaminophen for pain.
- Ask about physical therapy, heat, or stretching for joint pain.
- Tell every new doctor, dentist, or pharmacist you’re on a blood thinner.
- If you’ve had unexplained bruising, dark stools, or nosebleeds, tell your doctor immediately.
What’s Next?
The American Heart Association’s new guidelines, expected in January 2025, will likely make warnings even stronger. New AI tools are being tested to automatically flag NSAID prescriptions for patients on anticoagulants. Some trials are even testing modified NSAIDs that don’t affect platelets. But the real solution isn’t technology. It’s awareness. It’s patients asking questions. It’s doctors listening. It’s pharmacists double-checking. Because the truth is simple: If you’re on a blood thinner, NSAIDs aren’t worth the risk. There are safer ways to manage pain. You don’t have to suffer. But you do have to be careful.Can I take ibuprofen with warfarin?
No. Taking ibuprofen with warfarin significantly increases your risk of serious bleeding - especially in the stomach and brain. Warfarin already makes your blood clot slower, and ibuprofen reduces platelet function and damages your stomach lining. Even small doses can be dangerous. If you need pain relief, use acetaminophen instead and always check with your doctor before taking anything.
Is naproxen safer than ibuprofen with blood thinners?
No. Naproxen is actually riskier than ibuprofen when taken with blood thinners. Studies show it increases bleeding risk by 4.1 times compared to 1.79 times for ibuprofen. Both are dangerous. Neither is safe. The only approved alternative is acetaminophen.
What about topical NSAIDs like Voltaren gel?
Topical NSAIDs like diclofenac gel are absorbed through the skin, so less enters your bloodstream. But they still raise bleeding risk - especially if you use them often, on large areas, or with broken skin. Studies show even topical NSAIDs can increase bleeding risk by 1.5 times when combined with blood thinners. They’re not risk-free. Acetaminophen or physical therapy are still safer choices.
Can I take aspirin with my blood thinner?
Aspirin is also an NSAID - and it blocks platelets. Taking it with a blood thinner like warfarin or apixaban doubles your bleeding risk. Unless your doctor specifically prescribed low-dose aspirin for heart protection (which is rare now), you should avoid it. Don’t assume aspirin is safe just because it’s old or sold for heart health.
How do I know if I’m bleeding internally?
Signs include: dark, tarry stools; vomiting blood or material that looks like coffee grounds; unexplained bruising or large bruises without injury; pink or red urine; severe headaches or dizziness (could mean brain bleed); sudden weakness or confusion. If you notice any of these, seek medical help immediately. Don’t wait. Internal bleeding can be silent until it’s life-threatening.
What painkillers are safe with apixaban or rivaroxaban?
Acetaminophen (Tylenol) is the only over-the-counter painkiller proven safe with DOACs like apixaban and rivaroxaban at standard doses (up to 4,000 mg per day). Avoid all NSAIDs - including ibuprofen, naproxen, and celecoxib. Always check with your pharmacist before taking any new medicine, even herbal supplements.
Can I use heat packs or physical therapy instead of NSAIDs?
Yes - and many patients do better with them. Heat packs, cold packs, stretching, and physical therapy can reduce arthritis and joint pain just as effectively as NSAIDs - without the bleeding risk. A 2023 Cleveland Clinic study found 68% of patients who switched from NSAIDs to physical therapy reported good pain control after four weeks. Talk to your doctor about a referral.
Should I stop NSAIDs cold turkey if I’ve been taking them?
If you’ve been taking NSAIDs regularly for pain, stopping suddenly might cause rebound pain or inflammation. But you shouldn’t keep taking them while on a blood thinner. Talk to your doctor about switching to acetaminophen and starting physical therapy or other non-drug treatments. They can help you taper off safely if needed.




![Buy Generic Lexapro (Escitalopram) Online Cheap-Safe UK Options, Prices, and Checks [2025]](/uploads/2025/09/thumbnail-buy-generic-lexapro-escitalopram-online-cheap-safe-uk-options-prices-and-checks.webp)

christy lianto
January 8, 2026 AT 16:04Just had my knee replaced last year and was on apixaban. My doctor told me straight: no NSAIDs. I tried ibuprofen once for a headache and woke up with a nosebleed that wouldn’t stop. Scared the hell out of me. Now I use Tylenol and heat packs. Pain’s still there, but I’m alive to feel it.
Luke Crump
January 9, 2026 AT 20:38So let me get this straight - we’re being told that the only safe painkiller is acetaminophen, which can kill your liver if you drink coffee or breathe wrong? This isn’t medicine, it’s Russian roulette with a pharmacy label. We’re being forced into a corner where pain is the lesser evil. Who decided this? A committee of people who’ve never had a bad back?
Annette Robinson
January 11, 2026 AT 18:19I’m a nurse, and I see this all the time. Elderly patients come in with dark stools and say, ‘Oh, I just took Advil for my arthritis.’ They don’t realize it’s not ‘just’ Advil - it’s a silent killer when paired with their blood thinner. Please, if you’re on anticoagulants, don’t gamble. Talk to your pharmacist. They’re the unsung heroes who catch these mistakes before the ER does.
Ken Porter
January 13, 2026 AT 04:40Another nanny-state overreaction. People used to manage pain without a PhD in pharmacology. If you want to take ibuprofen, take it. If you bleed, you bleed. Stop treating adults like toddlers with a pill bottle.
swati Thounaojam
January 14, 2026 AT 00:02i read this and thought of my dad. he’s on warfarin and takes diclofenac gel for his knee. he says it’s ‘just on the skin’ so it’s fine. i’m gonna show him this post. thank you for writing this.
Donny Airlangga
January 15, 2026 AT 01:48My mom had a GI bleed last year after taking naproxen for a week. She didn’t even know it was dangerous. We found out because she passed out in the kitchen. Now she uses Tylenol and does yoga twice a week. Her pain is manageable. Her quality of life? Way better. This isn’t just about avoiding bleeding - it’s about living without fear.
Molly Silvernale
January 16, 2026 AT 20:44There’s a quiet tragedy here - not in the statistics, not in the ER visits, but in the silence. The silence of the 72-year-old who grits their teeth through morning stiffness because they’re too afraid to ask, ‘Is this safe?’ The silence of the daughter who Googles ‘can I take ibuprofen with rivaroxaban’ and finds conflicting Reddit threads. We’ve turned medical advice into a scavenger hunt. And the prize? A second chance at life - if you’re lucky enough to find the right clue.
Joanna Brancewicz
January 17, 2026 AT 22:07DOACs + NSAIDs = synergistic anticoagulant effect with amplified GI mucosal injury. Acetaminophen remains first-line. PPI co-prescription reduces but doesn’t eliminate risk. Topical NSAIDs still have systemic absorption - especially with compromised skin integrity. Always screen OTC meds.
Evan Smith
January 19, 2026 AT 20:33So wait - you’re telling me I can’t take Advil for my headache after my wife’s surgery because I’m on Xarelto? But I can take Tylenol? That’s like saying you can’t drink soda but you can drink Diet Coke. Both have sugar. One’s just prettier. 😅
Lois Li
January 20, 2026 AT 05:59I’ve been on warfarin for 12 years. I used to take naproxen for my back. Then I started physical therapy. I didn’t know how much better I could feel until I stopped chasing pain with pills. I still have bad days - but I don’t have hospital days anymore. If you’re scared to stop NSAIDs, start small. One day without. Then two. You might be surprised how much your body adapts.
Manish Kumar
January 21, 2026 AT 21:06Think about it - we live in an age where we can map the human genome but we still can’t design a painkiller that doesn’t turn your blood into a leaky faucet. The irony is that the body’s own mechanisms - inflammation, clotting - are both essential and dangerous. We’ve weaponized our own biology against ourselves. Maybe the real question isn’t ‘What’s safe?’ but ‘Why did we ever think we could outsmart evolution with a pill?’