Getting hit with a $150 monthly copay for your medication isn’t just annoying-it can make you skip doses or skip filling the prescription altogether. But what if you could drop that same drug from tier 4 to tier 2 and pay only $40 instead? That’s where a tier exception comes in. It’s not a secret loophole. It’s a formal right built into Medicare Part D and most private insurance plans. And yet, most people never ask for it.
What Exactly Is a Tier Exception?
Your insurance plan puts your medications into tiers. Tier 1 is usually generic drugs with the lowest copay-sometimes even $0. Tier 2 is preferred brand-name drugs. Tier 3 is non-preferred brands. Tier 4 and 5? Those are specialty drugs-often biologics, cancer meds, or treatments for autoimmune diseases-and they can cost $100 to over $1,000 per month. You pay a percentage of the price, not a flat fee. A tier exception lets you move a drug from a higher tier to a lower one-even if it’s not the plan’s first choice-because your doctor says you need it. It’s not about the drug being better. It’s about your body reacting differently. Maybe the cheaper alternative gave you nausea, or caused a dangerous drop in blood pressure, or didn’t control your symptoms at all. That’s enough. The Centers for Medicare & Medicaid Services (CMS) defines it clearly: a tier exception is a request to get a drug on the formulary at a lower cost-sharing level. It’s different from a formulary exception, which is for drugs your plan doesn’t cover at all. This one? You’re asking to pay less for a drug they already cover-but too expensively.Why Most People Don’t Ask (And Why You Should)
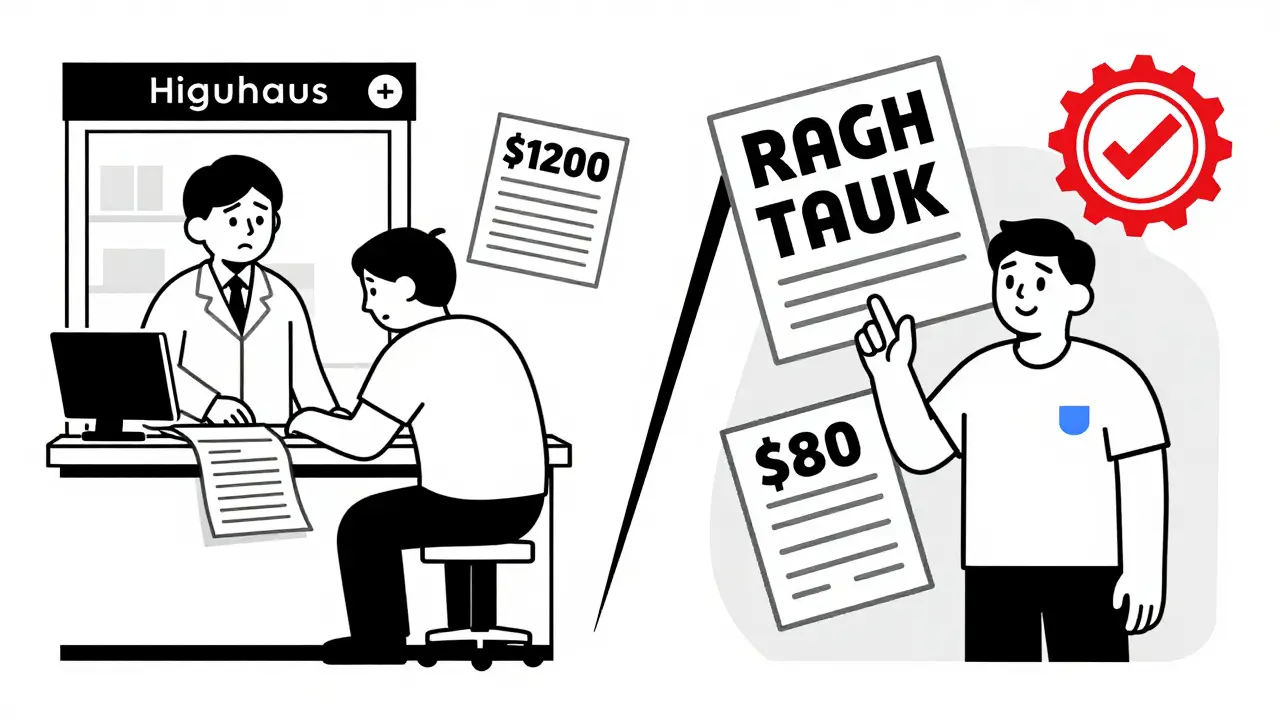
A 2023 survey by the Medicare Rights Center found that only 18% of patients who could benefit from a tier exception actually request one. Why? Because they don’t know it’s an option. Or they assume their doctor already handled it. Or they got scared off by the paperwork. Here’s the reality: if your drug is on your plan’s formulary but you’re paying $80 a month, and there’s a cheaper version of the same drug class that your doctor says won’t work for you, you’re leaving money on the table. The average savings? $37.50 per fill. That’s over $450 a year for one drug. For specialty meds, moving from tier 4 to tier 2 can cut costs from $1,200 to $80 a month. That’s not a small win-it’s life-changing. And here’s the kicker: 62% of tier exception requests are approved when submitted with proper documentation. That’s better than flipping a coin. But if the paperwork is sloppy? Approval drops to 31%.How to Get a Tier Exception: Step by Step
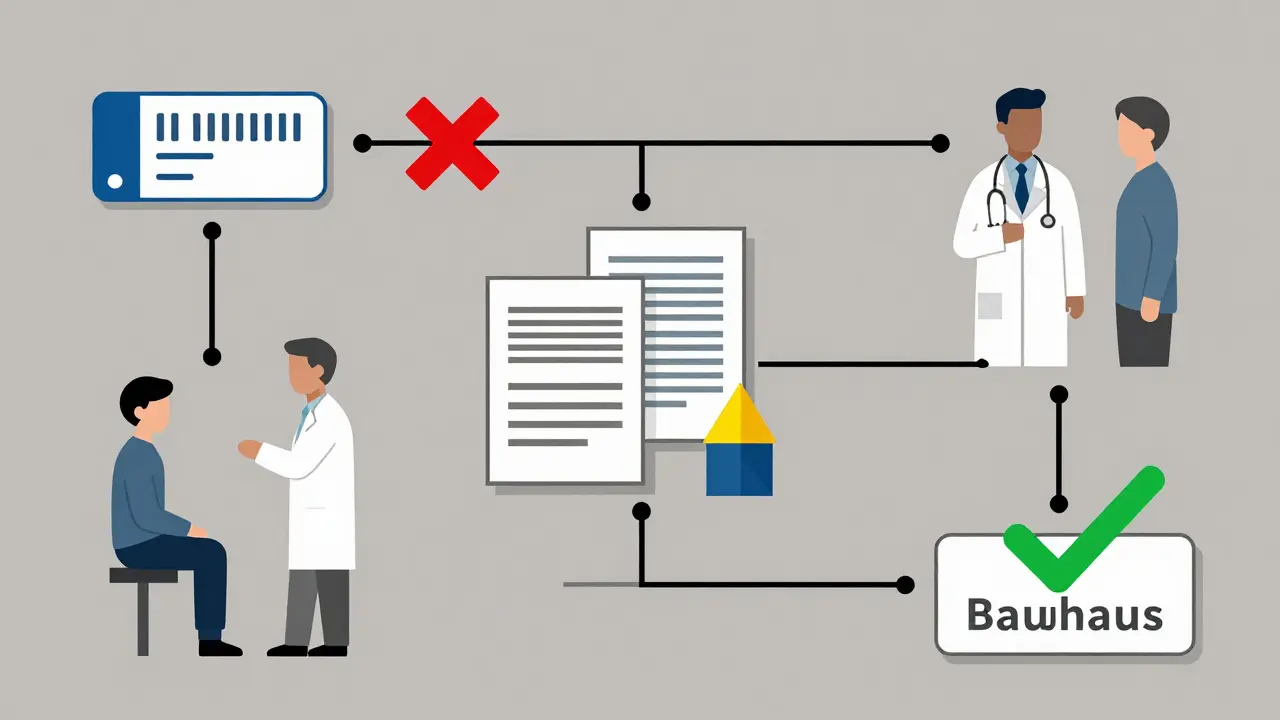
It’s not complicated. But it does require two people: you and your doctor.- Check your copay before filling the prescription. When your pharmacy tells you the price, ask: “Is this the lowest tier this drug is on?” If it’s not, and it’s higher than you expected, don’t fill it yet.
- Ask your doctor to submit a tier exception request. Tell them: “I can’t afford this copay. Can you request a tier exception to move this drug to a lower tier?” They’ll need to fill out a form from your insurer. Most have online portals now. Some still use paper.
- Make sure the doctor’s note is specific. Generic statements like “This drug works better for me” won’t cut it. They need to say: “Patient experienced severe dizziness and syncope on Lisinopril. Switching to Losartan is medically necessary due to intolerance.” Or: “Patient developed GI bleeding on Warfarin. Apixaban is required to avoid recurrence.” Specifics = approval.
- Submit the request. Your doctor’s office can submit it for you. Or you can log into your insurer’s portal and upload the form yourself. Either way, keep a copy.
- Wait for a decision. For non-emergencies, you’ll hear back in 14 days. If your doctor says your health is at risk without the drug, request an expedited review-you’ll get a decision in 72 hours.
What If They Say No?
Denials happen. But they’re not final. About 37% of initial requests get denied because the clinical documentation is too vague. That’s fixable. You can appeal. And 78% of appeals with better documentation get approved. Here’s how to appeal:- Get a second note from your doctor. Add more detail: lab results, hospitalizations, prior medication failures.
- Include a letter from your pharmacist if they’ve seen you struggle with side effects.
- Call your insurer’s member services. Ask for the appeals process. Write down the name of the rep you speak to.
Which Drugs Are Most Likely to Qualify?
Tier exceptions are most common-and most valuable-for drugs treating chronic, complex conditions:- Rheumatoid arthritis: Biologics like Humira, Enbrel, or Orencia often sit in tier 4. Moving to tier 3 can cut costs by 70%.
- Multiple sclerosis: Drugs like Tysabri or Lemtrada are specialty tier. A tier exception can drop coinsurance from 35% to $50 flat.
- Heart failure or atrial fibrillation: Switching from a generic blood thinner to a preferred brand due to bleeding risk.
- Diabetes: Insulin analogs like Humalog or Lantus sometimes get stuck in tier 3. If you’re on Medicare, you’re now capped at $35/month for insulin-but tier exceptions still help with other meds like GLP-1 agonists.
Timing Matters
Don’t wait until you’ve paid $150 for your first fill. The best time to request a tier exception is right after your doctor writes the script-before you go to the pharmacy. New trend: “Proactive tier exceptions.” Doctors submit the request at the same time they write the prescription. In 2023, UnitedHealthcare reported 89% approval rates for proactive requests versus 67% for reactive ones. Why? Because the insurer gets the full picture before the patient even tries the drug.What’s Changing in 2025?
Starting in 2025, the Inflation Reduction Act caps out-of-pocket drug costs for Medicare Part D beneficiaries at $2,000 per year. That’s huge. But here’s the catch: that cap only kicks in after you’ve spent $2,000. So if you’re paying $100 a month for a drug, you’ll hit that cap in 20 months. But if you lower your copay to $40? You’ll hit it in 50 months. Tier exceptions still matter. They keep you under the cap longer. They reduce financial stress. They prevent gaps in care. And even if you’re not on Medicare-most private insurers use the same tier system. The rules are similar. The process is the same.Final Tip: Know Your Plan
Every plan is different. Some have 4 tiers. Some have 5. Some include specialty drugs in tier 4. Others have a separate tier 5. Your plan’s formulary list is online. Look it up. Find your drug. See what tier it’s on. Then compare it to alternatives. If you see a drug in a lower tier that’s in the same class, ask your doctor: “Could I use this? If not, why?” That’s your opening to request an exception. You don’t need to be a medical expert. You just need to know your rights. And if you’re paying too much for a drug your doctor says you need, you’re not being unreasonable. You’re being smart.Can my pharmacist help me with a tier exception?
Your pharmacist can tell you what tier your drug is on and explain your copay. They can also give you the right forms or direct you to your insurer’s portal. But they can’t write the medical justification-that’s your doctor’s job. They can, however, help you spot when a tier exception might be worth pursuing.
Do I need to be on Medicare to use tier exceptions?
No. While tier exceptions are most commonly discussed in Medicare Part D, most private insurance plans-like those from UnitedHealthcare, Aetna, or Blue Cross-use the same tiered formulary system. The process is nearly identical. Check your plan’s drug list and ask your doctor if you’re paying more than necessary.
How long does a tier exception take to approve?
Standard requests take up to 14 days. If your doctor says your health is at risk without the drug-like if you’re at risk of hospitalization or worsening symptoms-you can request an expedited review. That cuts the wait to 72 hours. Many insurers now offer online tracking so you can see the status in real time.
Can I request a tier exception for multiple drugs at once?
Yes. You can submit multiple requests at the same time. But each one needs its own medical justification. Don’t lump them together. For each drug, your doctor must explain why the lower-tier alternatives won’t work for you. It’s more work, but if you’re on several high-cost meds, it’s worth it.
Will a tier exception affect my coverage in the Medicare doughnut hole?
Yes. Moving a drug to a lower tier means you pay less out of pocket, which helps you get out of the coverage gap faster. Once you reach the catastrophic coverage phase, you pay 5% or a small copay. But until then, every dollar you save on copays counts toward your out-of-pocket total. Lower copay = faster exit from the doughnut hole.
What if my doctor won’t submit a request?
Some doctors don’t know about tier exceptions or think it’s too time-consuming. Politely explain: “I’m trying to avoid skipping doses because I can’t afford this. Can you help me request a lower tier?” If they still refuse, ask for a referral to a patient advocate. Many hospitals and nonprofits offer free help with insurance appeals. You’re not asking for a favor-you’re exercising your right as a patient.







Solomon Ahonsi
February 2, 2026 AT 10:02This is bullshit. I’ve been on Humira for 6 years and my copay’s still $120. My doctor won’t even file the damn form because he says ‘it’s a waste of time.’ Guess what? It is. Unless you’re rich or have a personal assistant, this whole system is rigged.
George Firican
February 2, 2026 AT 22:05The real tragedy here isn’t the tier system-it’s the fact that we’ve normalized medical debt as part of the American experience. People are choosing between insulin and groceries, and the system doesn’t just fail them-it actively incentivizes that failure. A tier exception isn’t a loophole; it’s a Band-Aid on a hemorrhage. We need universal drug pricing, not patient gymnastics to get basic care. But until then, yes, this guide is one of the few practical lifelines left.
Matt W
February 4, 2026 AT 00:46Just did this last month for my Xarelto. Went from $65 to $35. My doctor was skeptical at first, but when I showed him the CMS guidelines and said I’d skip doses if I had to pay full, he filed it same day. Took 9 days. Approved. No drama. Just paperwork. Do it. Your body deserves more than a spreadsheet.
Anthony Massirman
February 6, 2026 AT 00:01Do it. Save money. Don’t be lazy.
jay patel
February 7, 2026 AT 06:27so i tried this for my metformin and they denied it because it was 'too generic' lmao. i mean, if you're gonna charge me 80 bucks for a pill that costs 2 cents to make, at least let me appeal with a photo of my empty fridge. my doc just shrugged and said 'welcome to healthcare in 2025' 😅
Hannah Gliane
February 9, 2026 AT 03:46Wow. So you’re telling me that people who can’t afford their meds should just ‘ask nicely’? And the doctor’s gonna magically fix it? 😂 I’ve seen this before. You think you’re clever until you’re on the phone with your insurer for 47 minutes while your blood sugar spikes. This isn’t empowerment-it’s exploitation dressed up as a checklist.
Ellie Norris
February 10, 2026 AT 03:03Just wanted to add-I’m a pharmacist in Manchester and we see this all the time. If your doctor says ‘I don’t know how to submit,’ ask for the form number on the insurer’s site. Most have a ‘Tier Exception Request Form’ under ‘Provider Resources.’ I’ve helped 3 people this week alone. You’re not being a pain-you’re being smart.
Chinmoy Kumar
February 10, 2026 AT 22:22i read this and i thought wow this is so practical but then i remembered my cousin in delhi who pays 2000 rupees a month for his insulin and has no insurance at all. i feel guilty even thinking about tier exceptions when the real problem is global access. but still… this is useful for those who have a system to game. thank you for sharing
Gary Mitts
February 11, 2026 AT 21:03My doctor refused to file because he said 'it's not his job' so I did it myself. Took 20 minutes. Approved. The system hates you but it's not invincible. Just don't wait until you're out of pills
clarissa sulio
February 12, 2026 AT 14:27Why are we even talking about this? This is why America is crumbling. You’re supposed to get care because you’re a human, not because you jumped through 12 bureaucratic hoops. This isn’t a guide-it’s a confession that our healthcare system is broken and we’re all just scavenging scraps.
Bridget Molokomme
February 13, 2026 AT 08:43My mom got her Enbrel moved from tier 4 to tier 2 last year. She cried when she saw the new copay. Said she finally felt like a person again, not a cost center. If you’re reading this and you’re scared of paperwork? Do it for her. Do it for the people who can’t speak up.