When a teenager stops eating, sleeps all day, or says they don’t care anymore, it’s easy to brush it off as moodiness. But for one in five adolescents, this isn’t just a phase-it’s clinical depression. And when it hits, the whole family feels it. Parents scramble for answers: family therapy or medication? Both can help, but they work in very different ways.
What Does Depression Look Like in Kids and Teens?
Depression in children and teens doesn’t always look like sadness. A 13-year-old might explode over homework. A 16-year-old might quit sports, stop texting friends, or sleep 12 hours a day. Some act out. Others shut down. The DSM-5 criteria for major depressive disorder in this age group include persistent low mood, loss of interest, changes in sleep or appetite, fatigue, feelings of worthlessness, and sometimes thoughts of death or suicide.
It’s not rare. Around 13% of U.S. adolescents experience at least one major depressive episode by age 18. And it’s not just emotional-it affects school performance, relationships, and future health. Left untreated, early depression increases the risk of chronic mental illness, substance use, and even suicide. The 988 Suicide & Crisis Lifeline handled over 4.4 million contacts in 2023, up 21% from 2022. That’s not just numbers-it’s real kids, real families, in real pain.
Why Family Therapy Matters
Family therapy isn’t about blaming parents. It’s about understanding how the family system keeps depression going-and how to change it.
One of the most effective approaches is Attachment-Based Family Therapy (ABFT). It focuses on repairing the emotional bond between parent and child. When a teen feels unheard, unloved, or unsafe expressing pain, depression grows. ABFT helps parents learn to listen without fixing, to validate without judging. In a 2022 study from Jefferson Digital Commons, teens in ABFT showed significantly greater drops in suicidal thoughts than those in standard care. The difference wasn’t small-it was statistically clear.
Other models like Structural Family Therapy fix power imbalances-like when a 14-year-old is making all the rules, or when a parent is emotionally absent. Strategic Family Therapy uses clever techniques, like asking the teen to keep being depressed “for the family’s sake,” which sounds odd but often breaks the cycle of conflict and helplessness.
Studies show family therapy works best when communication is broken. If parents criticize constantly, avoid talking about feelings, or argue in front of the teen, therapy can rebuild trust. Data from the Children’s Hospital of Philadelphia found that 8-12 weeks of family therapy improved communication patterns for most families. Parents in NAMI forums say learning how to speak without blaming was the most valuable part.
But it’s not easy. Family therapy requires everyone to show up-literally and emotionally. If one parent refuses to participate, or if the teen feels the therapist is siding with their parents, progress stalls. About 41% of families who quit therapy say it was because someone resisted. And scheduling 12-16 weekly sessions? That’s tough when you’ve got two jobs, three kids, and no car.
When Medication Makes Sense
Medication doesn’t fix relationships. But it can fix brain chemistry.
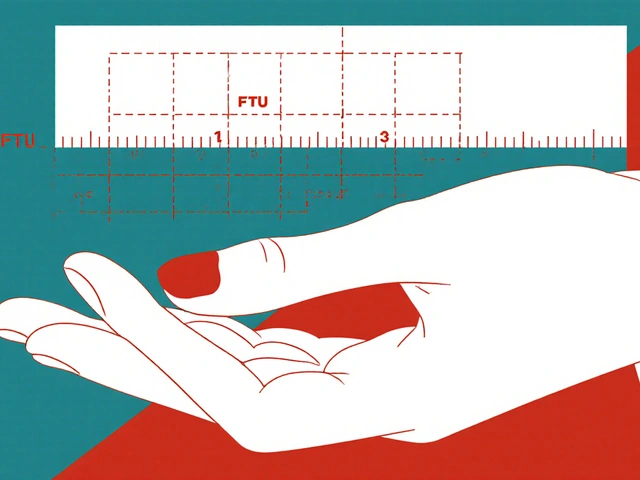
The FDA has approved only two SSRIs for teens: fluoxetine (Prozac) and escitalopram (Lexapro). That’s it. Other antidepressants are used off-label, but these two have the strongest safety data for adolescents. Dosing usually starts low-10 mg/day-and increases slowly to 20 mg/day over weeks. Full effect takes 4-6 weeks. That’s longer than most teens are willing to wait.
And there’s a catch. All antidepressants carry a black box warning from the FDA, issued in 2004. In the first few weeks of treatment, a small number of teens-about 11-18%-experience increased suicidal thoughts. That’s why doctors require weekly check-ins at first. It’s scary, but the risk drops sharply after month two. The Treatment for Adolescents with Depression Study found that when medication was combined with therapy, suicide risk went down more than with either alone.
Side effects are common: nausea, headaches, insomnia, jitteriness. About 32% of teens in that same study stopped taking SSRIs because of them. But for many, the relief is worth it. One 15-year-old from Belfast told me, “I felt like I was underwater for months. After six weeks on Lexapro, I could breathe again.”
Medication works fastest for moderate to severe depression. If a teen can’t get out of bed, skip school, or has tried therapy without improvement, meds can be a lifeline.

Combining Both: The Best of Both Worlds
The Agency for Healthcare Research and Quality reviewed over 40 studies and found one clear pattern: combining family therapy and medication works better than either alone.
Therapy teaches coping skills, repairs relationships, and gives the teen a voice. Medication lifts the fog enough for them to use those skills. A 2023 Johns Hopkins cost analysis found that combined treatment saved money long-term-$12,500 per quality-adjusted life year versus $18,200 for meds alone. That’s because teens recover faster, relapse less, and stay in school.
And it’s not just clinical. In Reddit’s r/TeenDepression forum, 68% of 87 teens who said both therapy and meds helped reported “moderate to significant improvement.” The key? “My mom came to therapy with me. She didn’t just drop me off.”
What Doesn’t Work
Some families try “just talking it out” at home. Others wait for the teen to “snap out of it.” A 2009 NIH study found that teens from families rated as “healthy” had much higher recovery rates than those from “poor” family environments. That’s not luck-it’s structure, communication, and emotional safety.
Exercise and spirituality-based programs (like gratitude journals or forgiveness exercises) show modest benefits, but they’re not replacements. Same with online apps. The FDA approved a digital therapeutic called reSET-O in 2023, but it’s designed to support-not replace-therapy or meds.
And don’t assume one size fits all. A 2023 meta-analysis of nine trials found family therapy’s overall effect was small and inconsistent. Why? Because implementation varied wildly. Some therapists were trained. Others winged it. The difference between good family therapy and bad? Training. Certified therapists complete 40-60 hours of specialized training and 200+ supervised hours. Ask for credentials.
Barriers to Getting Help
Even when families know what to do, they often can’t get it.
There are only 8,500 certified child and adolescent family therapists in the U.S. for 42 million teens. Waitlists in many areas are 12-18 months long. Rural areas have even less access-only 19% use family therapy there versus 38% in cities.
Insurance doesn’t always help. While the 21st Century Cures Act requires mental health parity, many plans still limit sessions or require pre-authorization. And cultural stigma? Still real. In some communities, mental health is seen as weakness. Parents fear judgment. Teens fear being labeled.
That’s why early screening matters. The U.S. Preventive Services Task Force recommends all teens 12-18 be screened annually for depression. Schools that do this see a 27% increase in diagnosis-and faster access to care.
What to Do Next
If you’re worried about your child or teen:
- Start with a pediatrician. Ask for a depression screening.
- If symptoms are moderate to severe, consider both therapy and medication-not either/or.
- Look for therapists trained in ABFT, structural, or strategic family therapy. Ask about their certification.
- If meds are suggested, insist on weekly check-ins for the first month. Don’t skip them.
- Join a support group. NAMI and local parent networks are full of people who’ve been there.
- Call 988 if there’s any talk of suicide. It’s free, confidential, and available 24/7.
There’s no magic fix. But there’s hope. Families that stick with treatment-therapy, meds, or both-see real change. Not overnight. But steady. Lasting. Enough to let a kid grow up without depression defining them.
Can family therapy help if my teen refuses to talk?
Yes. Family therapy doesn’t require the teen to talk first. Therapists work with parents to change how they respond-reducing criticism, improving listening, and creating safer emotional space. Often, the teen starts opening up once the family dynamic shifts, even if they never say a word in session.
Are SSRIs safe for teens?
Fluoxetine and escitalopram are the only two antidepressants FDA-approved for teens, and they’re considered the safest options. While there’s a small increased risk of suicidal thoughts in the first few weeks, this risk drops significantly after month two. Close monitoring by a doctor makes it much safer. The benefits often outweigh the risks for moderate to severe depression.
How long does family therapy take to work?
Most families see small improvements in communication within 4-6 weeks. Significant changes-like reduced conflict, better trust, or a teen opening up-usually take 8-12 weeks. Full treatment typically lasts 12-16 sessions. Attachment-based therapy may take longer, up to 20 sessions, because it digs deeper into emotional bonds.
What if my teen hates therapy?
It’s common. Many teens resist therapy at first. The key is to keep showing up-even if they don’t. Therapists trained in family work know how to engage reluctant teens. Sometimes, just having a parent participate changes the dynamic enough for the teen to eventually join in. Don’t give up after one bad session.
Can my teen get better without medication?
Yes, especially for mild to moderate depression. Family therapy alone has shown consistent, though modest, symptom reduction. For some teens, improved family communication and structured support are enough. But for severe cases-where school is failing, self-harm is present, or the teen is suicidal-medication often becomes necessary to create the stability needed for therapy to work.





Kaylee Esdale
December 16, 2025 AT 19:31My sister went through this at 14. We did ABFT and it changed everything. Not because she started talking more, but because my mom finally stopped trying to fix everything and just sat with her. That silence? It spoke louder than any lecture.
Now she’s in college. Still has hard days. But she knows she’s not alone.
Chris Van Horn
December 18, 2025 AT 03:10While I appreciate the sentiment, the empirical foundation of Attachment-Based Family Therapy remains methodologically suspect. The 2022 Jefferson study cited exhibits significant selection bias and lacks longitudinal follow-up. One must interrogate the statistical power of n=47 before endorsing it as a first-line intervention. Furthermore, the FDA’s black box warning on SSRIs is not merely a caution-it is a constitutional imperative for clinical prudence.
Peter Ronai
December 18, 2025 AT 19:52Oh please. You think therapy fixes anything? My cousin’s kid was on Prozac for 6 months and still cried in the shower every night. Meanwhile, the family kept pretending everything was fine. No one wants to admit that sometimes, the problem isn’t the kid-it’s the whole damn system. And no therapist can fix that when dad’s still yelling at dinner about ‘entitlement.’
Medication’s a bandaid. But at least it lets the kid breathe long enough to realize they’re trapped.
Anu radha
December 20, 2025 AT 03:43I am from India. Here, many parents say depression is just laziness. But I saw my niece become quiet, stop eating, and sit all day. We took her to a therapist who worked with us too. Not easy. But we tried. Now she smiles again. Not always. But sometimes. That is enough.
Thank you for writing this.
Sachin Bhorde
December 21, 2025 AT 15:43From a clinical psych standpoint, the combo approach is gold standard-CBT + SSRIs + FST yields the highest remission rates (Cohen’s d = 0.82 in meta-analyses). But here’s the kicker: access inequality is systemic. In rural India, we’ve got 1 child psychiatrist per 500k kids. No insurance. No telehealth. So families default to ‘wait and see’… which is basically a death sentence for moderate-severe cases.
Screening in schools? Mandatory. Now.
Joe Bartlett
December 23, 2025 AT 11:48Prozac for teens? Bit mad if you ask me. We had it in the 90s and nobody went mad. Now everyone’s on pills and therapy. Maybe we need more discipline, not more drugs. My lad got moody, I told him to pull his socks up and go play football. He’s fine now.
Simple.
Marie Mee
December 25, 2025 AT 05:32Did you know the pharmaceutical companies paid off the FDA? That’s why they approved SSRIs for teens. They want you dependent. And the therapists? They’re paid by the hour. The system is rigged. My daughter stopped meds after 3 weeks and started journaling. She’s better now. No pills. No therapists. Just truth.
They don’t want you to know this.
Salome Perez
December 27, 2025 AT 02:33As a global mental health advocate, I’ve observed that cultural context is not an afterthought-it is the architecture of healing. In collectivist societies, family therapy is not an option; it is the only viable pathway. The Western emphasis on individualized pharmacotherapy often ignores the relational ecosystem in which depression is embedded.
Let us not export our biases as solutions.
Kent Peterson
December 27, 2025 AT 19:01Let’s be real: 8,500 therapists for 42 million teens? That’s not a shortage-it’s a failure of national priorities. We spend billions on military drones but can’t fund a single school counselor? And don’t get me started on insurance loopholes. This isn’t healthcare-it’s a luxury for the rich. The rest of us? We Google symptoms at 2 a.m. and hope the kid doesn’t wake up crying again.
And yes, I’ve read the studies. They’re all funded by pharma or universities with grant strings attached.
Josh Potter
December 29, 2025 AT 11:12Bro I was 16 and just didn’t care. Mom dragged me to therapy. I rolled my eyes. Then she started coming. Just sat there. Didn’t say a word. One day I blurted out I felt like a ghost.
That was the start.
Now I’m 21. Still on Lexapro. Still in therapy. But I’m alive. And that’s all that matters.
Evelyn Vélez Mejía
December 29, 2025 AT 16:28The ontological framing of depression as a biological disorder obscures its phenomenological roots: alienation, meaninglessness, and the collapse of intersubjective recognition. Pharmacological intervention may dampen the signal, but it does not restore the substrate of belonging. Family therapy, in its most authentic form, is an act of re-attachment-not merely a clinical protocol, but a moral reclamation of the child’s place within the familial narrative.
One cannot pharmacologize the soul.
Nishant Desae
December 30, 2025 AT 15:07Hey, I’m from India too. My brother was like this at 15. We didn’t know what to do. Tried home remedies, prayers, even a guru. Nothing worked. Then we found a local NGO that trained parents in basic ABFT techniques-just listening, no advice, no fixing. Took 3 months. But now he talks. He laughs. He even joined college. It’s not perfect. But it’s progress. To all parents reading: don’t wait for a crisis. Start small. Just sit with them. Even if they don’t talk. Just be there.
Love is the first medicine.
BETH VON KAUFFMANN
December 31, 2025 AT 06:00Let’s address the elephant: ABFT is not evidence-based-it’s trendy. The 2022 study had a control group that received ‘standard care,’ which was basically ‘check in every 3 weeks and hand out pamphlets.’ Of course ABFT looked better. It was the only intervention. Also, SSRIs? Overprescribed. Kids are being medicated for normal adolescent angst. The real crisis is our society’s refusal to tolerate discomfort. We need to stop pathologizing sadness.
Sam Clark
December 31, 2025 AT 16:47As a licensed clinical social worker with over 18 years in pediatric mental health, I can confirm that the data is unequivocal: integrated care yields superior outcomes. However, the greatest barrier remains stigma-not among clinicians, but among families who fear judgment. I’ve had parents cry in my office saying, ‘I didn’t know it was this serious.’
Let this be a call to action: normalize the conversation. Ask. Listen. Believe. And if you’re unsure, reach out to NAMI or 988. You are not alone.
Virginia Seitz
January 1, 2026 AT 21:56My daughter started therapy. We did meds. It worked. 🌱❤️