Medication Adherence Impact Calculator
How Digital Pill Sensors Improve Adherence
Digital pill sensors can boost adherence rates from typical 62% to 84% as shown in clinical studies. This calculator helps you understand the impact on your medication routine and potential healthcare savings.
How This Works
Based on clinical studies, digital pill systems can improve adherence from your current rate to an average of 84%. This means fewer missed doses, better health outcomes, and potential savings for healthcare systems.
Your Adherence Improvement
Example: If you take 30 doses per month at a $50 cost per dose, missing 10 doses could cost up to $500 in healthcare costs. Digital pill sensors can help reduce missed doses and associated complications.
What You Should Know
-
Adherence Improvement 22% increase
-
Cost Savings Estimate $150-$500 per year
-
Side Effect Detection Available in newer systems
-
Privacy Considerations Requires careful implementation
Imagine swallowing a pill and knowing, with certainty, whether it actually reached your stomach. Not guessing. Not hoping. Digital pill sensors make this real. They don’t just tell you if you took your medicine-they record exactly when, and even start spotting early signs your body is reacting badly to it. This isn’t science fiction. It’s happening right now in clinics and clinical trials across the U.S. and Europe.
How Digital Pills Actually Work
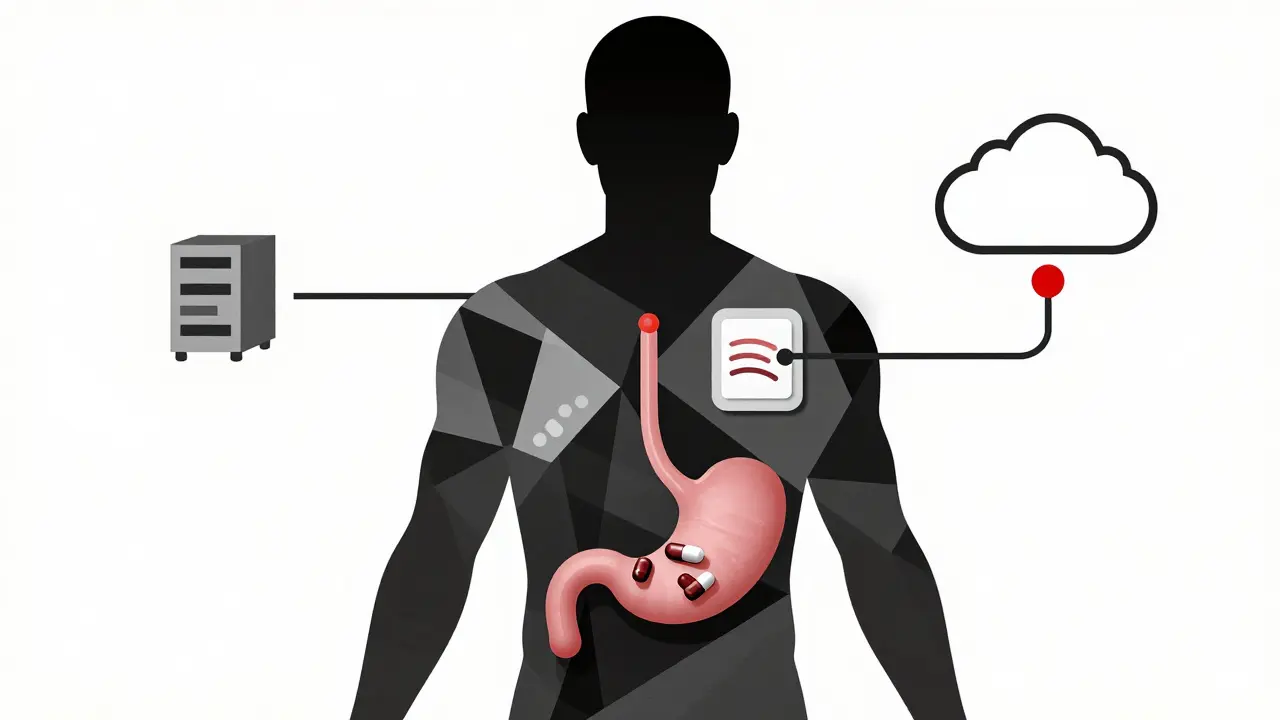
A digital pill looks like any other capsule. Inside, though, is a tiny sensor-about the size of a grain of sand. Made from copper and magnesium, it’s harmless and passes through your system like normal. When it hits stomach acid, the metals react. That reaction creates a tiny electrical pulse-enough to send a signal.
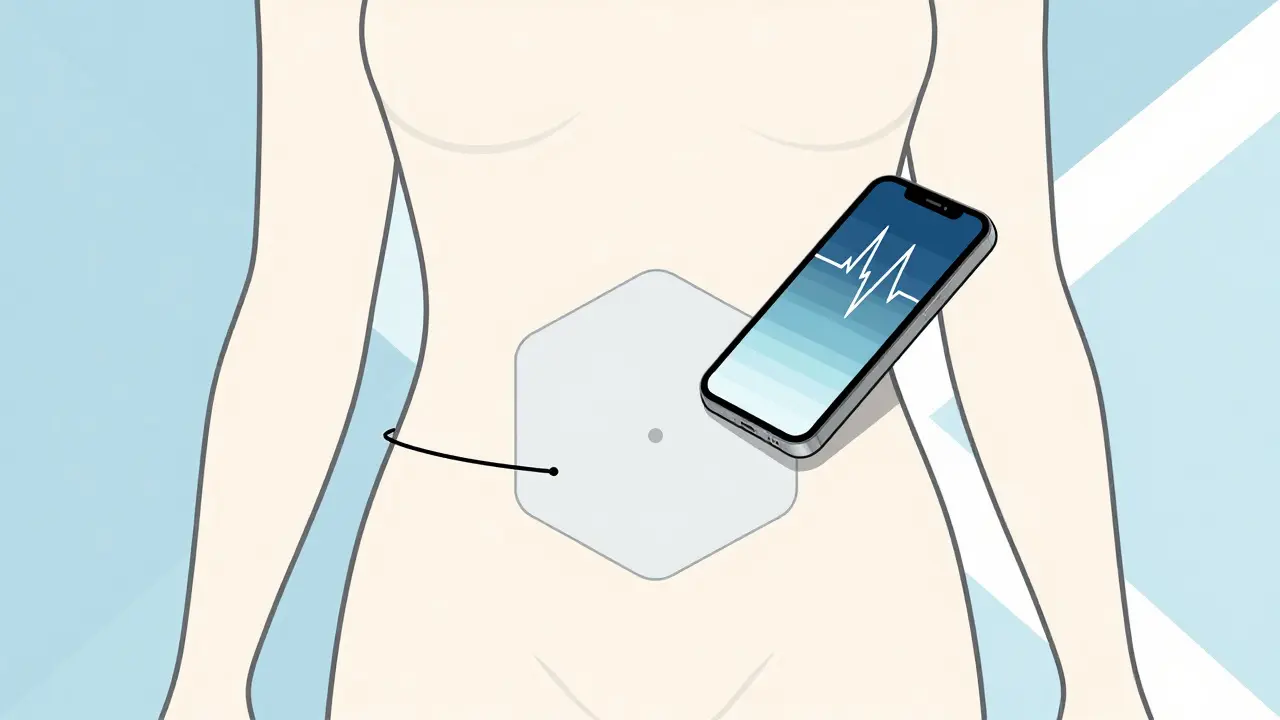
That signal gets picked up by a patch you wear on your skin, usually on your abdomen. The patch isn’t just a receiver. It also tracks your heart rate and how many steps you take each day. All of that data flows to your phone via Bluetooth, then up to a secure server. Your doctor or care team can see when you took your pill, and whether your body responded in real time.
The system has three parts: the sensor inside the pill, the wearable patch, and the app or web dashboard. It’s simple on the surface, but the tech behind it is precise. The sensor uses a Texas Instruments chip to send data, encrypted with AES standards so no one else can intercept it. The patch has a 72-hour battery life. After that, you swap it out. The whole setup takes about 15 minutes the first time-pairing the patch, logging into the app, syncing everything.
Why Adherence Rates Are So Low-And How This Changes That
Half of all people with chronic illnesses don’t take their meds as prescribed. That’s not laziness. It’s forgetfulness. It’s side effects. It’s cost. It’s fear. The World Health Organization has said this for years: poor adherence costs the U.S. healthcare system between $100 billion and $290 billion a year.
Digital pills cut through the guesswork. In a 12-week trial with patients on antipsychotics, adherence jumped from 62% to 84% when they used the sensor system. That’s not a small win. That’s life-changing for someone with schizophrenia or bipolar disorder. One Reddit user said, “Seeing the logs made me realize I skipped doses on weekends. I didn’t even know I was doing it.”
But it’s not just about remembering. It’s about trust. Some patients feel watched. In surveys, 73% of people hesitant to use the tech cited privacy as their top concern. Others said, “It feels like my doctor is watching me swallow.” That’s real. And it matters. The tech doesn’t judge-but the data can be misused if not handled carefully.
Side Effect Detection: Beyond Just Taking the Pill
The next big leap isn’t just tracking ingestion. It’s detecting how your body reacts to the drug. Newer systems, like those from Philips Research and etectRx, now monitor stomach pH levels and temperature. Why? Because some drugs cause inflammation, slow digestion, or trigger early signs of liver stress before symptoms show up.
For example, if a patient on a new antiviral for HIV starts showing a drop in stomach pH right after taking their pill, that could signal irritation before nausea or vomiting kicks in. That’s early warning. That’s prevention.
By 2026, 60% of digital pill systems are expected to include side effect detection as standard. IBM Watson Health is already working with etectRx to build AI models that predict adverse reactions based on patterns-like how your heart rate spikes 20 minutes after ingestion, or how your step count drops the day after a new dose. These aren’t guesses. They’re data-driven alerts.
One recent trial in tuberculosis treatment used this approach. Patients on the new drug pretomanid had sensors that flagged unusual temperature spikes. Doctors intervened early, adjusting dosages before patients developed severe liver toxicity. That’s the future: not just compliance, but protection.
Who’s Using This-and Who Isn’t
Right now, mental health leads the way. Nearly half of all digital pill deployments are for schizophrenia, bipolar disorder, or depression. Why? Because missing doses can lead to hospitalization. The stakes are high, and the benefits are clear.
HIV and cardiovascular disease are next. For HIV patients, missing even one dose can lead to drug resistance. Digital pills give providers real-time proof of adherence, which helps tailor support. For heart patients on blood thinners, knowing exactly when a dose was taken reduces the risk of dangerous interactions.
But for conditions like high blood pressure or mild diabetes? Adoption is slow. Why? Cost. Insurance doesn’t cover it. The pill itself costs $50-$100 per dose, plus the patch and app support. Most insurers won’t pay unless there’s proof it reduces ER visits or hospital stays-and that data is still being gathered.
Pharmaceutical companies are the biggest users. Seventy-eight percent of digital pill systems are in clinical trials. They use them to verify that patients in studies actually took the drug. That makes trial results more reliable. But for the average person? It’s still out of reach.
Real Problems, Real Limitations
This tech isn’t perfect. Signal loss happens. In 12-15% of cases, the patch doesn’t pick up the signal. Why? Body fat. If someone has a BMI over 35, the signal struggles to get through. Sensor orientation in the stomach matters too. If it lands sideways, the reaction might be delayed.
Then there’s the patch. Skin irritation is common. In one study, 22% of users quit because the adhesive burned or itched. Elderly patients, especially those over 65, struggle with the app. They need help pairing the patch. One geriatric trial found 38% needed family members to set it up.
And privacy? It’s the elephant in the room. The Electronic Frontier Foundation warns that this data could be sold to insurers or employers if regulations weaken. Right now, HIPAA protects it-but 14 U.S. states have added their own rules. That patch doesn’t just track pills. It tracks your movement, your heart, your daily rhythm. That’s intimate. And it’s not just your doctor who might want to see it.
What’s Next? AI, Regulation, and Wider Access
The market is growing fast. It was worth $628 million in 2022. By 2029, it could hit $2.4 billion. That growth isn’t accidental. It’s driven by two things: better tech and desperate need.
AI is the next frontier. Predictive models are learning which patients are likely to miss doses based on weather, sleep patterns, even their phone usage. If you usually take your pill at 8 a.m. but haven’t opened your app in three days? The system flags it. Not to punish you. To reach out.
Regulators are catching up. The FDA now requires separate approval for the drug and the sensor. That adds 22 months to the approval timeline. But it also means safety is built in. The first digital pill for tuberculosis got approved in March 2023. That opened the door for infectious disease use.
Reimbursement is the biggest barrier. Without insurance coverage, this stays a luxury. But as hospitals see fewer readmissions and fewer ER visits linked to missed doses, payers may start to pay. The Congressional Budget Office says costs need to drop 15-20% to make this sustainable at scale.
For now, digital pills are a tool for high-risk patients and clinical research. But the direction is clear: they’re becoming part of how medicine works-not because it’s flashy, but because it works.
What This Means for You
If you’re on a complex medication regimen-especially for mental health, HIV, or heart disease-ask your doctor if digital pills are an option. They’re not for everyone. But if you’ve struggled with adherence, or if your condition has serious consequences for missed doses, this could be a game-changer.
If you’re a caregiver, understand the privacy trade-offs. The data is secure, but it’s yours. Who sees it? Can you turn off real-time sharing? Can you delete logs? Ask those questions before you agree.
If you’re just curious? Keep watching. This isn’t just about pills. It’s about the future of personalized medicine-where your body’s response to treatment isn’t guessed at, but measured, tracked, and acted on in real time.
Are digital pill sensors safe to swallow?
Yes. The sensor is made from materials already used in dietary supplements-copper and magnesium. It’s small, smooth, and passes through your digestive system without being absorbed. It exits your body naturally in your stool within a few days. No surgery or removal is needed.
Can digital pills detect if I actually absorbed the medication?
No. They only confirm ingestion-when the pill reached your stomach. They can’t tell if the drug entered your bloodstream or if your liver processed it. That’s a limitation. Future versions may include biomarker sensors, but as of 2026, absorption data still requires blood tests.
Do I need a smartphone to use a digital pill system?
Yes. The wearable patch connects to a smartphone app via Bluetooth. The app sends data to the cloud and lets you view your adherence logs. If you don’t have a smartphone or can’t use one, most systems require a family member or caregiver to manage the app for you.
Can my insurance cover digital pills?
Most insurance plans don’t cover digital pills yet. They’re still considered experimental for most conditions. Coverage is mostly limited to clinical trials or specific mental health programs. Some Medicaid waivers and VA programs offer it for high-risk patients. Always check with your provider.
How long does the sensor last in my body?
The sensor activates only once-when it contacts stomach acid. It transmits for a few hours, then shuts off. It doesn’t recharge or keep working. It’s designed to pass through your system in 24-72 hours and exit naturally. No long-term presence.
Is this technology being used outside the U.S.?
Yes. The UK, Germany, Japan, and Australia have active pilot programs, especially in mental health and HIV care. The European Medicines Agency is reviewing approval pathways, and Canada has approved Abilify MyCite for use in select clinics. Adoption is slower than in the U.S. due to stricter privacy laws, but interest is growing.
What happens if I forget to wear the patch?
If you don’t wear the patch, the sensor in the pill still activates-but the signal won’t be picked up. You’ll get no notification, and your doctor won’t see the dose. The system only works when the patch is on. Some newer models have backup alerts that remind you to put it on, but you still need to wear it for data to be recorded.
Can I remove the patch if I don’t want to be tracked?
Yes. You can remove the patch at any time. But doing so stops data collection. Your doctor will see gaps in your adherence record, which may trigger a check-in. If you’re in a clinical trial, removing the patch could disqualify you. Always discuss privacy concerns with your care team before starting.
If you’re considering digital pills, start by talking to your doctor-not Google. This tech works best when it’s part of a support plan, not a surveillance tool. The goal isn’t to catch you skipping doses. It’s to help you stay well.







Beth Templeton
January 5, 2026 AT 07:40Matt Beck
January 7, 2026 AT 05:20Ryan Barr
January 8, 2026 AT 07:06Cam Jane
January 9, 2026 AT 12:00Tiffany Adjei - Opong
January 10, 2026 AT 09:04Stuart Shield
January 11, 2026 AT 13:26Dana Termini
January 11, 2026 AT 18:23Amy Le
January 12, 2026 AT 11:56Jeane Hendrix
January 13, 2026 AT 12:33Lily Lilyy
January 15, 2026 AT 11:45Katelyn Slack
January 16, 2026 AT 17:19