When a drug has a narrow therapeutic index, the difference between a dose that helps and one that kills is razor-thin. Theophylline is one of those drugs. Used for decades to treat asthma and COPD, it’s not a first-line choice anymore - but it’s still in use. And when it’s used, getting the level just right isn’t optional. It’s life-or-death.
What Makes Theophylline So Dangerous?
Theophylline works by relaxing airway muscles and reducing lung inflammation. But it doesn’t play nice. Its effective range? 10 to 20 mg/L. Go below 10, and it barely helps. Go above 20, and you’re flirting with seizures, irregular heartbeats, and even death. At 25 mg/L and up, the risk of fatal arrhythmias jumps sharply.
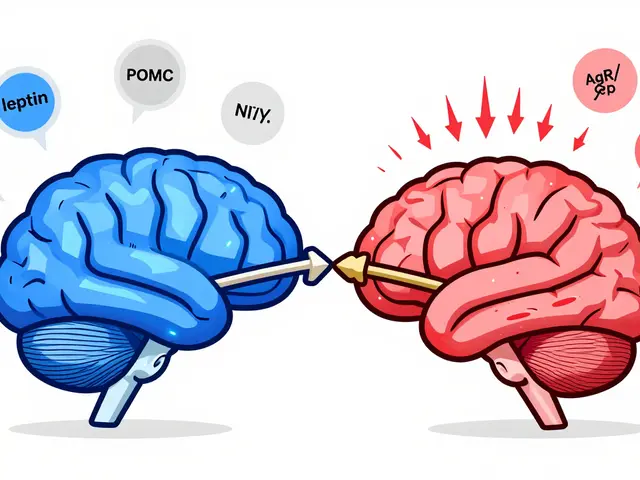
What makes this worse? Two things: how your body handles it, and what else you’re taking. Theophylline is broken down by your liver - but not everyone’s liver works the same. A smoker might clear it 50% faster than a non-smoker. Someone with liver disease? Their body might hold onto it like a sponge. And if they start taking an antibiotic like clarithromycin? That can spike theophylline levels by 100% in days.
Even small changes matter. A patient on 300 mg/day for months might feel fine. Then they quit smoking. Suddenly, their body can’t clear the drug like before. Levels creep up. They get nauseous. Then shaky. Then their heart starts racing. By the time they get to the ER, their level is 28 mg/L - and they’re in ventricular tachycardia.
Why You Can’t Guess the Dose
Doctors used to think: ‘Start at 200 mg, see how they do.’ That’s how it was done in the 1980s. Today, we know that’s reckless.
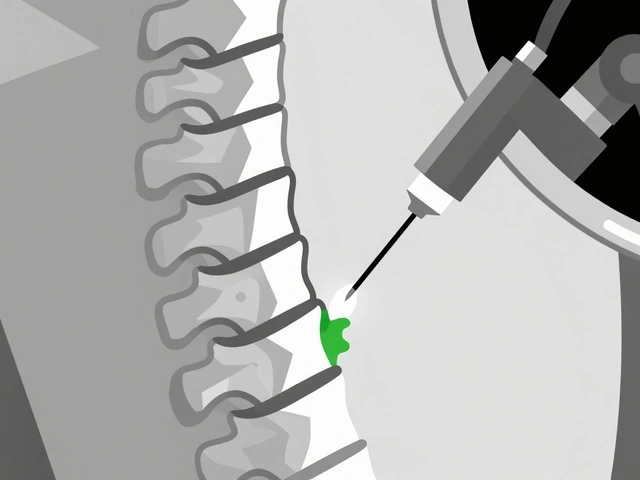
Theophylline doesn’t follow simple rules. Its metabolism shifts from first-order to zero-order kinetics as the dose increases. That means doubling the dose doesn’t just double the level - it might triple it. And it’s unpredictable across people. Age, weight, diet, liver function, heart failure, pregnancy - all of these change how the drug behaves.
Pregnant women? Clearance drops by 30-50% in the third trimester. Elderly patients? Liver function slows. That means the same dose that was safe at 45 might be toxic at 70. A 2023 case in Cureus showed a 68-year-old man with COPD develop life-threatening arrhythmia after starting ciprofloxacin. His theophylline level jumped from 14 mg/L to 28 mg/L in 72 hours. He survived - but barely.
And it’s not just antibiotics. Cimetidine, allopurinol, fluvoxamine - all slow theophylline breakdown. Carbamazepine, rifampin, St. John’s Wort? They speed it up. One patient on 400 mg/day might be fine. Another on the same dose, taking St. John’s Wort for depression? Their level could drop below 5 mg/L - and their asthma flares up. They think the drug isn’t working. They up the dose. And then… boom.
When and How to Test
You don’t test theophylline levels once and forget it. You test at key moments - and you test regularly.
- First test: 5 days after starting, or 3 days after a dose change. That’s when steady state kicks in.
- For immediate-release tablets: draw blood right before the next dose - that’s your trough level.
- For extended-release: wait 4-6 hours after the dose.
Stable patients? Test every 6-12 months. But if you’re over 60? Every 3-6 months. Heart failure? Every 1-3 months. Pregnant? Monthly in the second and third trimesters.
And never skip testing when something changes: new medication, stopped smoking, started drinking, got sick, lost weight, or started vomiting. Those aren’t just side effects - they’re red flags.
What Else to Watch For
Level alone isn’t enough. You need the full picture.
- Heart rate above 100 bpm? Watch for arrhythmias.
- Tremors, insomnia, headaches? Could be early toxicity.
- Low potassium? Theophylline and beta-agonists both pull it out of cells. Low K+ raises arrhythmia risk.
- Abnormal blood gases? Theophylline can cause hyperventilation - masking worsening lung disease.
- Full blood count? Rare, but theophylline can suppress bone marrow over time.
And if it’s IV? Never mix it with dextrose. It can cause hemolysis or fake clumping. That’s not a myth - it’s in the textbooks.
Real Results from Real Monitoring
One community hospital in Ohio implemented a strict theophylline monitoring protocol in 2021. They trained nurses, set up automatic alerts for out-of-range levels, and required lab checks before every refill.
Within 18 months:
- Adverse events dropped by 78%.
- Asthma control scores improved by 35%.
- ER visits for theophylline toxicity fell to zero.
Meanwhile, the NHS estimates that 15% of theophylline-related harms come from not adjusting for liver disease. Another 22% come from unmonitored drug interactions - especially with macrolide antibiotics.
Patients notice too. Surveys show 82% of long-term users say their symptoms are better when levels are in range. But 37% say the frequent blood tests are a hassle. That’s the trade-off. Convenience vs. safety.

Why It Still Matters in 2025
Newer inhalers, biologics, and monoclonal antibodies are expensive. Theophylline? A generic bottle costs $15-$30 a month. That’s why it’s still used - especially in low-resource areas, or for patients who can’t afford newer drugs.
But cost doesn’t make it safe. In fact, the lower price might make people think it’s harmless. It’s not. Poison control centers in the U.S. reported a 23% yearly rise in theophylline toxicity cases from 2020 to 2023. Most were elderly patients with undiagnosed kidney or liver problems.
There are new tools coming - handheld devices that can measure theophylline from a finger prick in under five minutes. Companies like TheraTest Diagnostics and PharmChek Solutions are in Phase 2 trials. But until those are widely available and proven, the old way is still the only safe way: blood tests.
The American College of Chest Physicians says it plainly: ‘Until such technologies become widely available and validated, traditional serum concentration monitoring remains the standard of care for all patients receiving theophylline therapy.’
The Bottom Line
Theophylline isn’t a drug you prescribe and forget. It’s a drug you monitor - constantly, carefully, and with full awareness of what else the patient is taking, how their body is changing, and how close they are to the edge.
That narrow window - 10 to 20 mg/L - isn’t a suggestion. It’s a boundary. Cross it, and the risks aren’t just side effects. They’re emergencies.
If you’re on theophylline, get your levels checked. If you’re prescribing it, don’t assume. Test. Adjust. Re-test. Because when the margin between help and harm is this small, there’s no room for guesswork.




Rachel Whip
November 26, 2025 AT 02:13Theophylline is one of those drugs that makes you appreciate how much pharmacology has evolved. I’ve seen patients on it for decades-some with perfect control, others crash into the ER with no warning. The key isn’t just the level-it’s knowing their whole story. Smoking status? Liver enzymes? What meds they’re secretly taking? That’s where the real work happens.
One time, a 72-year-old woman on 300 mg/day was fine until she started taking cipro for a UTI. No one asked about OTC stuff. Level went from 14 to 26 in 4 days. She didn’t even know cipro could do that. We almost lost her.
Ali Miller
November 27, 2025 AT 12:00Let’s be real-this drug is a relic. 🤦♂️ We’ve got inhalers that work better, safer, and don’t require a blood test every other Tuesday. Why are we still clinging to this 1950s relic like it’s some kind of medical tradition? It’s not ‘cost-effective’-it’s negligence dressed up as pragmatism.
And don’t get me started on the ‘it’s still used in low-resource areas’ excuse. That’s just lazy healthcare systems hiding behind poverty. We can do better. We just choose not to.
JAY OKE
November 27, 2025 AT 23:00I work in a rural clinic. We still use theophylline because it’s cheap and our patients can’t afford biologics. But we don’t guess. We test. Every 3 months for stable folks, monthly if they’re older or have heart issues. It’s a hassle, sure-but it’s cheaper than an ambulance ride.
One guy quit smoking, didn’t tell anyone, kept taking his 400 mg. Got dizzy, thought it was just ‘getting old.’ We caught it because his next test was due. Level was 23. He cried when we told him how close he was. We adjusted, he’s fine now.
Joe bailey
November 29, 2025 AT 00:31Love this breakdown 👏 Seriously, this is the kind of post that reminds me why I got into healthcare. Theophylline isn’t dangerous because it’s bad-it’s dangerous because we forget how delicate the balance is.
My grandma was on it for years. We did her levels every 6 months like clockwork. She never had an issue. It wasn’t magic-it was consistency. And yeah, the blood draws sucked. But she lived to 92. I’ll take the prick over the panic any day.
Also-St. John’s Wort? Yeah, it’s ‘natural’ but it’s basically a drug thief. Always ask about supplements. Always.
Sanjay Menon
November 29, 2025 AT 18:52While the clinical data presented is, of course, statistically significant and clinically relevant, one cannot help but notice the implicit bias toward institutionalized, Western medical paradigms. Theophylline, in many global contexts, is not merely a drug-it is a cultural artifact of pharmaceutical colonialism.
Whereas Western clinicians obsess over serum concentrations, indigenous systems often integrate herbal adjuvants, breathwork, and circadian rhythm alignment to modulate bronchial tone. The reductionist focus on ‘10–20 mg/L’ ignores the phenomenological experience of the patient, which, in my view, is the true therapeutic metric.
Furthermore, the claim that ‘traditional serum concentration monitoring remains the standard of care’ is not a scientific conclusion-it is a hegemonic assertion.
Brittany Medley
November 29, 2025 AT 22:20Just wanted to add: if you’re testing trough levels, make sure the patient hasn’t eaten a huge meal right before. Fat can delay absorption and throw off your timing. Also-don’t assume ‘stable’ means ‘safe.’ I had a patient whose level dropped to 4.2 because she started drinking grapefruit juice daily. No one asked. She had a near-fatal exacerbation.
And yes, the blood draws are annoying. But so is being intubated. I’d rather have a needle than a ventilator.
Kaushik Das
December 1, 2025 AT 19:27Bro this is wild. I used to work in a pharmacy in Delhi-we’d sell theophylline like candy. No script, no test. One guy came back 3 weeks later with tremors, heart racing-he’d been doubling his dose because he thought ‘it wasn’t working.’ We got him to the hospital just in time.
Now I tell every patient: ‘This ain’t ibuprofen. This is a knife. You need to know exactly how sharp it is.’ And yeah, if they’re on antibiotics? Stop the theo till you check. No exceptions.
Also-St. John’s Wort? Even if they say ‘it’s just tea,’ I still ask. People lie. We all do.
mohit passi
December 3, 2025 AT 05:40