Carb Counter & Dose Calculator for Alpha-Glucosidase Inhibitors
Calculate your daily carb intake to determine the right starting dose and minimize gas, bloating, and diarrhea from alpha-glucosidase inhibitors like acarbose and miglitol. Follow the guidelines in the article for successful management.
Carb Intake Calculator
Dose Adjustment Guide
No calculation performed yet
Slow Titration Schedule
Dietary Recommendations
Foods to Limit
- White bread
- Potatoes
- Sugary snacks
- Rice (limit portion size)
Better Alternatives
- Whole grains
- Beans and lentils
- Vegetables
- Lean proteins
When you're trying to control your blood sugar after meals, alpha-glucosidase inhibitors like acarbose and miglitol can seem like a smart choice. They don’t cause low blood sugar. They don’t make you gain weight. And for people who eat a lot of rice, bread, or potatoes, they work well. But there’s a catch - for most people, the side effects are brutal. Gas. Bloating. Diarrhea. Sometimes all three at once.
Why Do These Drugs Cause So Much Gas?
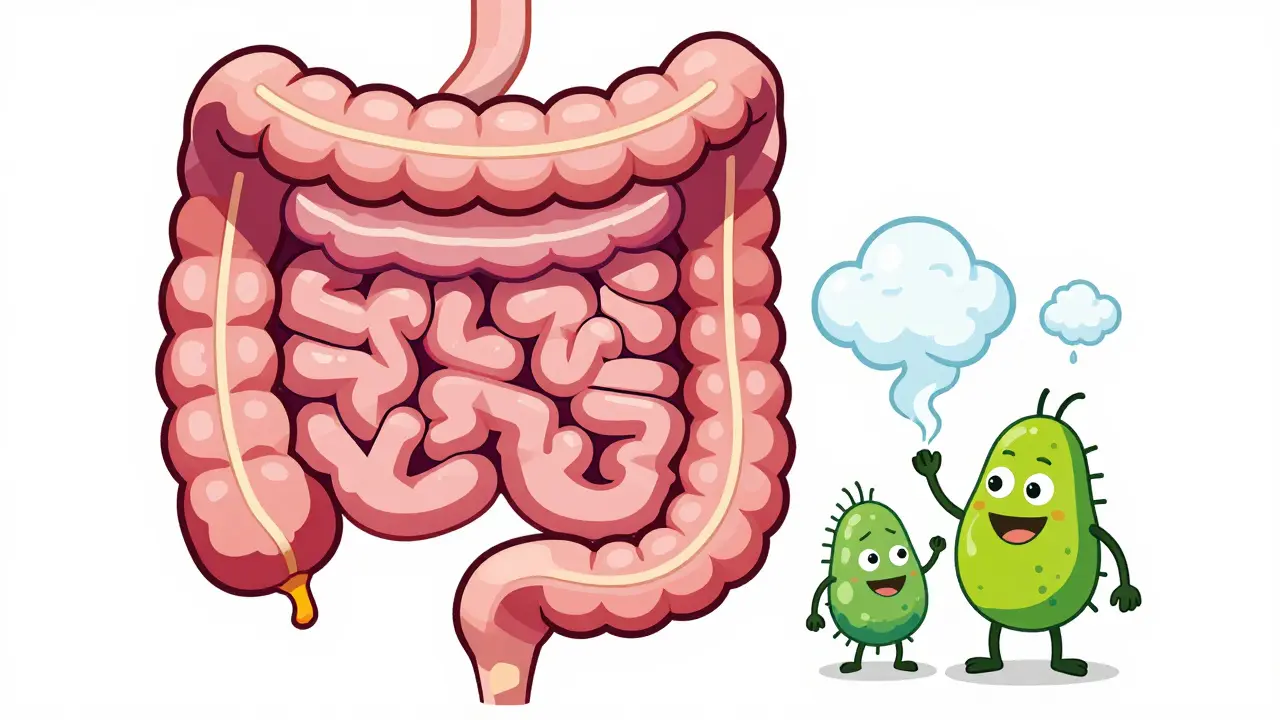
Alpha-glucosidase inhibitors don’t get absorbed into your bloodstream. That’s actually why they’re safe for kidneys and don’t cause low blood sugar. But here’s the problem: they stay in your gut. They block the enzymes that break down complex carbs like starches and sugars in your small intestine. So instead of being digested, those carbs move straight into your colon.
That’s where your gut bacteria come in. They love undigested carbs. They feast on them. And when they do, they produce gas - lots of it. Hydrogen, methane, carbon dioxide. The kind of gas that makes you feel like your stomach is a balloon about to pop. In clinical trials, up to 73% of people on acarbose had severe flatulence in the first month. It’s not rare. It’s normal.
How Bad Is the Bloating and Diarrhea?
Gas is bad enough. But bloating? That’s worse. You start feeling full after just a few bites. Your clothes feel tight. You avoid social meals because you’re scared of what’s going to happen next. Then comes the diarrhea. Not the occasional loose stool - we’re talking urgent, frequent, watery bowel movements. Around 10-20% of users develop diarrhea within the first few weeks. For some, it lasts for months.
One user on Reddit said: “I started acarbose at 50 mg three times a day. Within three days, I was running to the bathroom after every meal. I couldn’t even sit through dinner with my family.” That’s not an outlier. A 2020 study in the Journal of Diabetes Research found that 30% of people stopped taking these drugs within three months because of gut symptoms.
Who Still Uses These Drugs Today?
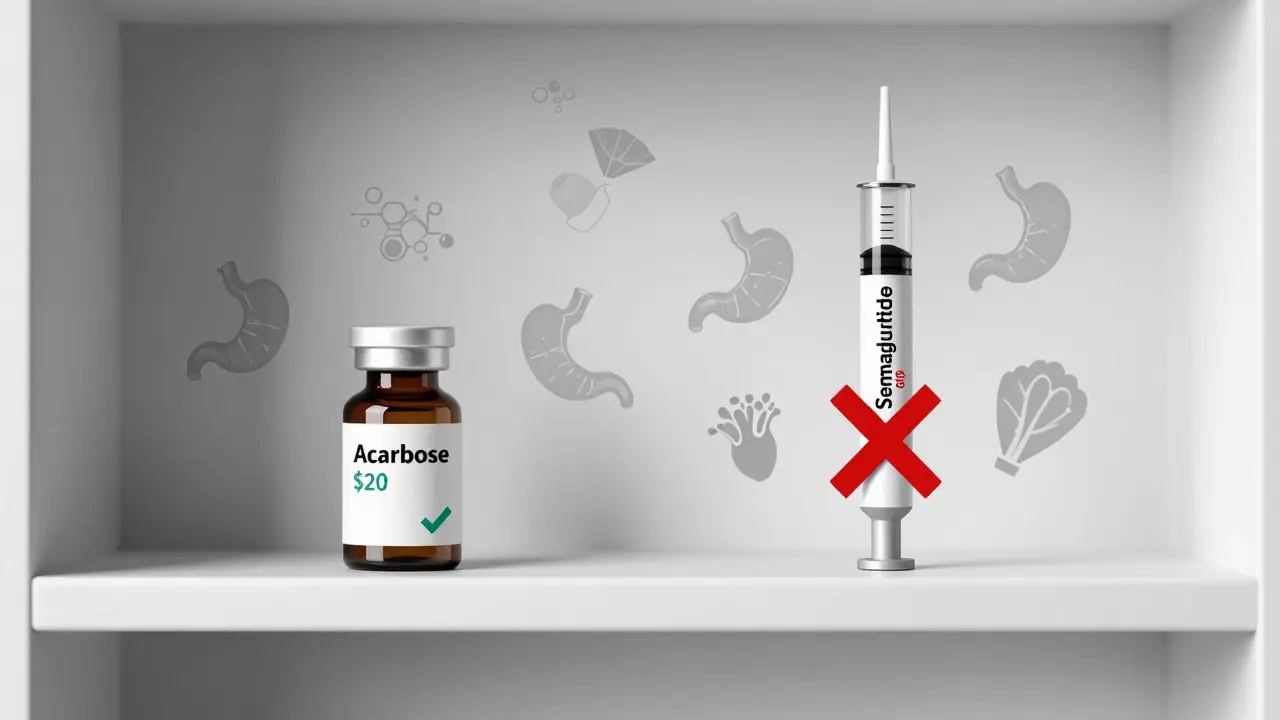
Not many. In the U.S., alpha-glucosidase inhibitors make up less than 3% of all diabetes prescriptions. That’s down from over 5% just six years ago. Newer drugs like GLP-1 agonists and SGLT2 inhibitors are more effective, easier to take, and have fewer stomach problems.
But they’re not gone. Doctors still prescribe them - mostly for older adults, people with kidney issues, or those who can’t afford newer medications. Acarbose costs about $15 to $25 a month as a generic. Compare that to $500+ for a monthly supply of semaglutide. For someone on a fixed income, that difference matters.
They’re also still used in Asia. In China and India, where meals are heavy in rice and noodles, these drugs are more common. The diet matches the drug’s mechanism. In Western countries? Not so much.

Can You Make the Side Effects Bearable?
Yes - but only if you do it right. Most people fail because they start too fast. The key is slow, slow, slow.
- Start with 25 mg once a day, with your biggest meal.
- Wait two weeks. If you’re not too miserable, go to 25 mg twice a day.
- After another two weeks, try 25 mg three times a day.
This isn’t just advice - it’s backed by clinical trials. People who titrated slowly had half the dropout rate compared to those who jumped straight to the full dose.
Diet changes are just as important. You need to cut back on the carbs that these drugs are designed to slow down. That means:
- White bread? Avoid it.
- Potatoes? Limit them.
- Sugary snacks? Cut them out.
- Instead: choose whole grains, beans, lentils, and vegetables.
Try to keep each meal to 30-45 grams of carbs. That’s about one small slice of whole grain bread, half a cup of brown rice, and a cup of broccoli. It’s not easy, but it cuts gas and diarrhea by 40-50% in most people.
What About Over-the-Counter Remedies?
Don’t take Beano. It sounds like it should help - it’s an enzyme that breaks down carbs, right? But Beano contains alpha-galactosidase. That’s the same enzyme that acarbose blocks. So Beano fights your medication. It defeats the whole purpose.
Simethicone (Gas-X, Mylanta Gas) might help a little with bloating. It doesn’t stop gas production, but it breaks up bubbles so you feel less pressure. Take 125 mg right before meals.
For diarrhea, loperamide (Imodium) is okay to use occasionally. But don’t rely on it. It masks the problem, doesn’t fix it. And if you’re having diarrhea every day, you need to rethink your dose or your diet.
Do the Side Effects Ever Get Better?
They can. Your gut microbiome adapts. After 8 to 12 weeks, many people notice a big drop in symptoms. One user on Drugs.com wrote: “Month one was hell. Month three? I could eat a bowl of oatmeal without feeling like I was going to explode.”
But here’s the thing: that improvement only happens if you stick with the slow titration and the low-carb diet. If you keep eating pasta and cookies, your gut won’t adapt. It’ll keep screaming at you.
Is It Worth It?
That depends. If your HbA1c is stuck at 8.5% and you can’t tolerate metformin or GLP-1 drugs, then yes - it might be worth a shot. These drugs can lower post-meal sugars by 40-50 mg/dL. That’s meaningful.
But if you’re young, active, and have access to newer medications? Probably not. The side effects are too harsh, and the benefits are modest. Most people end up quitting anyway.
And here’s a hard truth: even if you stick with it, you’re still more likely to have embarrassing, uncomfortable days than to feel great. You’re trading one problem (high blood sugar) for another (constant gut misery). For some, that’s a fair trade. For most, it’s not.
What Should You Do If You’re Starting These Drugs?
- Ask your doctor for a 25 mg starting dose - not 50 mg.
- Get a dietitian’s advice on low-glycemic meals.
- Keep a symptom journal: rate your gas, bloating, and diarrhea on a scale of 1 to 10 every day.
- Don’t expect miracles in the first week. Give it 8 weeks.
- If you’re still miserable after 12 weeks, talk about switching.
These drugs aren’t evil. They just have a brutal side effect profile. And if you’re not prepared for it, you’ll quit - and your blood sugar will suffer.
Final Thought
There’s a reason these drugs are fading out of mainstream use. They work - but at a cost most people aren’t willing to pay. If you’re considering them, go in with your eyes open. Know what you’re signing up for. And if your doctor pushes them without explaining the gut issues? Ask for alternatives. There are better options now.
Do alpha-glucosidase inhibitors cause low blood sugar?
No, not when taken alone. Unlike sulfonylureas or insulin, alpha-glucosidase inhibitors don’t trigger insulin release. They just slow down carb digestion. That means your blood sugar rises more slowly and doesn’t crash. But if you take them with other diabetes meds like insulin or sulfonylureas, you can still get low blood sugar - and you won’t be able to fix it with regular sugar. You’ll need glucose tablets or gel because table sugar won’t be absorbed fast enough.
Can I take these drugs if I have IBS?
Generally, no. If you already have irritable bowel syndrome (IBS), especially with diarrhea-predominant symptoms, alpha-glucosidase inhibitors will likely make things much worse. The extra gas, bloating, and loose stools can turn a manageable condition into a daily struggle. Most doctors avoid prescribing them to people with IBS unless there are no other options.
How long does it take for the side effects to go away?
For many people, the worst symptoms improve after 6 to 12 weeks. That’s when your gut bacteria start adapting to the undigested carbs. But this only happens if you stick with a low-carb diet and don’t increase your dose too fast. If you keep eating white rice or pastries, the symptoms won’t get better - they’ll just get worse.
Is there a better alternative to acarbose for post-meal sugar spikes?
Yes. GLP-1 receptor agonists like semaglutide or dulaglutide are more effective at lowering post-meal glucose and cause less gas. But they’re injectable and expensive. SGLT2 inhibitors like empagliflozin are pills and have minimal gut side effects, but they carry a small risk of dehydration and yeast infections. For people who can’t use those, metformin is still the first choice - though it causes nausea, not bloating.
Can probiotics help with the gas and bloating?
Some evidence says yes. A 2023 trial found that taking acarbose with specific probiotics - Lactobacillus acidophilus and Bifidobacterium lactis - reduced flatulence by 35%. The probiotics didn’t stop the gas, but they changed the kind of gas produced, making it less smelly and less bloating. You can try a high-quality probiotic with these strains, but don’t expect it to fix everything. Diet and dosing still matter most.
Why do these drugs work better in Asian populations?
Because Asian diets are typically higher in complex carbohydrates like rice, noodles, and steamed buns - the exact foods these drugs are designed to slow down. In Western diets, carbs come more from bread and sweets, which are easier to manage with other medications. In Asia, where rice is eaten at every meal, slowing its digestion makes a bigger difference in blood sugar control. That’s why they’re still commonly used there.





Phil Maxwell
January 23, 2026 AT 15:33I started acarbose last year after metformin wrecked my stomach. Honestly? Month one was a nightmare - I thought I was dying. But I stuck with the slow titration like the post said, cut out white bread and rice, and by week 8, I could eat a bowl of oatmeal without feeling like a balloon. Still get a little gassy after curry, but hey - my A1c dropped from 8.2 to 6.4. Worth the awkward dinners.
Luke Davidson
January 24, 2026 AT 06:27Bro this is the most real thing I’ve read about diabetes meds in years. I was about to quit acarbose after two weeks of pure chaos - then I found this. Started at 25mg once a day, swapped white rice for lentils, and now I’m at 3 months with zero diarrhea. My grandma even asked if I lost weight. I told her I just stopped eating like a 12-year-old on a sugar binge. 🙌
Patrick Gornik
January 24, 2026 AT 08:21Let’s be real - alpha-glucosidase inhibitors are the pharmaceutical equivalent of forcing a dragon to digest hay. They’re not broken, they’re just tragically mismatched with modern diets. The gut microbiome isn’t some passive plumbing system - it’s a warzone where undigested starches are the chemical weapons, and your colon is the frontline. We’re not treating diabetes here; we’re negotiating a ceasefire between evolution and industrialized carbs. And honestly? Most people don’t have the discipline to win that war. They want the sugar without the consequence. But biology doesn’t do loopholes. It just retaliates with methane.
Karen Conlin
January 24, 2026 AT 09:57As someone who’s helped 30+ patients navigate this exact issue, I can’t stress enough: the slow titration isn’t optional - it’s the difference between adherence and abandonment. And yes, probiotics with L. acidophilus and B. lactis? They’re not magic, but they’re the closest thing we’ve got to a peace treaty with your gut. Pair that with a dietitian who knows how to build a low-glycemic plate that doesn’t taste like cardboard, and you’ve got a real shot. Don’t give up - just pivot.
asa MNG
January 26, 2026 AT 09:31omg i tried this and it was like my intestines were having a rave with no bouncer 😭 i was running to the bathroom after every burrito. then i started taking gas-x before meals and it was like a miracle. also i switched to quinoa instead of rice and now i can watch tv without sweating through my pants. thx for saving me 🙏💖
blackbelt security
January 26, 2026 AT 22:04These drugs are a relic. If your doctor’s still pushing acarbose without mentioning GLP-1s or SGLT2s, they’re either stuck in 2012 or you’re on Medicaid. Don’t suffer for $20 a month when you could be on a $500 drug that lets you eat pizza without fear. Your future self will thank you.
Sushrita Chakraborty
January 28, 2026 AT 15:52In India, where rice is consumed at every meal, these medications remain clinically relevant - not due to economic constraints alone, but because of dietary patterns that align precisely with their pharmacological mechanism. The reduction in postprandial glucose spikes is statistically significant in populations consuming >200g of carbohydrates per meal. However, adherence remains low due to inadequate patient counseling regarding titration and carbohydrate modification. This is a systemic failure in education, not a flaw in the drug itself.
Tommy Sandri
January 28, 2026 AT 16:32The cultural and dietary context surrounding the use of alpha-glucosidase inhibitors cannot be overstated. In Western nations, where dietary guidelines have shifted toward low-carbohydrate paradigms, these agents naturally fall out of favor. In contrast, in East and South Asia, where carbohydrate-rich staples are culturally entrenched, the pharmacodynamic profile of these drugs remains highly congruent with habitual intake. This is not merely a matter of cost or convenience - it is a reflection of pharmacology meeting cultural nutrition.
Heather McCubbin
January 29, 2026 AT 09:01Let’s be honest - if you’re still on acarbose, you’re probably just too lazy to get a GLP-1 prescription or too broke to afford it. Everyone knows these drugs are a nightmare. You’re not brave for sticking with it - you’re just stubborn. And your gut knows it. Stop pretending this is a noble sacrifice. It’s just bad medicine wrapped in a ‘I’m too poor to be modern’ cape.
Sawyer Vitela
January 31, 2026 AT 01:3873% flatulence? 30% dropout? Then why is this even a thing? It’s not a treatment - it’s a test of endurance. If your drug makes you a social pariah, it’s not working. It’s failing. Move on.