When you're breastfeeding and hit with a cold or allergies, the last thing you want is to choose between feeling better and keeping your baby safe. Many moms assume that if a medicine is sold over the counter, it’s fine to take while nursing. But that’s not always true. Some common cough and allergy medications can make your baby dangerously sleepy - even after just one dose.
Why Some Medications Are Risky During Breastfeeding
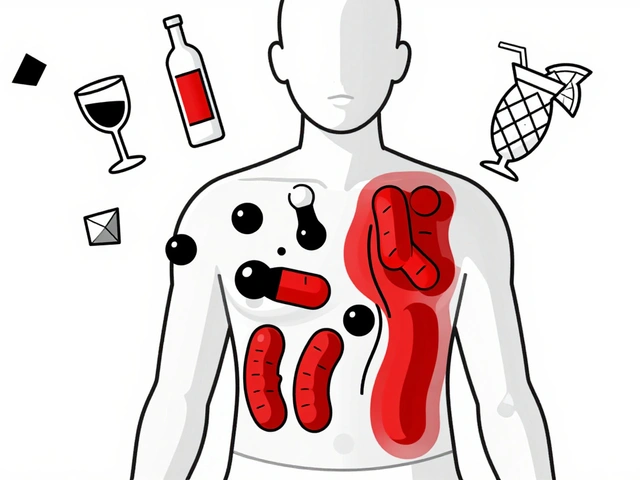
Not all drugs pass into breast milk the same way. What matters isn’t just whether a drug gets into your milk, but how much of it reaches your baby’s bloodstream and what it does to their tiny body. Babies, especially under 2 months old, have immature livers and kidneys. They can’t break down or flush out medications like adults can. That means even small amounts of certain drugs can build up and cause serious side effects. The biggest concern? Sedation. If your baby becomes too sleepy, they might not wake up to feed. That leads to poor weight gain, dehydration, and in extreme cases, respiratory depression - where breathing slows to dangerous levels. This isn’t theoretical. There are documented cases of infants dying after maternal use of codeine for postpartum pain. One 13-day-old baby passed away after the mother took codeine for pain after delivery. The drug converted to morphine in her system, passed into her milk, and overwhelmed her baby’s system.Codeine: A Medication You Must Avoid
Codeine used to be a go-to for coughs and pain. Now, it’s a red flag. The FDA issued a black box warning in 2017 because some people are “ultra-rapid metabolizers.” These individuals turn codeine into morphine much faster than normal - up to 20 times more. About 1 in 100 Caucasian people fall into this group. You can’t tell who they are without genetic testing. Even if you’re not an ultra-rapid metabolizer, codeine still transfers into breast milk at levels that can affect infants. Studies show infant serum morphine levels can hit 30 ng/mL after a standard maternal dose - enough to cause slowed breathing and deep sleep. The Breastfeeding Network, the American Academy of Pediatrics, and the Academy of Breastfeeding Medicine all now say: do not use codeine while breastfeeding. It’s no longer listed as a safe option in clinical guidelines.First-Generation Antihistamines: The Hidden Danger
Diphenhydramine (Benadryl), chlorpheniramine, and hydroxyzine are common in allergy and cold meds. They work well for runny noses and itchy eyes - but they’re also strong sedatives. These drugs cross into breast milk easily, with milk-to-plasma ratios as high as 1.0. That means your baby could be getting nearly as much of the drug as you are, per pound of body weight. A Motherisk study found that 1.6% of infants exposed to diphenhydramine became noticeably sleepy. That might sound low, but in a population of thousands of nursing mothers, that’s dozens of babies every week who become too drowsy to feed properly. On Reddit, a mom shared that her 6-week-old became “excessively sleepy” and wouldn’t wake for feeds after she took one Benadryl. The ER confirmed it was likely the medication. These drugs are classified as L2-L3 by the American Academy of Pediatrics - meaning they’re possibly unsafe. The Royal Women’s Hospital in Australia explicitly warns: “Sedating antihistamines are not recommended because the medicine may pass into your breast milk and make your baby drowsy.”Safer Alternatives: What You Can Take Instead
The good news? There are plenty of safe, effective options that won’t make your baby sleepy.- Cetirizine (Zyrtec) - Transfers at only 0.14% of your dose. No sedation reported in infants at standard doses. L1 safety rating.
- Loratadine (Claritin) - Even less transfer - just 0.04-0.05% of your dose. Minimal to no effect on babies. Also L1.
- Fexofenadine (Allegra) - Non-sedating, low transfer. Safe for daily use while nursing.

Decongestants and Nasal Sprays: What to Watch Out For
Pseudoephedrine (Sudafed) doesn’t make babies sleepy - but it can dry up your milk supply. A 2003 study found a 24% drop in milk production within 24 hours of taking it. That’s enough to derail breastfeeding for many moms. Avoid it unless you’re already pumping and storing milk, or you’re weaning. Nasal steroids like fluticasone (Flonase) and budesonide (Rhinocort) are a better choice. They’re applied right where you need them - inside your nose. Less than 0.1% of the dose enters your bloodstream, so almost none reaches your milk. The AAFP calls them first-line treatment for allergic rhinitis during breastfeeding. Saline nasal sprays and neti pots? Completely safe. No drugs. No risks. Just rinse out the allergens.What About Cough Suppressants?
Dextromethorphan, the main ingredient in many cough syrups, is one of the safest options. It transfers into breast milk at only 0.1% of your dose. No documented cases of sedation in infants. The InfantRisk Center gives it an L1 rating - the safest category. Avoid cough syrups that combine dextromethorphan with antihistamines or decongestants. Read labels carefully. “Multi-symptom” formulas often hide diphenhydramine or pseudoephedrine. Stick to plain dextromethorphan-only products.How to Time Your Medication for Maximum Safety
If you must take a medication with any risk, timing matters. Take it right after you breastfeed, not before. That gives your body time to clear some of the drug before the next feeding. For drugs like diphenhydramine (half-life 4-6 hours), waiting 3-4 hours before nursing cuts infant exposure by more than half. If your baby sleeps for 4-5 hours at night, take your dose right before bed. That way, the highest drug levels in your milk coincide with their longest stretch of sleep. Don’t pump and dump unless you’re taking something like codeine or a high-risk drug. Pumping doesn’t speed up clearance - it just removes milk you’ll need to replace. And it can lower your supply over time.
Watch for These Signs in Your Baby
Even with the safest meds, keep an eye out. Call your pediatrician if your baby shows:- Excessive sleepiness - harder than usual to wake for feeds
- Reduced feeding frequency - skipping feeds or taking less milk
- Shallow or irregular breathing
- Lack of responsiveness - not reacting to your voice or touch
What’s Changed in the Last Few Years
The landscape has shifted dramatically. In 2018, only 9 cough and allergy meds had sedation warnings in the LactMed database. Today, that number is 17. The FDA now requires black box warnings on codeine products. Over-the-counter brands have responded - 68% of allergy meds now offer non-drowsy versions, up from 42% in 2015. New tools like the LactaMap app give real-time, personalized safety info based on your baby’s age and your medication. Pharmacogenetic testing for codeine metabolism is now available in some hospitals - though it’s not yet routine.Bottom Line: Safer Choices Exist
You don’t have to suffer through allergies or a cough while breastfeeding. You just need to know what to reach for.- Avoid: Codeine, diphenhydramine, chlorpheniramine, pseudoephedrine
- Use: Cetirizine, loratadine, fexofenadine, dextromethorphan, nasal steroids, saline sprays
- Time: Take meds right after feeding, wait 3-4 hours if possible
- Watch: For signs your baby is too sleepy or not feeding well




![Buy Generic Lexapro (Escitalopram) Online Cheap-Safe UK Options, Prices, and Checks [2025]](/uploads/2025/09/thumbnail-buy-generic-lexapro-escitalopram-online-cheap-safe-uk-options-prices-and-checks.webp)

Tina Dinh
December 1, 2025 AT 13:05LINDA PUSPITASARI
December 3, 2025 AT 01:05Joy Aniekwe
December 3, 2025 AT 03:08Latika Gupta
December 3, 2025 AT 18:16Sullivan Lauer
December 4, 2025 AT 08:15Sohini Majumder
December 6, 2025 AT 06:21tushar makwana
December 7, 2025 AT 15:52Richard Thomas
December 7, 2025 AT 22:10Matthew Higgins
December 9, 2025 AT 15:38Mary Kate Powers
December 11, 2025 AT 13:58Sara Shumaker
December 13, 2025 AT 09:50Steven Howell
December 13, 2025 AT 13:30Robert Bashaw
December 15, 2025 AT 00:14