When your kidneys aren’t working right, even common medications can turn dangerous. It’s not just about taking less of a pill - it’s about knowing which pills to avoid, when to change the dose, and how to spot trouble before it’s too late. For the 37 million Americans with chronic kidney disease (CKD), medication safety isn’t a side note - it’s the core of staying alive and avoiding dialysis.
Why Kidneys Matter More Than You Think
Your kidneys don’t just filter waste. They handle drug clearance. About 70% of all prescription medications leave your body through the kidneys. When kidney function drops - say, from an eGFR of 90 down to 40 - those drugs build up. That’s when side effects turn serious: nausea, confusion, irregular heartbeat, or even sudden kidney failure.
Many people don’t realize this. A 2022 study in JAMA Internal Medicine found that nearly 24% of CKD patients were given medications at doses that could harm them. Why? Because most doctors don’t have kidney dosing built into their workflow. Electronic health records often don’t flag when a drug is risky for someone with an eGFR under 60. And patients? They’re taking over-the-counter painkillers like it’s no big deal.
The Silent Killer: NSAIDs and Other Nephrotoxins
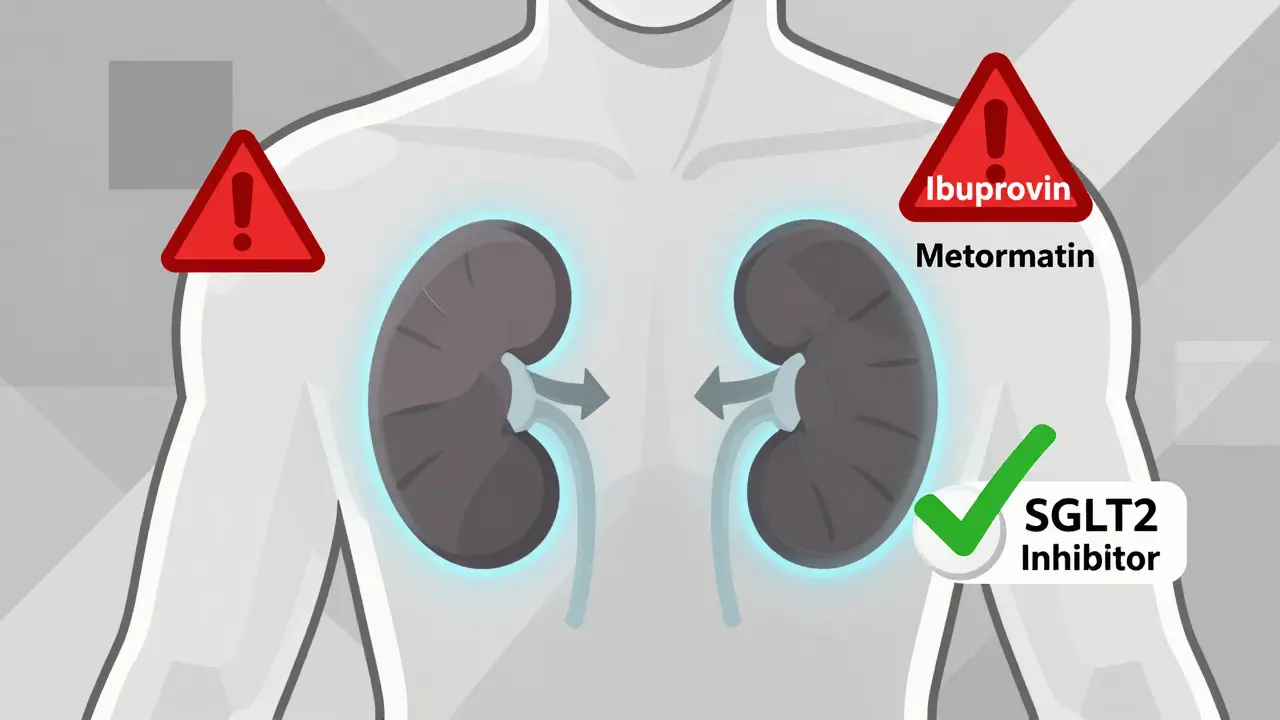
One of the most common mistakes? Taking ibuprofen or naproxen for a headache. These NSAIDs - nonsteroidal anti-inflammatory drugs - are the number one cause of acute kidney injury in people with CKD. They cut off blood flow to the kidneys. In someone with stage 3 or 4 kidney disease, two Advil can spike creatinine from 3.2 to 5.7 in under 48 hours. That’s not a fluke. It’s a pattern.
One user on the American Association of Kidney Patients forum, ‘DialysisDave,’ shared his story: after taking ibuprofen for a headache, he ended up in the ER with acute kidney injury. His creatinine jumped so fast, he nearly died. He wasn’t alone. A 2023 NIDDK survey found that 68% of CKD patients had no idea NSAIDs were risky. Even worse - many pharmacists don’t ask.
But NSAIDs aren’t the only danger. Some antibiotics, like gentamicin, can wreck kidney cells. Vancomycin? Needs careful monitoring. Contrast dye used in CT scans? A major red flag. Even some laxatives and herbal supplements - like senna or aristolochic acid - can cause permanent damage.
Dosing by eGFR: The New Rulebook
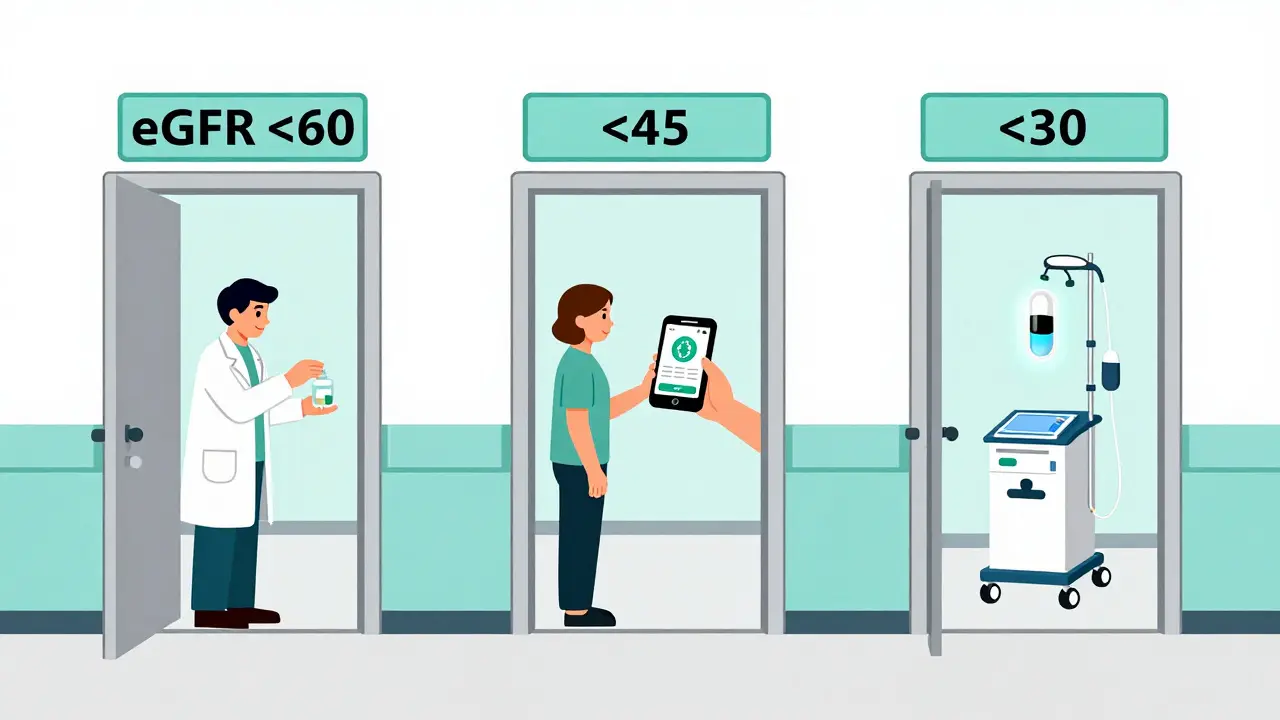
The standard now? Use eGFR - estimated glomerular filtration rate - not just creatinine. eGFR tells you how well your kidneys are filtering. It’s calculated from age, sex, race, and serum creatinine. The KDIGO 2024 guidelines (the gold standard) say:
- eGFR < 60 mL/min/1.73 m²: Start reviewing all medications
- eGFR < 45 mL/min/1.73 m²: Many drugs need dose reduction
- eGFR < 30 mL/min/1.73 m²: High-risk zone. Avoid certain drugs entirely
- eGFR < 15 mL/min/1.73 m²: Dialysis or transplant needed. Dosing becomes highly individualized
For example:
- Metformin (for diabetes): Must be stopped if eGFR drops below 30. Between 30 and 45, use the lowest dose and check kidney function monthly. Why? It can cause lactic acidosis - a rare but deadly buildup of acid in the blood.
- Vancomycin: In healthy people, the target blood level is 15-20 mcg/mL. In CKD, it drops to 10-15 mcg/mL. Too high? Hearing loss. Too low? Infection doesn’t clear.
- Aminoglycosides (like gentamicin): Normally given every 8 hours. In CKD, switch to once-daily dosing. This reduces toxicity while keeping effectiveness.
The Game-Changer: SGLT2 Inhibitors
Here’s the twist: not all drugs get harder to dose as kidneys fail. SGLT2 inhibitors - like dapagliflozin and empagliflozin - are the exception. They work differently. Instead of being cleared by the kidneys, they’re broken down in the liver. So no matter how bad your kidney function gets, the dose stays the same: 10 mg once daily.
And they’re not just safe - they’re protective. The CREDENCE trial showed SGLT2 inhibitors cut the risk of kidney failure, dialysis, or death from kidney disease by 39%. That’s why KDIGO 2024 now recommends them for nearly all CKD patients, even those without diabetes. They don’t just treat symptoms. They slow the disease.
What About Blood Pressure Drugs?
For years, doctors held back on ACE inhibitors and ARBs - drugs like lisinopril or losartan - because they raise creatinine. That scared people. But here’s the truth: a rise in creatinine from an ACE inhibitor doesn’t mean kidney damage. It means the drug is working. It’s reducing pressure inside the kidney’s filtering units, which protects them long-term.
KDIGO 2024 says: use the highest tolerated dose. Full stop. Don’t hold back because creatinine went up 0.3 or 0.5. That’s not a warning - it’s a sign you’re doing right. Experts like Dr. Katherine Tuttle say skipping this step is “suboptimal care.”
And if you’re still leaking protein (albuminuria) despite maximum ACE/ARB therapy? Add finerenone. It’s new, it’s powerful, and it cuts kidney failure risk by 23% in high-risk patients.
How to Stay Safe: Practical Steps
Real people survive with CKD. Not by luck - by systems. Here’s what works:
- Use one pharmacy. The NIDDK found a 42% drop in medication-related kidney injuries when patients used a single pharmacy. Pharmacists can track interactions, flag nephrotoxins, and call your doctor if something’s off.
- Review meds every 3 months. KDIGO recommends a full medication review for anyone with stage 3-5 CKD. Bring a list - all prescriptions, OTCs, supplements. Ask: “Is this still safe for my kidneys?”
- Know your eGFR. Don’t just look at creatinine. Ask for your eGFR number. If it’s below 60, every medication needs a second look.
- Use apps. Tools like Epocrates Renal Dosing are used by 63% of U.S. nephrologists. They give instant dosing advice based on your eGFR.
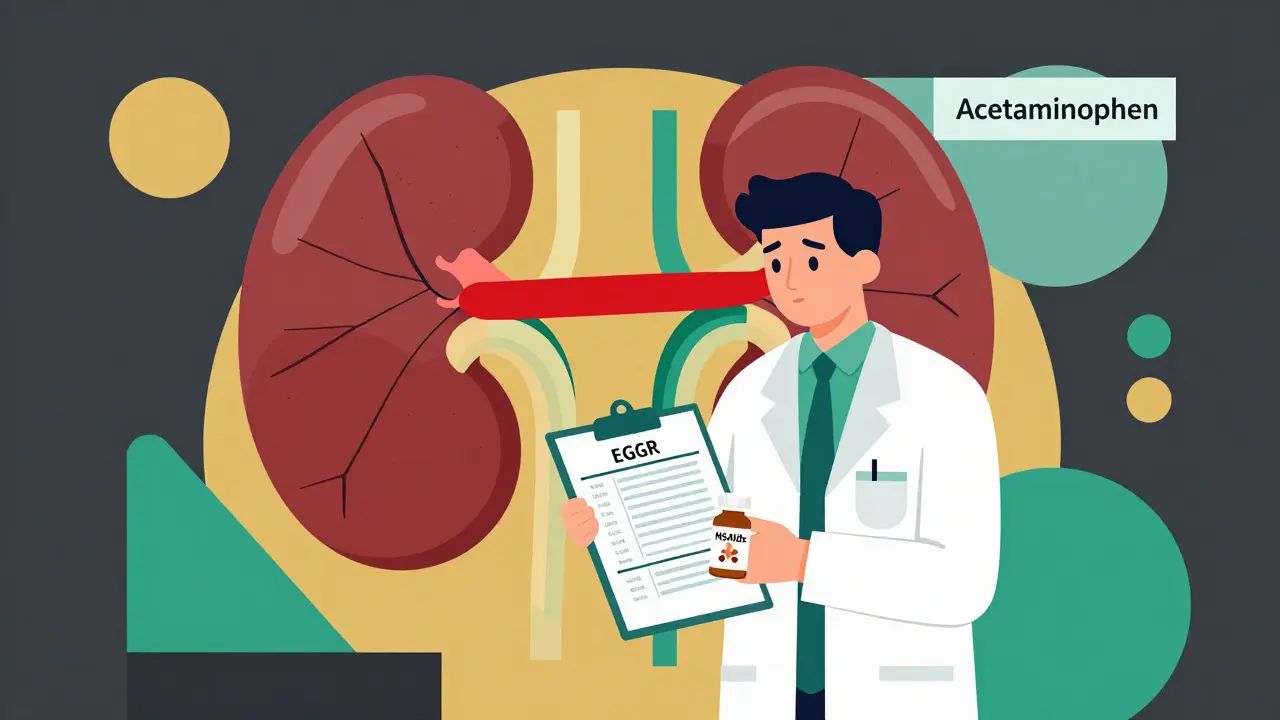
- Never take NSAIDs without asking. If you need pain relief, try acetaminophen (Tylenol) - it’s safer for kidneys. But don’t overdo it - liver damage is a risk too.
The Big Gaps
Even with the best guidelines, holes remain. Most dosing rules are based on stable CKD. But what if you get sick? A bad infection, dehydration, or surgery can crash your eGFR overnight. Hospitals rarely have protocols to adjust doses during acute kidney injury. One study found 41% of acute care units don’t have rules for this.
And what about end-stage kidney disease? If you’re not on dialysis yet, dosing becomes guesswork. The FDA says this is the “worst-case scenario” for drug studies - but very few drugs have clear guidance here.
That’s why therapeutic drug monitoring matters. For drugs like vancomycin or digoxin, checking blood levels isn’t optional - it’s life-saving.
What’s Coming Next
The future is better. In 2026, the FDA plans to update its guidelines using real-world data from electronic health records. KDIGO is working on a standardized checklist for CKD patients - to be released mid-2026. And pharmacies are starting to integrate eGFR alerts into their systems.
Meanwhile, researchers are exploring pharmacogenomics - using your genes to predict how you’ll react to drugs. Early trials are looking at how kidney disease changes how your body processes common meds. This could one day mean a blood test tells you exactly which drugs to avoid.
For now, the best defense is simple: know your numbers. Ask questions. Use one pharmacy. And never take a new pill - even an OTC one - without checking if it’s safe for your kidneys.
Can I still take ibuprofen if I have kidney disease?
No - not safely. Ibuprofen and other NSAIDs reduce blood flow to the kidneys, which can cause sudden kidney injury, especially if your eGFR is below 60. Even a single dose can spike creatinine levels. Use acetaminophen (Tylenol) instead for pain, and always check with your doctor before taking any painkiller.
What if my eGFR drops suddenly while I’m on medication?
Act fast. If your eGFR drops more than 25% in a week - say, from 50 to 35 - call your doctor immediately. Many drugs need dose changes during acute illness, dehydration, or infection. Don’t wait for your next scheduled visit. Hospitals often don’t have protocols for this, so you need to speak up.
Is metformin always dangerous for kidney disease?
Not always. Metformin is safe if your eGFR is above 45. Between 30 and 45, you can take it - but only at the lowest dose and with monthly kidney checks. Below 30, it’s stopped. The fear of lactic acidosis is real, but many people with CKD stay on metformin safely with proper monitoring.
Do SGLT2 inhibitors work if I don’t have diabetes?
Yes. SGLT2 inhibitors like dapagliflozin are now recommended for all CKD patients with albuminuria, even without diabetes. They reduce kidney damage and lower the risk of heart failure and death. This is a major shift in kidney care - and it’s backed by strong clinical trials.
How often should I get my kidney function checked?
At least every 3 months if you have stage 3-5 CKD. If you’re on high-risk medications, have diabetes, or have recently been sick, check every 4-6 weeks. Your eGFR and potassium levels are your early warning system.





Michael Page
February 14, 2026 AT 19:34It’s not just about dosing. It’s about the system failing people before they even get to the pharmacy. Doctors don’t get trained in renal pharmacology. Pharmacies don’t have real-time eGFR integration. Patients are left to Google their meds and hope they don’t die. This isn’t medical care-it’s a liability lottery. And the worst part? The people who need this info most are the least likely to understand it.
Joe Grushkin
February 14, 2026 AT 23:22Let’s be real-SGLT2 inhibitors aren’t magic. They’re expensive, and most patients can’t afford them. The guidelines sound great on paper but ignore the fact that 40% of CKD patients in this country are on Medicaid or have no insurance. You want to save kidneys? Fix the system first. Then talk about dosing.
Virginia Kimball
February 15, 2026 AT 11:31I love how this post breaks it all down-it’s like someone finally translated the medical jargon into something human. I used to think Tylenol was the only safe painkiller, but now I know to ask about my eGFR before even touching an OTC pill. My mom’s on metformin and we just had her med review last week. Small steps, but they matter. Keep sharing this stuff.
Daniel Dover
February 17, 2026 AT 02:09One pharmacy. That’s the easiest win. Done.
Chiruvella Pardha Krishna
February 18, 2026 AT 23:33There is a deeper truth here: medicine treats disease as if it were a static condition. But the body is a river. When infection strikes, when dehydration hits, when sleep vanishes-these are not abstract variables. They are tidal waves that drown the carefully calculated dose. We have checklists, but no contingency. We are preparing for calm seas while sailing into a hurricane.
Kaye Alcaraz
February 19, 2026 AT 06:46For anyone reading this: if you have CKD, get your eGFR number. Write it down. Put it on your fridge. Show it to your pharmacist. If they don’t know what it means, find a new one. This isn’t optional. Your kidneys don’t get second chances.
Sarah Barrett
February 20, 2026 AT 10:01The real tragedy isn’t the lack of guidelines-it’s the lack of urgency. We have the tools. We have the data. We have the trials. But no one is screaming. No one is lobbying. No one is forcing EHRs to flag nephrotoxins. And so, the silence continues. People die in silence.
Erica Banatao Darilag
February 20, 2026 AT 22:11i just had my first kidney check this year and my eGFR was 48… i didn’t even know what that meant. i’ve been taking ibuprofen for my back for 3 years. i’m so scared. thank you for this. i’m calling my doctor tomorrow.