Medication Overuse Headache Risk Checker
Check if your headache medication use puts you at risk for medication overuse headache (MOH) based on evidence-based guidelines from the article.
Think your headache is just getting worse over time? You might not be getting sicker-you could be using the wrong medicine to fix it. Every year, thousands of people in the U.S. and Europe unknowingly turn their occasional headaches into daily pain by doing exactly what their doctors told them: take painkillers when it hurts. This isn’t a rare oddity. It’s called medication overuse headache (MOH), and it’s one of the most common reasons people end up with chronic headaches they can’t shake.
What Exactly Is a Drug-Related Headache?
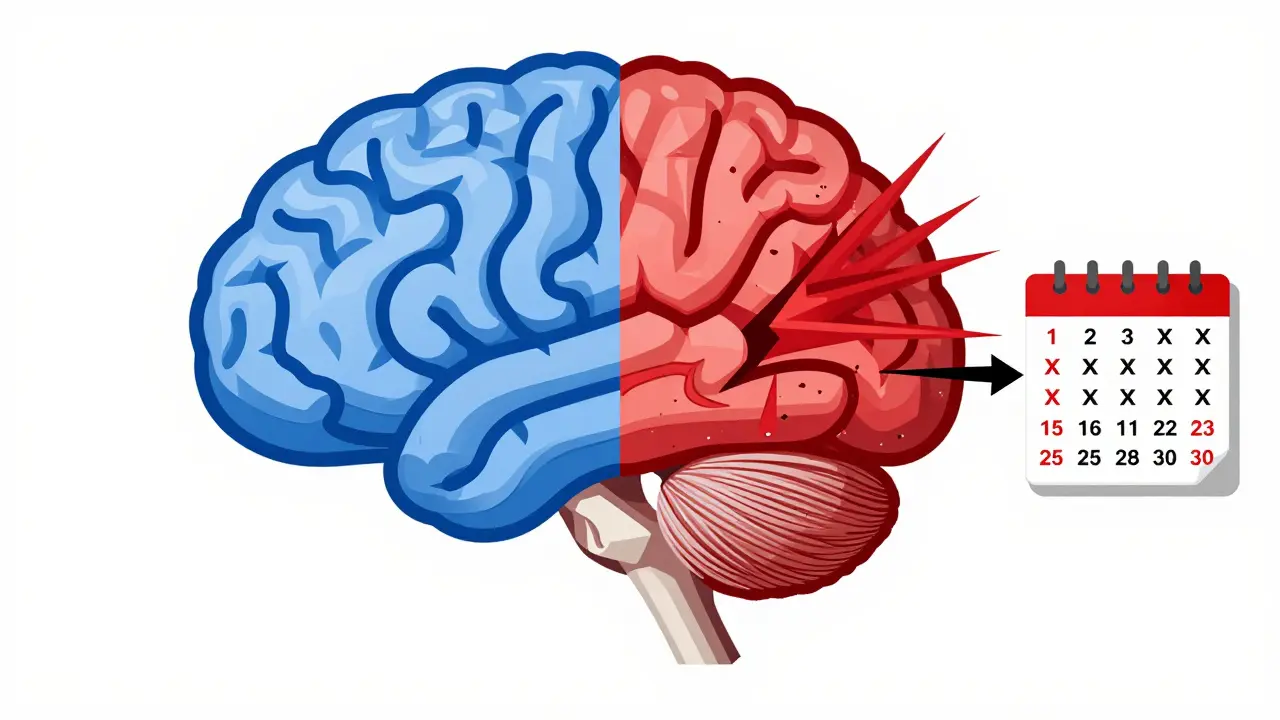
Medication overuse headache isn’t a new kind of headache. It’s the same old migraine or tension headache you already had-except now it’s happening 15 or more days a month because you’ve been treating it too much. The irony? The drugs meant to stop your pain are the ones making it worse. This isn’t about addiction in the street-drug sense. It’s about your brain getting rewired by repeated exposure to painkillers.
The science is clear: when you take headache meds too often, your brain stops normalizing pain signals. Studies using brain scans show these patients have heightened sensitivity to touch, light, and sound-not because their headache got worse, but because their nervous system stopped learning to ignore it. This isn’t in your head. It’s in your neurons.
Which Medications Cause This?
Not all pain relievers are equal when it comes to triggering MOH. Some are far more dangerous than others. Here’s what the data shows:
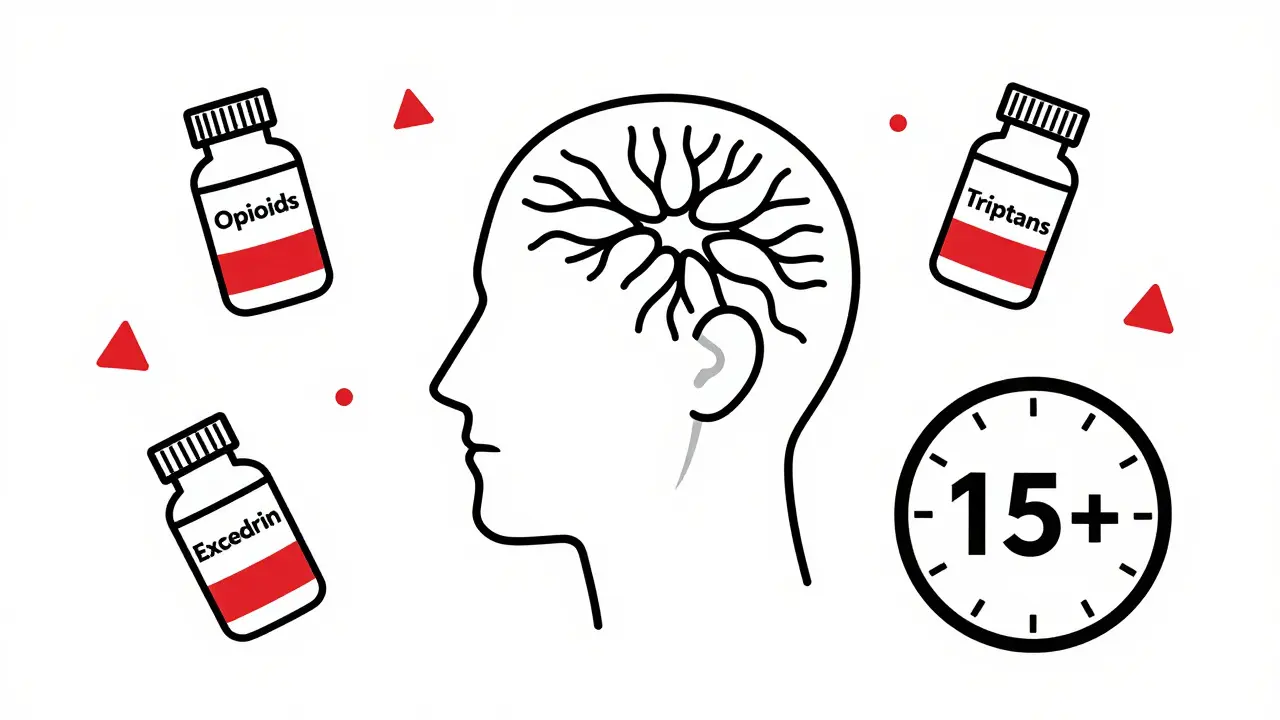
- Opioids (like oxycodone, hydrocodone, tramadol): Just 10 days a month of use can trigger MOH. These are the worst offenders.
- Butalbital combinations (like Butapap or Lanorinal): Also high-risk. Only 10 days a month is enough to set off the cycle.
- Triptans (Imitrex, Zomig): Used for migraines. Over 10 days a month? You’re at risk.
- Combination analgesics (Excedrin, which has aspirin, acetaminophen, and caffeine): Over 15 days a month can cause problems.
- NSAIDs (ibuprofen, naproxen): Lower risk, but still dangerous if you hit 15+ days a month. The FDA says you shouldn’t exceed 1,200mg of ibuprofen or 660mg of naproxen in a single day.
Here’s the catch: most people don’t realize they’re overusing. They think, “I only took two pills yesterday and three today.” But if you’re doing that every day for three months straight, your brain is in damage mode.
How Do You Know If It’s MOH?
The diagnosis is simple-if you have these three things, you likely have medication overuse headache:
- Your headaches happen 15 or more days a month.
- You’ve been doing this for more than 3 months.
- You’re regularly using one of the high-risk medications listed above.
It’s not about how bad the pain is. It’s about how often it shows up. Many patients think, “I’m not sick-I just have a constant dull ache.” That’s exactly the warning sign. If your headache has become your new normal, it’s probably not normal at all.
Doctors often miss this. Patients come in saying, “I’ve had headaches for years,” and the doctor just prescribes more pills. That’s why keeping a headache diary matters. Write down: when the pain started, how long it lasted, what you took, and whether it helped. Even a few weeks of tracking can reveal the pattern.
What Happens When You Stop the Meds?
Stopping the drug is the only way to fix this-but it’s not easy. Withdrawal symptoms are real and intense. In a 2022 study of 350 patients, 92% had worse headaches during withdrawal. Nearly 7 out of 10 felt nauseous. Over 4 in 10 vomited. One in three had low blood pressure.
It’s not a myth. It’s science. Your brain has gotten used to the drug. When you remove it, your nervous system goes haywire. This is why tapering matters. For opioids and butalbital, stopping cold turkey can be dangerous. You need to reduce slowly under medical supervision. For triptans and NSAIDs, many people can stop abruptly-but they need backup.
That’s where rescue meds come in. If you’re quitting Excedrin, you can use a single dose of a non-overused painkiller like acetaminophen-but only twice a week. No more. Otherwise, you’re just swapping one problem for another.
How Do You Get Better?
Stopping the meds is step one. Step two is preventing the headaches from coming back. You can’t just quit and hope for the best. You need a plan.
Doctors now recommend three proven preventive treatments:
- Topiramate (40-100mg daily): An antiseizure drug that also blocks migraine pathways.
- Propranolol (80-160mg daily): A beta-blocker that reduces blood vessel spasms linked to migraines.
- CGRP inhibitors (Aimovig, Emgality, Ajovy): Monthly injections that block a brain chemical tied to migraine pain. These work for 50-60% of patients.
And here’s the game-changer: newer drugs called gepants (Ubrelvy, Nurtec, Zavzpret) are now being used for acute attacks-and they don’t cause MOH. That’s huge. Unlike triptans or opioids, these don’t trigger brain sensitization. If you’ve had MOH before, they might be your safest option going forward.
Also, in January 2024, the FDA approved atogepant (Qulipta) for preventing migraines in people with MOH. This is the first drug specifically cleared for this group. It’s not a cure, but it’s a step forward.
Why Do So Many People Miss This?
Because doctors don’t always ask the right questions. Patients don’t realize their daily Excedrin is the problem. Reddit threads from the r/Migraine community show a pattern: 68% of people said they didn’t believe their doctor when they were told their meds were causing the headaches. One user wrote: “I thought my doctor was blaming me.”
Another common mistake: stopping the meds but not starting prevention. Studies show 78% of patients relapse within three months if they don’t begin a preventive treatment right away. It’s not enough to quit the painkillers. You need to protect your brain from the next wave.
What Should You Do Right Now?
If you’re taking headache meds more than 10 days a month, here’s your action plan:
- Track your headaches and meds for two weeks. Use a simple notebook or phone app.
- Find out what you’re taking and how often. Check the label-some combo pills have caffeine or butalbital you might not realize you’re using.
- Don’t stop cold turkey if you’re on opioids or butalbital. Talk to your doctor about a taper plan.
- Ask about preventive options. Topiramate, propranolol, or CGRP inhibitors may be better long-term than daily pills.
- Consider switching to gepants (Ubrelvy, Nurtec) for acute attacks. They’re pricier, but they don’t cause MOH.
And if you’re feeling overwhelmed? You’re not alone. Thousands of people have walked this path. One user on Reddit said: “After five weeks off Excedrin, my headache days dropped from 28 to 9 per month.” That’s not luck. That’s science.
What’s Next for MOH Treatment?
The future is getting smarter. Researchers have found 12 genetic markers linked to MOH risk. In the next few years, a simple blood test could tell you if you’re genetically prone to this problem-before you even start taking painkillers.
Also, companies are working on “smart” pain meds with built-in limits. Imagine a pill that stops working after 10 doses a month. Dr. Richard Lipton predicts these could cut MOH cases by 40-50% in the next decade.
For now, the best tool you have is awareness. If your headache isn’t getting better with more medicine, it might be getting worse. Stop. Track. Talk. Then act.



Stephon Devereux
February 12, 2026 AT 01:51Let me tell you something real: your brain isn't broken. It's adapting. Every time you pop a pill, your nervous system learns to expect it. No pill? Panic mode. That's not addiction-it's neuroplasticity gone sideways. The science here is rock solid. You're not weak. You're wired. And the fix? Not more drugs. Less. And patience. It takes months. But your brain can relearn how to be quiet again. I've seen it. People come back from this. Not because they're strong. Because their neurons are stubborn as hell and they want to feel normal.
Pat Mun
February 12, 2026 AT 20:11I was on Excedrin for 11 years. 15+ days a month. Thought I was just managing stress. Then my neurologist looked at me like I'd just confessed to stealing his lunch. Said I had MOH. I laughed. Said he was crazy. Then I tracked it. 27 headache days in one month. 24 of them with Excedrin. I quit cold turkey. Day 3: I cried for 12 hours. Day 7: I couldn't stand the light. Day 14: I thought I was dying. Day 30: I could hear birds outside. Not because they got louder. Because my brain finally stopped screaming. I'm on topiramate now. Still not perfect. But 4 days a month? That's a win. If you're reading this and you're still popping pills like candy? Stop. Track. Breathe. Your brain isn't broken. It's just tired.
Rachidi Toupé GAGNON
February 13, 2026 AT 07:27Just stopped my triptans after 8 years. 20 days a month. Felt like my skull was being crushed by a hydraulic press. Withdrawal? Oh yeah. Nausea, zaps, panic attacks, sleepless nights. But after 6 weeks? My headaches went from daily to maybe 3x a month. And I didn’t even need the fancy CGRP shots. Just sleep, hydration, and yoga. No magic pill. Just consistency. You got this. 💪
Alyssa Williams
February 14, 2026 AT 00:08Autumn Frankart
February 15, 2026 AT 08:09They don’t want you to know this but the FDA and Big Pharma are in bed together. MOH? It’s a scam. They make billions off people like you-hooked on pills they *know* cause the problem. Why? Because if you stop, you need a new drug. So they sell you more. They don’t care if you’re in pain. They care about your insurance claims. Read the fine print. Caffeine? Butalbital? Hidden in your "over-the-counter" meds. That’s not medicine. That’s chemical manipulation. And the doctors? They’re paid to look away. I’ve got the documents. I’m filing a class action. You’re not alone. Wake up.
Neha Motiwala
February 15, 2026 AT 15:34They told me to stop my triptans. I did. Then I got worse. Like, screaming-in-the-shower worse. My husband left. My boss said I was "unreliable." My cat stopped cuddling. I thought I was dying. Then I found a Reddit thread. Someone said: "It’s not you. It’s your brain rewiring." I cried. I still cry. But now I take topiramate. And I drink water. And I don’t take pills unless I’m on the floor. I’m not cured. But I’m not a zombie anymore. If you’re reading this? You’re not broken. You’re being reset. And that hurts. But it’s worth it.
Skilken Awe
February 16, 2026 AT 02:30Let’s be real. You think this is about "neuroplasticity"? Nah. It’s about profit margins. The pharmaceutical industry needs you to believe you’re addicted to painkillers so they can sell you a $1,200/month injection that "blocks CGRP." Meanwhile, the real solution-sleep, hydration, stress management-is free. But you can’t patent a nap. So they rebrand it as "lifestyle management" and call it "complementary therapy." Meanwhile, your insurance won’t cover it. They don’t want you healed. They want you on a subscription. I’ve worked in pharma sales. I know how this works. Stop paying for their lies.
Steve DESTIVELLE
February 16, 2026 AT 11:19What is pain if not the body’s way of saying stop? We have forgotten this. We have turned pain into a problem to be solved with chemicals rather than a signal to be understood. The modern medical paradigm reduces the human experience to neurotransmitters and receptors. But the soul does not speak in milligrams. It speaks in silence. In stillness. In the space between breaths. To heal from MOH is not to stop taking drugs. It is to stop running from yourself. The pills were never the enemy. The fear was. You are not broken. You are becoming. The headache is not your enemy. It is your teacher.
athmaja biju
February 17, 2026 AT 00:24India has the highest rate of medication overuse in Asia. Why? Because pharmacies sell painkillers like candy. No prescription. No questions. I saw a man buy 50 tablets of Combiflam in one go. The pharmacist smiled. I asked why. He said, "People need relief." Relief? Or dependency? We don’t teach people how to live with pain. We teach them how to drown it. And then we wonder why chronic pain is rising. This isn’t a medical issue. It’s a cultural one. We’ve outsourced discomfort. And now we’re paying the price.
Ernie Simsek
February 18, 2026 AT 19:16bro i quit excedrin after 10 years and the first week was like my brain was on fire 🔥🔥🔥 i thought i was gonna die but then i started doing 10 mins of breathing before bed and now i only get headaches like 2x a month and i don’t even care anymore. also i got a dog. dogs are the real gepants. 🐶❤️
Kristin Jarecki
February 19, 2026 AT 06:33As a neurologist with over 20 years of clinical experience, I must emphasize that medication overuse headache is not merely a pharmacological phenomenon-it is a complex interplay of neurobiological, psychological, and sociocultural factors. The data presented in the original post is accurate, but the framing risks oversimplifying a condition that often coexists with anxiety, depression, and sleep dysregulation. A successful recovery requires multidisciplinary care: behavioral therapy, pharmacological prevention, and structured tapering under supervision. I urge patients not to attempt abrupt cessation without professional guidance, particularly with opioids or barbiturates. The path to relief is not linear, but it is absolutely achievable with the right support system.
andres az
February 20, 2026 AT 09:25MOH? More like "Money Over Health." They don’t want you cured. They want you hooked. Look at the timeline: triptans introduced in 1993. MOH cases skyrocketed by 2005. Coincidence? Or corporate strategy? I’ve dug into the FDA’s advisory committee minutes. They knew. They just didn’t act. And now they’re pushing gepants at $10K a year. Same game. New label. Same profit. Don’t believe the hype. Don’t trust the doctor who only prescribes. Find a functional neurologist. Or go off-grid. Your brain doesn’t need a patent. It needs rest.
alex clo
February 21, 2026 AT 05:50I appreciate the thorough breakdown. I’ve been managing migraines for 15 years and only recently learned about MOH. My doctor never mentioned it. I’m starting topiramate next week and tracking everything. Thank you for the clarity. This is exactly the kind of information that should be on every prescription label.