Fluoroquinolone Delirium Risk Assessment
Assess Your Risk of Antibiotic-Induced Delirium
This tool helps identify if you or a loved one is at higher risk for delirium when taking fluoroquinolone antibiotics like levofloxacin or ciprofloxacin.
Risk Assessment Results
When an older adult starts taking an antibiotic like levofloxacin or ciprofloxacin, most people assume it’s just another pill to fight an infection. But for some, especially those over 65, that pill can trigger something far more dangerous: sudden confusion, hallucinations, and memory loss. This isn’t rare. It’s not just a side effect-it’s a recognized medical emergency called fluoroquinolone-induced delirium.
What Are Fluoroquinolones?
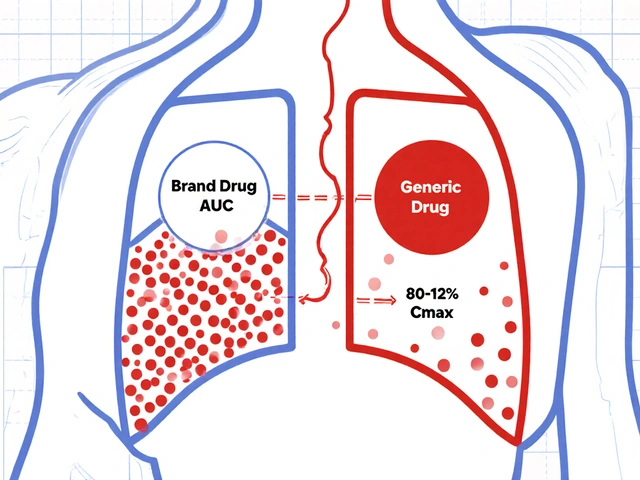
Fluoroquinolones are a class of powerful antibiotics used for serious infections like pneumonia, complicated urinary tract infections, and some types of skin infections. Common names include ciprofloxacin, levofloxacin, and moxifloxacin. They work by stopping bacteria from copying their DNA, which kills them off fast. That’s why doctors reach for them when other antibiotics fail.
But here’s the problem: these drugs don’t just target bacteria. They also cross the blood-brain barrier easily. In fact, levofloxacin reaches up to 90% of its blood concentration in the cerebrospinal fluid. That’s higher than most other antibiotics. And in older adults, whose brains are more sensitive, that’s a recipe for trouble.
How Fluoroquinolones Trigger Delirium
Delirium isn’t dementia. It’s sudden, confusing, and often reversible. Symptoms include:
- Not knowing where you are or what day it is
- Seeing or hearing things that aren’t there
- Being unusually agitated or withdrawn
- Struggling to follow a conversation or remember simple things
These symptoms usually show up within 1 to 3 days after starting the antibiotic. In one documented case, a 72-year-old woman on levofloxacin for a urinary infection became confused, hallucinated voices, and couldn’t recognize her own daughter. Within 48 hours of stopping the drug, she was back to normal.
The science behind this is clear: fluoroquinolones block GABA-A receptors in the brain. GABA is the brain’s main calming signal. When it’s shut down, neurons fire out of control. This imbalance leads to excitotoxicity-essentially, the brain overstimulates itself. Some studies also suggest these drugs directly activate NMDA receptors, which are linked to memory and learning. In older brains, already weakened by age or illness, this can push the system over the edge.
Who’s at Highest Risk?
Not everyone gets delirium from fluoroquinolones. But certain people are far more vulnerable:
- Age 65+: Nearly half of all hospitalized older adults are over 65, and they’re 3 times more likely to develop this side effect.
- Kidney problems: About 85% of levofloxacin is cleared by the kidneys. If kidneys are weak, the drug builds up in the blood and brain.
- Existing brain issues: People with dementia, Parkinson’s, or past strokes are at higher risk.
- High doses: Taking 750 mg daily of levofloxacin (instead of 500 mg) doubles the chance of neurological side effects.
- Diabetes or low blood sugar: The FDA warns fluoroquinolones can cause dangerous drops in blood sugar, especially in older adults, which can mimic or worsen delirium.
One study found that 40% of hospitalized older adults with delirium had been on a fluoroquinolone. And in many cases, doctors didn’t connect the dots until it was too late.

Why Doctors Miss It
Delirium is often mistaken for dementia, depression, or just "getting old." A 2016 review of 391 cases found fluoroquinolones were responsible for 18% of antibiotic-related delirium cases-more than any other class. Yet, as Dr. Shamik Bhattacharyya from Harvard pointed out, "Antibiotics are not necessarily the first medications doctors may suspect."
On Reddit, a physician with 10 years of experience said he’d seen three cases where fluoroquinolones caused severe delirium. Each time, it took 24 to 48 hours to realize the antibiotic was the cause. By then, the patient was already in a longer hospital stay, at risk of falls, and possibly heading to a nursing home instead of going home.
The American Academy of Neurology says this is a major blind spot in geriatric care. Delirium increases the risk of death by up to 40%. It also doubles the chance of long-term cognitive decline.
What Happens When You Stop the Drug?
Good news: if caught early, the damage is usually reversible.
In case reports, symptoms disappeared within 48 to 96 hours after stopping the fluoroquinolone. One patient in a 2018 study had full cognitive recovery in just 48 hours. No brain scans, no drugs-just stopping the antibiotic.
But here’s the catch: you have to recognize it first. Doctors need to rule out other causes: low sodium, infection in the brain, thyroid problems, or alcohol withdrawal. A normal CT scan and EEG don’t rule out fluoroquinolone delirium-they just help eliminate other possibilities.
Alternatives That Are Safer
You don’t need fluoroquinolones for most infections. For a simple UTI, nitrofurantoin or trimethoprim-sulfamethoxazole work just as well-and don’t touch the brain. For pneumonia, amoxicillin or doxycycline are often better first choices.
Even among antibiotics, some are safer than others. Beta-lactams like penicillin or ceftriaxone rarely cause delirium because they don’t cross into the brain easily. Cefepime is an exception-it can cause neurotoxicity, but through different mechanisms and much less often than fluoroquinolones.
The American Geriatrics Society’s 2023 Beers Criteria lists fluoroquinolones as "potentially inappropriate" for older adults. That’s their highest warning level. It means: avoid them unless there’s absolutely no other option.
What’s Changing in Practice?
After the FDA’s 2018 safety warning, prescriptions for fluoroquinolones in older adults dropped by over 20%. Hospitals like UCSF cut levofloxacin use for UTIs in seniors by 35% after putting in new protocols.
Now, many hospitals require:
- Checking kidney function before prescribing
- Using the lowest effective dose
- Monitoring patients for confusion during the first 72 hours
- Documenting why no safer alternative was used
Even with these steps, fluoroquinolones are still prescribed too often. In 2019, over 26 million prescriptions were filled in the U.S. alone. That’s 7.8% of all outpatient antibiotics. Many are for minor infections-sinusitis, bronchitis-that don’t need such strong drugs.
What Should You Do?
If you or a loved one over 65 is prescribed a fluoroquinolone:
- Ask: "Is there a safer antibiotic for this infection?"
- Ask: "What are the signs of confusion I should watch for?"
- Ask: "Can we start with a lower dose?"
Watch closely for any sudden changes in behavior in the first 3 days. If the person becomes disoriented, agitated, or starts seeing things that aren’t there-call the doctor immediately. Don’t wait. Stop the drug only if instructed, but get help fast.
And if you’re a caregiver: keep a daily log of mood, sleep, and awareness. That record can help doctors spot a pattern before it becomes a crisis.
The Bigger Picture
Fluoroquinolones aren’t going away. They’re still vital for life-threatening infections like anthrax or drug-resistant TB. But for most common infections in older adults, they’re overused-and dangerous.
The future is moving toward smarter prescribing: clinical decision tools that flag high-risk patients before the prescription is written. Research is also looking for blood markers that could predict who’s likely to have a reaction. But for now, the safest strategy is simple: avoid them unless absolutely necessary.
Older adults deserve antibiotics that treat infection without stealing their mind. The science is clear. The warnings are loud. The choice? It’s yours to make.
Can fluoroquinolones cause permanent brain damage in older adults?
In nearly all documented cases, cognitive symptoms from fluoroquinolone-induced delirium fully reverse after stopping the drug. There’s no strong evidence of permanent brain damage from a single episode. However, delirium itself can accelerate long-term cognitive decline, especially in people with early dementia. The longer delirium lasts, the higher the risk of lasting problems. That’s why early recognition and stopping the antibiotic is critical.
Is levofloxacin more dangerous than ciprofloxacin for seniors?
Both levofloxacin and ciprofloxacin carry similar risks for delirium in older adults. Levofloxacin has slightly higher brain penetration and is more commonly linked to cases in published reports, likely because it’s prescribed more often. Ciprofloxacin is still a major culprit. Neither is safer-the key is avoiding both when possible. Dose matters too: 750 mg daily increases risk more than 500 mg.
How long does fluoroquinolone delirium last?
Symptoms usually begin 1 to 3 days after starting the drug and resolve within 48 to 96 hours after stopping it. Most patients return to their baseline cognitive state within a week. In rare cases, if the delirium was severe or prolonged, it may take longer-up to 2 weeks-for full recovery. But permanent deficits are uncommon if the drug is stopped promptly.
Can fluoroquinolones cause hallucinations in elderly patients?
Yes. Hallucinations-both visual and auditory-are a well-documented symptom of fluoroquinolone-induced delirium. Patients report seeing people who aren’t there, hearing voices, or feeling insects crawling on their skin. These are not signs of psychosis or dementia alone; they’re direct neurological effects of the drug blocking brain signals. These symptoms are a red flag and require immediate discontinuation of the antibiotic.
Are there any blood tests to detect fluoroquinolone neurotoxicity?
No standard blood test exists yet to predict or confirm fluoroquinolone-induced delirium. Diagnosis is clinical: based on symptoms, timing, and ruling out other causes like infection, low sodium, or metabolic issues. Researchers are studying biomarkers, like specific brain proteins or genetic markers, but nothing is ready for clinical use. For now, the best tool is awareness and close monitoring.
Should older adults avoid all antibiotics?
No. Antibiotics save lives. The issue is which ones are chosen. Fluoroquinolones should be avoided in older adults when safer alternatives exist. For common infections like UTIs or bronchitis, antibiotics like nitrofurantoin, amoxicillin, or doxycycline are just as effective and much safer for the brain. The goal isn’t to avoid antibiotics-it’s to choose the right one for the right patient.






jefferson fernandes
January 12, 2026 AT 23:21Let me be clear: fluoroquinolones are not antibiotics-they’re neurological landmines wrapped in a prescription bottle. I’ve seen elderly patients go from sharp as a tack to completely lost in 36 hours after one dose. And yes, it’s reversible-if you catch it. But too many docs treat delirium like it’s just ‘old age’ and keep the script going. That’s malpractice disguised as convenience.
Acacia Hendrix
January 14, 2026 AT 10:42It’s fascinating how the pharmacokinetics of fluoroquinolones-particularly their high CSF penetration and GABA-A antagonism-create a perfect storm in the aging CNS. The NMDA receptor activation component is particularly underappreciated in clinical literature. Most clinicians still think in terms of ‘side effects’ rather than neurotoxic cascade dynamics. We need more neuropharmacology training in geriatric residencies.
James Castner
January 15, 2026 AT 16:44I’ve spent decades in emergency medicine, and let me tell you-there’s nothing more heartbreaking than watching a bright, independent 70-year-old woman stare at her own daughter like she’s a stranger, because some overworked intern reached for the easy antibiotic. We’ve got a culture of ‘quick fix’ medicine that ignores the long-term cost to human dignity. Fluoroquinolones aren’t just risky-they’re morally questionable when safer alternatives exist. This isn’t just medical advice-it’s a call to restore humility in prescribing.
Adam Rivera
January 16, 2026 AT 21:08My grandma got cipro for a UTI and thought she was seeing angels for three days. We thought she was having a spiritual moment. Turns out, she was having a drug reaction. I’m so glad someone’s talking about this. I told my uncle’s doctor last week to skip the fluoroquinolone-he’s 81, diabetic, and already forgets his keys. They switched him to amoxicillin. He’s fine now. Small wins matter.
Rosalee Vanness
January 17, 2026 AT 00:55It’s not just about the drug-it’s about the silence around it. Families don’t know to watch for sudden confusion. Nurses are stretched too thin to notice subtle shifts. Doctors are pressured to discharge fast. And when the patient’s mind goes blank, everyone shrugs and says, ‘Well, she’s just getting older.’ But no-this isn’t aging. This is iatrogenic trauma. I keep a little card in my wallet: ‘Watch for delirium after antibiotics.’ I hand it to every family I meet. One card. One conversation. Could save a mind.
lucy cooke
January 18, 2026 AT 21:56Oh, the tragedy of modern medicine-where we treat the body like a machine and forget the soul is wired into the same circuitry. Fluoroquinolones don’t just disrupt neurons-they disrupt identity. Imagine waking up and not knowing your own name because a doctor thought ‘faster is better.’ This isn’t healthcare. It’s pharmaceutical colonialism. We’ve outsourced wisdom to profit-driven guidelines. And the elderly? They’re the collateral damage in the war against ‘minor’ infections.
Trevor Davis
January 19, 2026 AT 20:28I’m a nurse. I’ve seen this too many times. One guy started cipro, got paranoid, tried to jump out the window thinking the walls were breathing. We had to sedate him. Family blamed dementia. Took us two days to realize it was the antibiotic. I swear, if I had a dollar for every time a doc said ‘it’s just old age’-I’d buy every senior in this country a new pair of socks and a warm hug. Stop being lazy. Check the meds first.
John Tran
January 21, 2026 AT 05:25so like... fluoroquinolones are bad for old peeps right? like, they get all weird and hallucinate? i mean, i get it, but like... isnt that just like... part of aging? i mean, my auntie used to talk to her dead husband and we just let her, you know? maybe its not the drug maybe its just... life? also i think the FDA is just scared of lawsuits, honestly. i mean, who even uses cipro anymore? i think its like 2% of prescriptions? idk just saying
mike swinchoski
January 22, 2026 AT 00:11Stop pretending this is a medical issue. It’s a moral failure. You think this is about science? It’s about profit. Big Pharma knows these drugs wreck brains-but they’re cheap, they’re fast, and insurance pays for them. Meanwhile, grandma’s walking around like a ghost because someone didn’t want to look up a different antibiotic. You don’t need a PhD to know that. You just need a heart.
Jesse Ibarra
January 22, 2026 AT 07:42And yet, you all still act like this is some shocking revelation. The FDA warned us in 2008. The Beers Criteria has listed these as inappropriate since 2012. We’ve had case reports since the 90s. This isn’t new. It’s negligence. You’re not raising awareness-you’re just now noticing the blood on your hands. Shame on every clinician who still prescribes this without a fight.
laura Drever
January 24, 2026 AT 01:31Yeah so what? We still use them. People die from untreated UTIs too. You want us to just let them pee themselves until sepsis? Realistic solutions? None. Just outrage. This is why medicine sucks.