Hydrocortisone is a synthetic glucocorticoid hormone that mimics the body’s natural cortisol. It reduces inflammation, suppresses immune responses, and helps manage adrenal insufficiency. Because it’s available in several forms-cream, ointment, tablet-it’s a go‑to drug for skin irritations, allergic reactions, and hormone replacement.
How Hydrocortisone Works in the Body
When you apply or ingest hydrocortisone, it binds to the glucocorticoid receptor, a protein found in nearly every cell. This binding triggers a chain reaction that shuts down inflammation‑producing genes and boosts anti‑inflammatory proteins. The result is less swelling, redness, and itching. The mechanism mirrors that of the adrenal gland’s own hormone, cortisol, which the body releases during stress.
Common Forms and Delivery Methods
Hydrocortisone comes in three main delivery formats, each suited for different conditions:
- Topical cream - 0.5% to 2.5% concentrations for eczema, insect bites, and minor rashes. Over‑the‑counter (OTC) versions are limited to 1% in many countries.
- Oral tablet - 10mg or 20mg pills used for adrenal insufficiency (Addison’s disease) or severe allergic reactions.
- Injectable suspension - Rare, reserved for acute asthma attacks or severe inflammatory flare‑ups.
Choosing the right form depends on the target area, severity, and whether a prescription is required.
Dosage Guidelines and Safety Tips
Dosage varies by age, condition, and formulation. Below is a quick reference:
- Adults (topical): Apply a thin layer 2-4 times daily for up to 7 days. Do not cover large body areas (>10% surface) with high‑potency creams.
- Children (topical): 0.5% cream, once or twice daily, limited to small patches. Watch for skin thinning.
- Adults (oral): 10-20mg in the morning, adjusted based on blood cortisol levels.
Always follow a healthcare professional’s advice. Overuse can lead to systemic absorption, especially with occlusive dressings.
Benefits and Typical Uses
Hydrocortisone shines in several everyday medical scenarios:
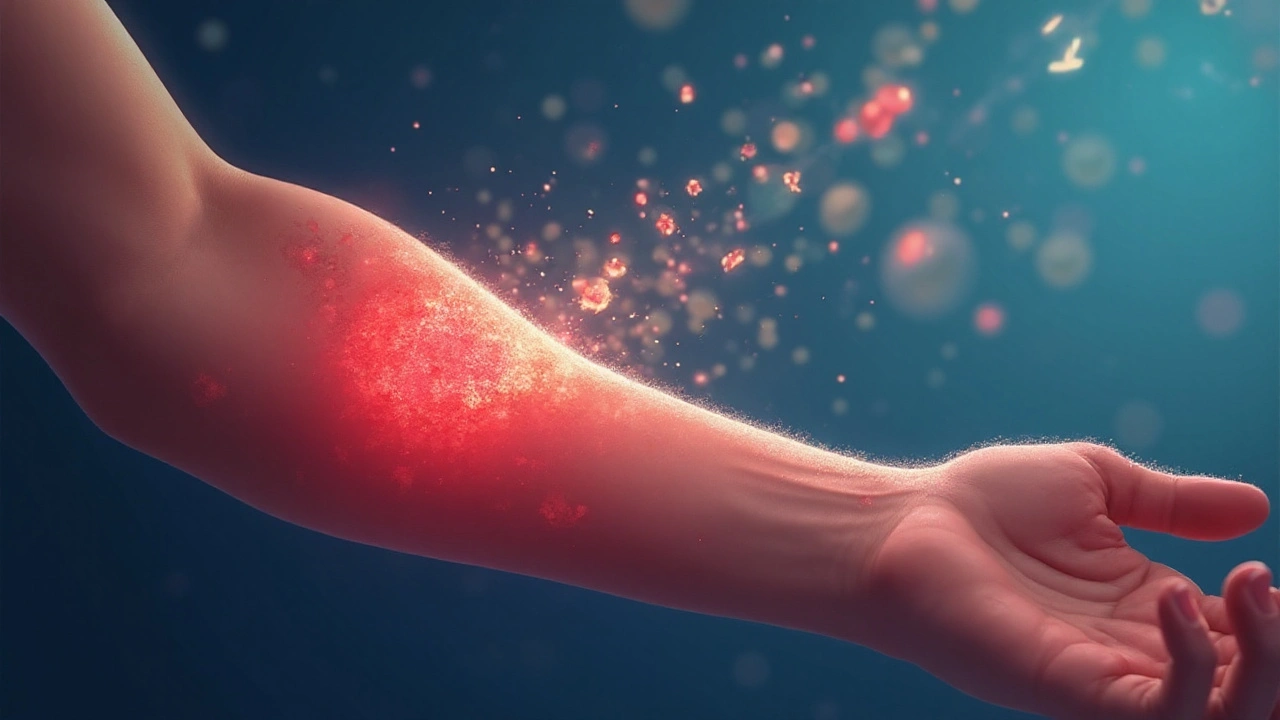
- Skin inflammation: Eczema, psoriasis flare‑ups, and contact dermatitis respond quickly to low‑strength creams.
- Allergic reactions: Hives, insect bites, and mild drug rashes calm down within hours.
- Adrenal insufficiency: Oral hydrocortisone replaces missing cortisol, preventing fatigue, low blood pressure, and electrolyte imbalance.
- Anti‑itch relief: Itch‑scratch cycles break when the inflammatory signal is turned off.
These benefits stem from the drug’s ability to balance the body’s stress response and immune activity.
Potential Side Effects and Precautions
Even a “mild” corticosteroid isn’t free of risk. Common side effects include:
- Skin thinning or striae when used on large areas.
- Temporary burning or stinging at the application site.
- Systemic effects (rare) such as elevated blood glucose, especially in diabetic patients.
- Suppressed adrenal function after prolonged high‑dose oral therapy.
Watch for signs of infection, as reduced immune activity can mask symptoms. If you notice unexpected weight gain, mood swings, or persistent fatigue, contact a clinician.
Comparison with Other Corticosteroids
| Attribute | Hydrocortisone | Betamethasone | Clobetasol |
|---|---|---|---|
| Potency (relative) | 1 (baseline) | 25-30 | 500-1000 |
| Typical concentration (cream) | 0.5-2.5% | 0.05% | 0.05% |
| Prescription status (US) | OTC ≤1%, otherwise Rx | Rx only | Rx only |
| Best for | mild-moderate skin irritation, adrenal insufficiency | moderate psoriasis, eczema | severe plaque psoriasis, lichen planus |
Choosing a steroid depends on the needed potency and the area being treated. Hydrocortisone remains the safest first‑line option for everyday skin issues.
Related Concepts and Broader Context
Understanding hydrocortisone also means grasping its place within the larger corticosteroid family. Corticosteroids include both glucocorticoids (like hydrocortisone) and mineralocorticoids (like fludrocortisone). They are regulated by the Food and Drug Administration (FDA), which sets limits on OTC concentrations and requires labeling for pregnancy safety.
When you hear “stress hormone,” think of cortisol produced by the adrenal gland. Hydrocortisone essentially replaces or supplements this natural hormone, which is why dosing must match the body’s daily rhythm-usually taken in the morning to mimic natural peaks.
For readers wanting deeper dives, the next logical topics are “Corticosteroid Potency Scale,” “Managing Long‑Term Steroid Therapy,” and “Differences Between Steroid Creams and Ointments.” Each expands on dosage nuances, safety monitoring, and formulation chemistry.
Frequently Asked Questions
Can I use OTC hydrocortisone on my face?
Yes, a 1% cream is safe for short‑term facial use, but limit application to once or twice a day and avoid the eye area. If you need stronger treatment, see a dermatologist for a prescription.
How long does it take to see relief?
Most people notice reduced redness and itching within 30 minutes to a few hours after topical application. Oral dosing for adrenal issues may take several days to stabilize blood cortisol levels.
Is hydrocortisone safe during pregnancy?
The FDA classifies low‑dose topical hydrocortisone as Category C, meaning risk cannot be ruled out. Always discuss with your OB‑GYN before starting any steroid, even OTC versions.
What are signs of steroid overuse?
Look for skin thinning, stretch marks, easy bruising, or unexplained weight gain. Systemic signs include high blood pressure, high blood sugar, and mood changes. If any appear, cut back and consult a doctor.
Can I apply hydrocortisone under a bandage?
Covering the area can increase absorption dramatically, turning a mild topical into a semi‑systemic dose. Use occlusion only if prescribed, and follow exact timing instructions.
How does hydrocortisone differ from prednisone?
Both are glucocorticoids, but prednisone is more potent (about 4× hydrocortisone) and is only available orally or intravenously. Hydrocortisone’s strength makes it ideal for skin and hormone‑replacement uses.
Do I need a doctor’s prescription for stronger hydrocortisone?
Yes. Concentrations above 1% for topical use and any oral formulation require a prescription in the United States. This ensures proper dosing and monitoring.







Philip Crider
September 23, 2025 AT 16:35Jackie Burton
September 24, 2025 AT 14:54Diana Sabillon
September 24, 2025 AT 21:10neville grimshaw
September 24, 2025 AT 21:41Carl Gallagher
September 25, 2025 AT 00:06bert wallace
September 25, 2025 AT 21:59Neal Shaw
September 26, 2025 AT 13:45Hamza Asghar
September 27, 2025 AT 06:05Karla Luis
September 28, 2025 AT 16:31jon sanctus
September 28, 2025 AT 22:53Kenneth Narvaez
September 30, 2025 AT 12:42Christian Mutti
October 1, 2025 AT 05:13Liliana Lawrence
October 2, 2025 AT 13:47Sharmita Datta
October 2, 2025 AT 22:15mona gabriel
October 4, 2025 AT 11:12Phillip Gerringer
October 4, 2025 AT 12:54jeff melvin
October 6, 2025 AT 05:04Matt Webster
October 7, 2025 AT 17:29Stephen Wark
October 8, 2025 AT 14:15Daniel McKnight
October 9, 2025 AT 01:59