When IBD Medications Stop Working, Surgery Becomes the Next Step
If you’ve been living with Crohn’s disease or ulcerative colitis for years, you know the toll it takes - constant pain, urgent bathroom trips, fatigue, and the fear of bleeding or flare-ups. When biologics, steroids, and other meds no longer bring relief, surgery isn’t a failure. It’s often the best chance to get your life back. About 75% of people with Crohn’s and 15-30% with ulcerative colitis will need surgery at some point, according to the Crohn’s & Colitis Foundation. The goal isn’t just to remove diseased tissue - it’s to stop the cycle of inflammation and give you freedom from symptoms.
Resection: Removing the Damaged Part
In Crohn’s disease, the inflammation doesn’t always affect the whole bowel. Surgeons often perform a bowel resection, cutting out the inflamed section - usually the end of the small intestine (ileum) or part of the colon - and reconnecting the healthy ends. This is called an anastomosis. The surgery can be done laparoscopically, using small incisions and a camera, which cuts hospital stays from 7 days down to 3-5. But resection doesn’t cure Crohn’s. The disease can come back right next to the reconnected area. Studies show up to 80% of patients see symptoms return within 10 years if they don’t stay on maintenance therapy. Still, for many, it’s a huge relief. One patient described it like this: “I hadn’t had a full night’s sleep in five years. After surgery, I slept through the night for the first time.”
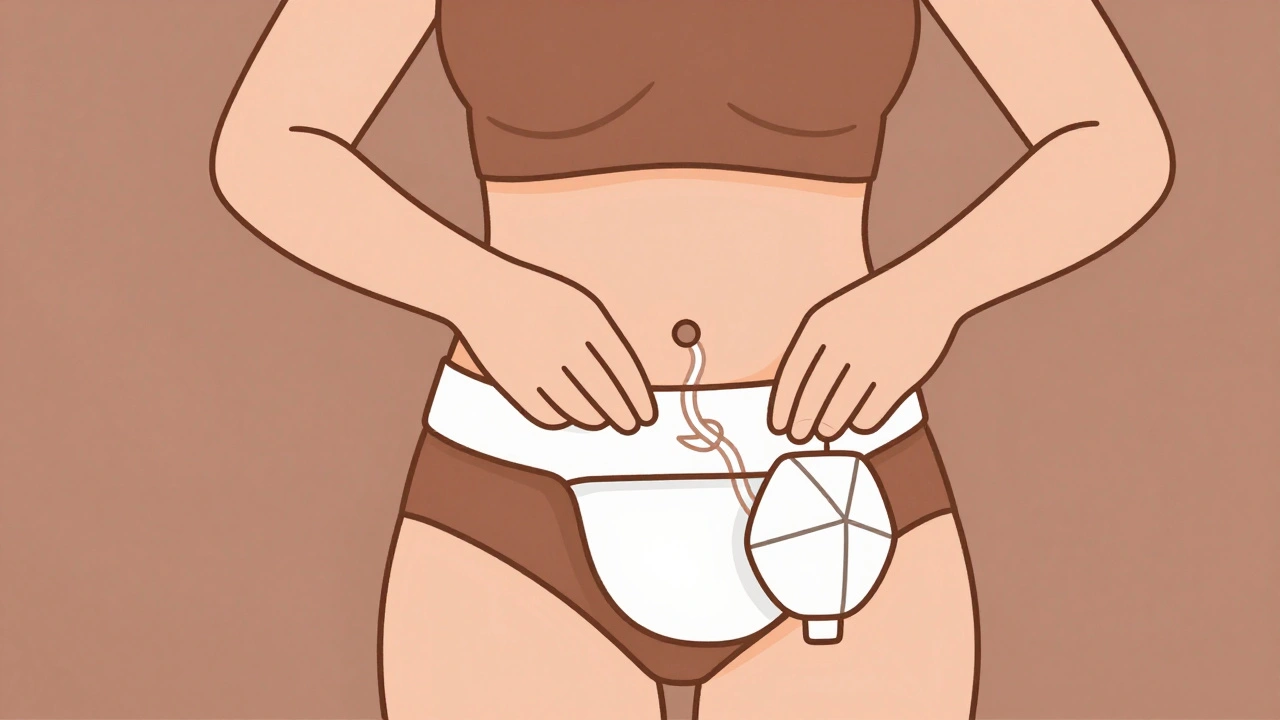
Ostomy: Living with a Stoma
An ostomy means creating an opening in the abdomen to let waste leave the body. There are two main types used in IBD: ileostomy and colostomy. For ulcerative colitis, a total proctocolectomy removes the entire colon and rectum. After that, you’ll need an ostomy - either temporary or permanent. The stoma is about the size of a quarter, sticking out 1-2 cm from your belly. Waste flows into a bag you wear. It sounds scary, but many patients say it’s life-changing. “I used to plan every outing around bathrooms,” one Reddit user wrote. “Now I just go. No anxiety. No leaks.”
Temporary ostomies are common after J-pouch surgery to let the new pouch heal. They usually last 8-12 weeks. Permanent ostomies are chosen when the rectum must be removed and a pouch isn’t possible - often in older patients, those with poor sphincter control, or if Crohn’s affects the anus. About 42% of permanent ostomy patients report high satisfaction at five years. Modern bags are thin, odor-proof, and stick well even during exercise. Brands like Convatec and Hollister offer discreet options that fit under regular clothes.
J-Pouch Surgery: The Alternative to a Permanent Ostomy
The most common surgery for ulcerative colitis is the ileal pouch-anal anastomosis, or J-pouch. Surgeons take the last 8-10 cm of your small intestine, shape it into a pouch, and attach it directly to your anus. That means you still go to the bathroom normally - just more often. Most people have 4-8 bowel movements a day after healing. The success rate is high: 80-90% of patients report being happy with their quality of life. But it’s not simple. J-pouch surgery usually takes two or three steps. First, the colon and rectum are removed and a temporary ileostomy is made. After 8-12 weeks, the pouch is built and connected. Then, after another few months, the stoma is closed. Each step means another hospital stay and recovery period.
Complications happen. About 20-40% of J-pouch patients get pouchitis - inflammation inside the pouch - which often needs antibiotics. Some need more surgeries later. And while most people regain control, nighttime seepage affects about one-third. Still, for those who qualify, it’s the gold standard. The American Society of Colon and Rectal Surgeons says it’s the first choice for anyone with healthy anal muscles and no Crohn’s.
Who Gets a J-Pouch - and Who Doesn’t
Not everyone is a candidate. If you’re over 70, your surgeon may recommend a permanent ileostomy instead. The risk of complications rises with age. If you have Crohn’s disease - even if it’s only in the colon - J-pouch surgery is usually avoided. Studies show up to half of Crohn’s patients with a J-pouch develop new inflammation around the pouch, forcing them back to a permanent stoma. Women who want to have children should know: fertility drops from 15% to 50-70% after J-pouch surgery. Men may face erectile dysfunction in 15-20% of cases. These aren’t side effects you can ignore. Talk to your surgeon about them before signing off.
Another big factor: your anal sphincter. If it’s weak from years of inflammation or previous surgeries, a J-pouch won’t work. You won’t be able to hold stool. In those cases, a permanent ileostomy is the safer, more reliable option. And if you’ve had multiple abdominal surgeries before, scar tissue can make J-pouch surgery too risky.
What Happens After Surgery - The Real Recovery
Surgery isn’t the end. It’s the start of a new routine. For J-pouch patients, it takes 6-12 months to get used to your new bowel habits. You’ll go more often at first - up to 10 times a day. Then it settles. You’ll need to drink 8-10 cups of water daily to avoid dehydration. High-fiber foods like raw veggies, nuts, and popcorn can block the pouch early on. Stick to soft, low-residue meals at first. Your dietitian will help you adjust.
If you have an ostomy, you’ll need training. A certified wound, ostomy, and continence nurse (WOCN) will show you how to change the bag, clean the skin, and prevent leaks. Skin irritation is the #1 complaint - 41% of negative reviews mention it. Using a barrier cream and fitting the wafer properly makes a huge difference. Many patients swear by the Convatec Adapt Mini Ostomy Belt ($45.99) to keep the bag secure during movement.
Watch for warning signs: fever over 101°F, sudden increase in output (more than 1,500 mL a day), or severe pain. These could mean infection, blockage, or a leak. Don’t wait. Call your surgeon right away.
Support, Tools, and What’s New
You’re not alone. The United Ostomy Associations of America has over 25,000 members. Online, r/IBD on Reddit has nearly 30,000 people sharing tips on everything from pouch diets to finding the best bag adhesive. Many say finding a good WOCN before surgery is the most important thing they did.
Technology is improving fast. In 2023, the FDA approved the first smart ostomy bag - OstoLert by ConvaTec - that alerts you if it’s leaking. Robotic surgery for J-pouches is now used at top hospitals like Mayo Clinic, cutting operation time by 20% and reducing complications. Researchers are even testing fecal microbiome transplants to prevent pouchitis, with early results showing a 40% drop in inflammation.
Costs vary. Medicare reimburses about $28,500 for a J-pouch procedure and $18,200 for an ostomy reversal. Most insurance covers it, but out-of-pocket costs for bags and supplies can add up. Many manufacturers offer free samples and discount programs.
Is Surgery Right for You?
Surgery isn’t a decision to rush into. But if you’re tired of being controlled by your disease, it’s worth exploring. Talk to an IBD specialist surgeon - not just a general colorectal surgeon. Centers that do over 50 IBD surgeries a year have 35% fewer complications. Ask about their success rates, pouch retention rates, and how many patients they’ve helped return to normal life. Bring your list of questions. Bring a family member. This is about your future. And for many, it’s the best decision they ever made.





Joel Deang
December 3, 2025 AT 07:32Arun kumar
December 3, 2025 AT 18:36Zed theMartian
December 4, 2025 AT 23:05Shannara Jenkins
December 6, 2025 AT 07:58Roger Leiton
December 6, 2025 AT 17:51Laura Baur
December 8, 2025 AT 14:45Jack Dao
December 9, 2025 AT 12:14dave nevogt
December 10, 2025 AT 16:20Steve World Shopping
December 12, 2025 AT 16:05Rebecca M.
December 13, 2025 AT 16:30Elizabeth Grace
December 14, 2025 AT 22:24Steve Enck
December 16, 2025 AT 12:12मनोज कुमार
December 16, 2025 AT 12:18