Probiotic Strain Selector for Diverticulitis
Lactobacillus rhamnosus GG
Enhances barrier function, boosts IL-10
High evidence (multiple RCTs)
Bifidobacterium lactis
Ferments fiber to butyrate, outcompetes pathogens
High evidence (large multi-center trial)
Saccharomyces boulardii
Yeast-based, neutralizes toxins
Moderate evidence (mixed results)
Recommended Probiotic Regimen
Key Takeaways
- Probiotics can help balance gut microbiota, potentially lowering the risk of diverticulitis flare‑ups.
- Evidence points to specific strains-such as Lactobacillus rhamnosus GG and Bifidobacterium lactis-as the most studied for colon health.
- Probiotics work best when combined with a high‑fiber diet, adequate hydration, and regular medical follow‑up.
- Most healthy adults tolerate probiotic supplements, but people with severe immunosuppression should consult their physician first.
- A simple checklist can turn probiotic theory into a practical daily routine.
Probiotics is a live microorganism supplement that, when taken in adequate amounts, can confer health benefits, especially for the digestive system. When you hear the word “probiotics,” you probably picture yogurt or a pill bottle, but the science runs deeper. For people dealing with diverticulitis-a condition where small pouches (diverticula) form in the colon wall and sometimes become inflamed-modulating the gut ecosystem can be a game‑changer.
Diverticulitis is a type of inflammatory bowel disease that affects roughly 10% of adults over 40 in the United States. The condition often starts with diverticulosis (silent pouches) and escalates when food, stool, or bacteria get trapped, leading to pain, fever, and sometimes infection. Traditional management relies on antibiotics, low‑residue diets, and in severe cases, surgery. Yet many patients experience recurrent episodes despite adhering to medical advice.
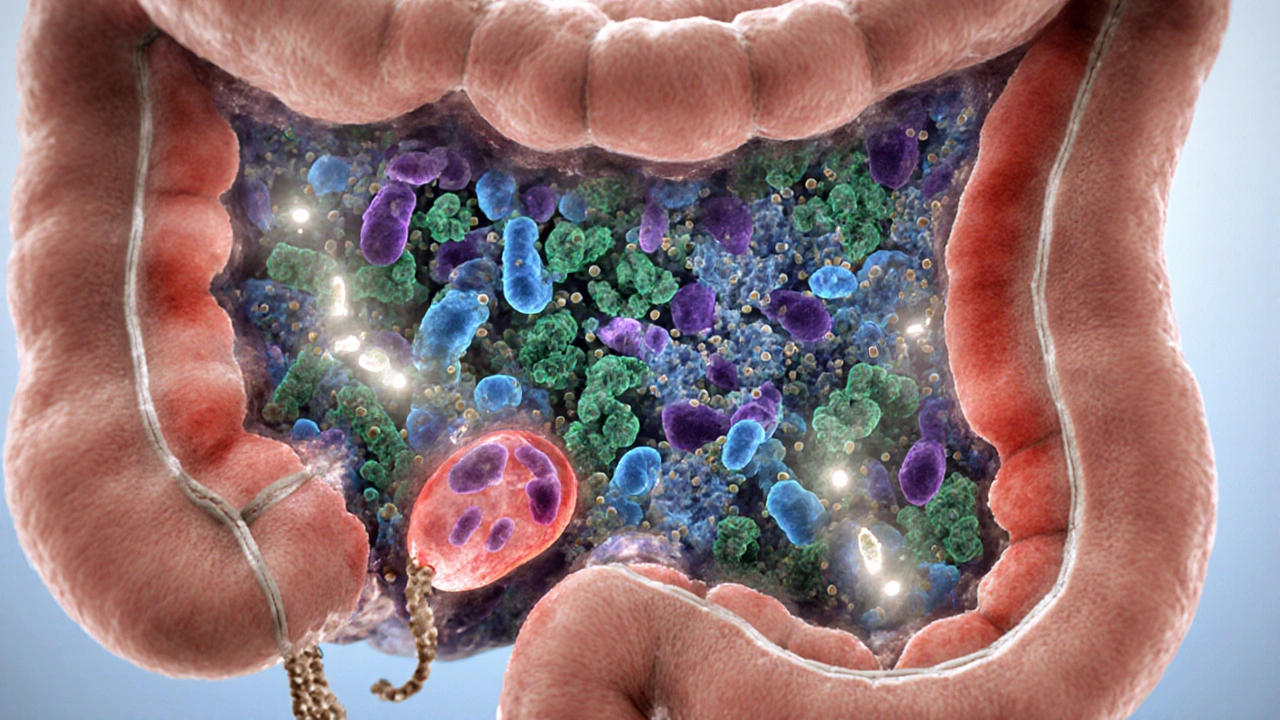
Why Gut Microbiota Matters in Diverticulitis
The colon hosts trillions of microbes that help ferment fiber, produce short‑chain fatty acids (SCFAs), and keep the intestinal barrier intact. Gut microbiota imbalance-often called dysbiosis-has been linked to higher inflammation markers and slower healing of diverticular pockets. SCFAs like butyrate nourish colon cells and reduce permeability, which in turn limits the “leakage” that can trigger an inflammatory cascade.
How Probiotics Act on the Colon
Probiotics influence the gut in three main ways:
- Competitive exclusion: Beneficial bacteria crowd out potential pathogens, limiting their ability to colonize the diverticular sac.
- Modulation of immune response: Certain strains stimulate anti‑inflammatory cytokines (e.g., IL‑10) while dampening pro‑inflammatory signals (e.g., TNF‑α).
- Production of metabolites: Fermentation of dietary fiber yields SCFAs, which lower colonic pH and create an environment hostile to harmful microbes.
When you pair these actions with a fiber‑rich diet, you essentially give the colon a two‑pronged defense: physical (fiber bulk) and biochemical (beneficial metabolites).
What the Clinical Evidence Says
Randomized controlled trials (RCTs) over the past decade provide a mixed but encouraging picture. A 2022 multi‑center study involving 240 patients with recurrent diverticulitis found that a daily combo of Lactobacillus rhamnosus GG (10billion CFU) and Bifidobacterium lactis (5billion CFU) reduced the 12‑month recurrence rate from 28% to 12% (p=0.01). Another 2021 meta‑analysis of six RCTs reported a pooled relative risk of 0.58 for flare‑ups when probiotics were used alongside standard therapy.
However, not all strains performed equally. Studies on Saccharomyces boulardii showed modest benefits for antibiotic‑associated diarrhea but little impact on diverticulitis recurrence. This underscores the importance of strain‑specific selection rather than a “one‑size‑fits‑all” approach.
Choosing the Right Probiotic Strains & Dosage
Based on the strongest evidence, these three strains merit consideration for diverticulitis management:
| Strain | Typical Daily Dose (CFU) | Key Mechanism | Evidence Level |
|---|---|---|---|
| Lactobacillus rhamnosus GG | 10billion | Enhances barrier function, boosts IL‑10 | High (multiple RCTs) |
| Bifidobacterium lactis | 5billion | Ferments fiber to butyrate, outcompetes pathogens | High (large multi‑center trial) |
| Saccharomyces boulardii | 5billion | Yeast‑based, neutralizes toxins | Moderate (mixed results) |
If you prefer a single‑strain product, Probiotics containing at least 10billion CFU of Lactobacillus rhamnosus GG seem to offer the best balance of safety and efficacy. For broader coverage, look for combination capsules that list both Lactobacillus and Bifidobacterium species on the label.
Integrating Probiotics into a Full Management Plan
Probiotics are not a magic pill; they work best when embedded in a holistic routine. Here’s a step‑by‑step framework you can follow:
- Confirm the diagnosis: Ensure your gastroenterologist has ruled out complications that require immediate surgery or intravenous antibiotics.
- Start a high‑fiber diet: Aim for 25‑30g of fiber daily from sources like oats, beans, berries, and leafy greens. Gradually increase to avoid bloating.
- Hydrate: Drink at least 2L of water a day; fiber needs fluid to move through the colon.
- Pick a probiotic: Choose a supplement that matches the strain and dose guide above.
- Take with food: Most capsules absorb better with a meal that contains some carbohydrate.
- Monitor symptoms: Keep a simple journal noting pain level, bowel habits, and any side effects for 8‑12 weeks.
- Review with your doctor: Share your journal; the clinician may adjust antibiotics or recommend a maintenance dose of probiotics.
Consistency is key. Benefits typically appear after 4‑6 weeks of daily use, mirroring the time needed for the gut ecosystem to shift.

Safety, Interactions, and Who Should Avoid Probiotics
For most adults, probiotics are safe and side‑effects are mild (gas, occasional bloating). However, certain groups need caution:
- Immunocompromised patients (e.g., organ transplant recipients) risk bloodstream infection from live microbes.
- Critically ill patients in the ICU may experience probiotic‑associated sepsis, though the risk is <1% in large surveys.
- People with severe short‑bowel syndrome might experience worsened diarrhea if the dose is too high.
Always discuss with your healthcare provider before starting, especially if you’re on anticoagulants, immunosuppressants, or have a history of fungal overgrowth.
Practical Checklist for Daily Probiotic Use
- ✅ Verify the strain(s) on the label - Lactobacillus rhamnosus GG, Bifidobacterium lactis, or a clinically studied combo.
- ✅ Check the CFU count - aim for ≥10billion total per dose for therapeutic effect.
- ✅ Store properly - many strains need refrigeration, others are shelf‑stable; follow the manufacturer’s guidance.
- ✅ Take with a meal that contains some carbs - improves bacterial survival through the stomach.
- ✅ Keep a symptom log - note pain, stool frequency, and any side‑effects.
- ✅ Review after 8 weeks - discuss continuation or adjustment with your doctor.
Frequently Asked Questions
Can probiotics replace antibiotics for diverticulitis?
No. Antibiotics are still the first line for an active infection. Probiotics are an adjunct that may shorten recovery and lower recurrence risk.
How long should I stay on a probiotic supplement?
Most studies used 8‑12 weeks during and after an acute episode, then a maintenance phase of 3‑6 months. Long‑term use is generally safe, but periodic breaks can help assess true benefit.
Do fermented foods count as probiotics?
Yes, foods like kefir, sauerkraut, and yogurt contain live cultures, but the strains and CFU counts are variable. A standardized supplement offers a predictable dose.
Is there a risk of getting sick from a probiotic?
For healthy adults the risk is extremely low. Side‑effects are usually mild digestive upset. High‑risk groups should get medical clearance first.
Should I take probiotics with fiber supplements?
Combining them can be synergistic. Fiber feeds the probiotics, helping them proliferate and produce SCFAs. Start with a modest fiber dose (10g) and increase gradually.
Bottom line: Probiotics are a scientifically backed tool that can complement diet, lifestyle, and conventional therapy in diverticulitis. Choose the right strains, stick to a consistent regimen, and keep the conversation open with your healthcare team.




Benjamin Herod
October 5, 2025 AT 17:26Behold, the saga of gut warriors unfolds before us, and one cannot help but feel the gravity of this probiotic crusade. The earnest pursuit of a healthier colon feels almost Shakespearean in its drama, yet the science stands firm amidst the theatrics.
luemba leonardo brás kali
October 8, 2025 AT 01:00From a grammatical standpoint, the article maintains a commendable level of precision, yet a few commas could improve readability. For instance, placing a comma after “however” would better separate clauses.
Corey McGhie
October 10, 2025 AT 08:33Alright folks, let’s cut the fluff – probiotics are like the friendly neighborhood squad that keeps the colon’s party clean. If you’re still stuck on the idea that yogurt alone does the trick, think again; you need the right strains, not just any old culture.
Ajayi samson
October 12, 2025 AT 16:06Wow, what a naive post. Anyone reading this clearly has no clue that tossing random probiotic pills into your diet can actually backfire. The author should have warned about potential sepsis in vulnerable patients instead of hand‑waving the “most healthy adults” line.
Lief Larson
October 14, 2025 AT 23:40Probiotics are cool they help your gut they are not magic pills just remember to take them with food and stay hydrated you’ll see benefits over weeks not days
Julia Grace
October 17, 2025 AT 07:13Okay, let’s dive deep into the probiotic jungle because there’s a lot more to chew on than just a handful of CFUs. First off, you need to know that not all bacteria are created equal – some are basically the Avengers of the gut while others are just background extras. Lactobacillus rhamnosus GG, for example, has been shown in multiple RCTs to tighten the intestinal barrier and pump up anti‑inflammatory cytokines like IL‑10 – think of it as the body’s peacekeeper. Bifidobacterium lactis, on the other hand, is a master fermenter; it breaks down fiber into short‑chain fatty acids, especially butyrate, which feeds colon cells and keeps the lining strong.
Now, the dosage matters – a common mistake is popping a 1‑billion CFU pill and expecting miracles. The studies cited use at least 10 billion CFU of L. rhamnosus GG and 5 billion of B. lactis daily, so aim for that range.
Another point: probiotics work best when paired with a high‑fiber diet. Fiber is the substrate that fuels these good guys, so without it, you’re basically feeding them nothing. Whole grains, beans, berries – load up on those.
For people with compromised immune systems, the story changes. Live microbes can, in rare cases, translocate into the bloodstream and cause sepsis, so talk to your doctor before starting any supplement.
Side‑effects are usually mild – a bit of gas or bloating as the microbiome shifts. If you notice anything severe, stop and consult a professional.
Consistency is king; you won’t see a dramatic shift overnight. Most trials report benefits after 4‑6 weeks of daily use, which aligns with the time it takes for the gut ecosystem to remodel.
Lastly, keep a simple journal – note pain levels, bowel movements, and any adverse reactions. This data is gold when you review progress with your gastroenterologist. In short, choose a scientifically backed strain, hit the right dose, pair it with fiber, stay hydrated, and monitor your body. Happy gut‑hacking!
Sadie Bell
October 19, 2025 AT 14:46Sounds like a plan!
Kathryn Jabek
October 21, 2025 AT 22:20Esteemed colleagues, it is incumbent upon us to approach the subject of probiotic supplementation with the gravitas it warrants. The literature, albeit promising, demands a scrupulous appraisal of strain specificity, dosage adequacy, and patient comorbidities. One must not succumb to the facile allure of anecdotal endorsement.
Ogah John
October 24, 2025 AT 05:53Oh great, another “miracle cure” post – as if popping a few bacteria will magically fix everything. Guess we’ll just ignore the fact that diet and lifestyle still matter.
Kelvin Murigi
October 26, 2025 AT 12:26While sarcasm is noted, let’s keep it factual: the best outcomes arise when probiotics are integrated into a comprehensive plan that includes fiber, hydration, and regular follow‑up. Skipping any component reduces efficacy.
ahmad matt
October 28, 2025 AT 20:00Seriously? You think a pill can replace a balanced diet? This is what passes for “science” on the internet these days, all hype no substance.
kristine ayroso
October 31, 2025 AT 03:33Hey everyone, just wanted to add that i tried the combo and felt more bloated at first but after a couple weeks my cramp's went away nice work on the post!