Every pill, liquid, or patch you take comes with a label. But how many of you actually read it - really read it - before taking anything? If you’ve ever taken medicine and wondered, "Was that the right dose?" or "Should I take this with food?", you’re not alone. Misreading medication labels is one of the most common reasons people end up in the emergency room. It’s not about being careless. It’s about confusing language, tiny print, and hidden details that can cost you your health.
What’s on the Label? The Basics You Can’t Ignore
Medication labels, whether prescription or over-the-counter, follow strict rules set by the FDA. For prescription drugs, the label includes 16 sections, but you only need to focus on a few key ones. For OTC meds, it’s simpler: the Drug Facts box is your lifeline.Here’s what you must check every time:
- Active Ingredient(s): This is the chemical that does the work. If you’re taking more than one medicine, check this first. Many cold and flu pills contain acetaminophen. Taking two different products with it can lead to a dangerous overdose - the #1 cause of liver failure from medication errors.
- Dosage: This tells you exactly how much to take. Look for numbers like "500 mg" or "10 mL." Don’t guess. If it says "take two tablets," don’t take one because "it feels like enough."
- Directions: This is where people slip up. "Take every 6 hours" means four times a day - not three. "Take with food" isn’t optional. Some drugs irritate your stomach if taken on an empty stomach. Others won’t absorb properly without food.
- Warnings: This section is buried, but it’s critical. It tells you what not to mix with the drug (like alcohol or other meds), what side effects to watch for, and who shouldn’t take it (pregnant women, people with kidney disease, etc.). Skipping this is like driving without checking your mirrors.
- Expiration Date: Expired meds don’t just lose strength - some become toxic. Liquid antibiotics, insulin, and nitroglycerin are especially risky after expiration. Pharmacy-dispensed prescriptions usually expire one year after filling, even if the bottle says 2027.
Understanding Dosage: It’s Not Always "One Pill"
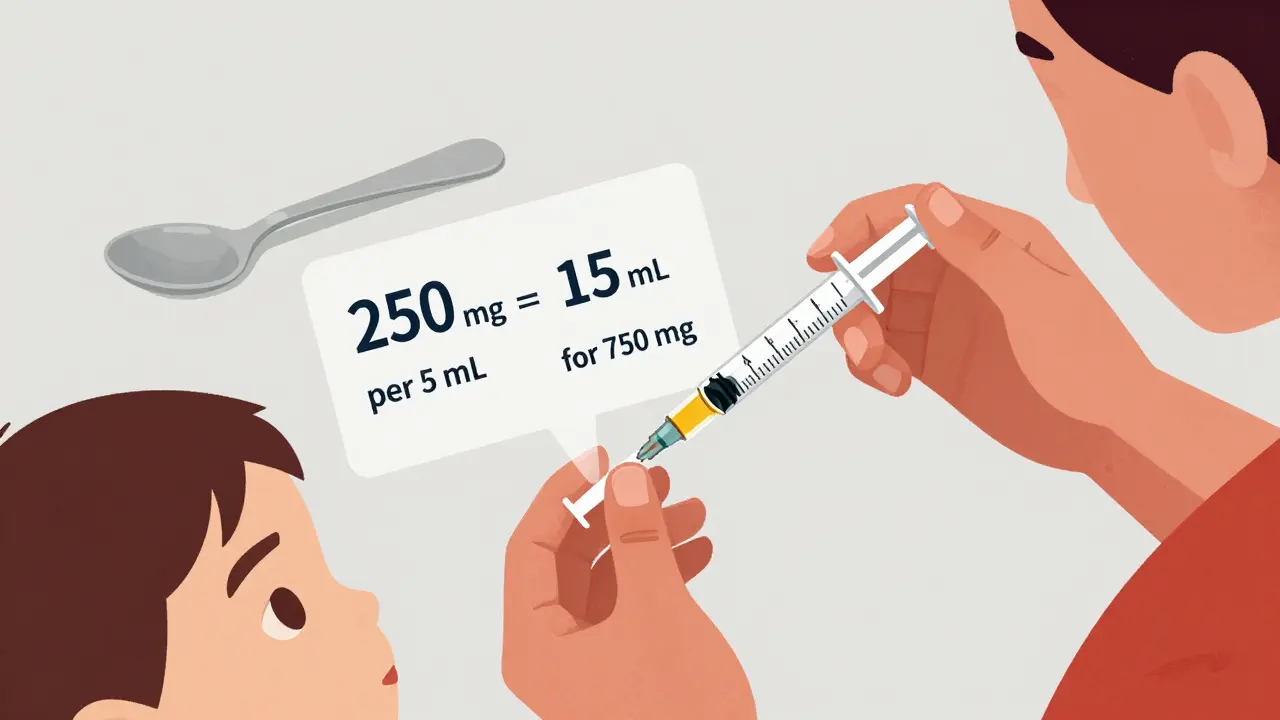
Most people assume "dose" means one pill. But that’s not always true. Some medicines are measured by weight - especially for kids. If your child weighs 20 kg, the label might say "5 mg per kg," meaning you need 100 mg total. If the tablet is 25 mg, you give four. No guesswork.For liquid medicines, concentration is everything. A label might say: "250 mg per 5 mL". That means each milliliter has 50 mg. If the doctor ordered 750 mg, you need to calculate: 750 ÷ 50 = 15 mL. That’s three teaspoons - not one. But here’s the trap: household spoons vary wildly. A teaspoon from your kitchen could hold anywhere from 2.5 to 7.3 mL. That’s a 200% difference. Always use the syringe or cup that came with the medicine. If it didn’t come with one, ask the pharmacist for one. They’re free.
And don’t assume "as needed" means "whenever you feel like it." For painkillers, "take as needed for pain, up to 4 times daily" means maximum four doses in 24 hours - no more. Taking one at 8 a.m., another at noon, another at 4 p.m., and another at 10 p.m. is fine. Taking two at 8 a.m. because "it didn’t work"? That’s how people end up in the hospital.
Why People Get It Wrong - And How to Avoid It
A 2022 study found that 42% of adults misread liquid medicine concentrations. Among parents of young children, that number jumped to 68%. Why? They’re tired. They’re stressed. They’re trying to juggle work, kids, and appointments. But the biggest reason? They don’t double-check.Here’s what happens in real life:
- A mom gives her 3-year-old amoxicillin. The bottle says "250 mg per 5 mL." The doctor prescribed 500 mg. She thinks, "Two 5 mL doses = 500 mg," so she gives 10 mL. But she uses a kitchen spoon, not the syringe. The spoon holds 7 mL. She gives 7 mL × 2 = 14 mL - that’s 700 mg. Too much. She doesn’t realize until the child vomits.
- A man with high blood pressure takes his pill at 8 a.m. He forgets. At 10 a.m., he takes another, thinking he missed it. He doesn’t see the warning: "Do not take more than once daily." He ends up with dangerously low blood pressure.
- A woman takes Tylenol for a headache. Then she takes a cold medicine. Both have acetaminophen. She doesn’t know. She takes six doses in 12 hours. Her liver starts failing.
These aren’t rare cases. They happen every day.
Here’s how to stop it:
- Read it twice. Once when you pick it up. Once before you take it.
- Ask the pharmacist. They’re trained to explain labels. Say: "Can you walk me through the directions? I want to make sure I’m doing it right."
- Write it down. Copy the dosage and timing onto a sticky note. Put it on your bathroom mirror or fridge.
- Use a pill organizer. Pre-filled ones with alarms help you track when you’ve taken your dose.
- Keep a list. Write down every medicine you take - including vitamins and supplements. Bring it to every doctor visit.
The Hidden Dangers: Overlapping Ingredients and Drug Interactions
One of the most dangerous mistakes is taking multiple medicines with the same active ingredient. You might take Advil for pain. Then you take a nighttime cold remedy. Both have ibuprofen. You double up. Your stomach bleeds. Your kidneys get damaged.Even "natural" products can clash. St. John’s Wort, a common herbal supplement for mood, can cancel out birth control pills and make antidepressants ineffective. If you’re taking anything beyond a daily multivitamin, ask your pharmacist if it interacts with your prescriptions.
And don’t forget alcohol. Many antibiotics, painkillers, and sleep aids warn against drinking. The label says "avoid alcohol." That means no beer, no wine, no whiskey. Even one drink can cause dizziness, liver damage, or breathing problems.
What’s Changing - And What to Expect Soon
The FDA is pushing for simpler labels. By 2024, you’ll start seeing QR codes on prescription bottles. Scan it with your phone, and you’ll get a video showing how to take the medicine - in plain language, with visuals. Some are already testing this with insulin and blood thinners. Early results show a 37% drop in errors.By 2027, high-alert drugs - like opioids, insulin, and blood thinners - will have standardized color-coding and warning icons. No more guessing what the symbols mean. Red = danger. Yellow = caution. Green = safe.
Also, by law, all high-risk meds must now use "plain language" - no medical jargon. "Administer orally" becomes "swallow the pill." "Concomitant use" becomes "don’t take with other painkillers."
Your Action Plan: 5 Steps to Never Misread a Label Again
1. Stop and read. Don’t grab the bottle and rush. Sit down. Look at it like it’s a map. 2. Check the active ingredient. If you’re taking more than one medicine, write them all down. Use a free app like Medisafe or MyTherapy to scan barcodes and check for overlaps. 3. Measure correctly. Never use a spoon. Use the syringe. If you lost it, go back to the pharmacy. They’ll give you a new one. 4. Ask one question. Before leaving the pharmacy, ask: "Is there anything here I need to watch out for?" That one question saves lives. 5. Review every 3 months. Your meds change. Your weight changes. Your liver function changes. Re-read your labels every time you refill.Medication labels aren’t just paperwork. They’re your protection. They’re the last line of defense between you and harm. You wouldn’t drive a car without reading the manual. Don’t take medicine without reading the label.
What should I do if I can’t read the small print on my medicine label?
Ask your pharmacist for a large-print copy. Most pharmacies will print a bigger version for free. You can also request an audio version through your pharmacy’s patient services. Some pharmacies even offer magnifying label readers. Don’t struggle with blurry text - it’s not worth the risk.
Can I split pills if the dose seems too high?
Only if the pill is scored (has a line down the middle) and your doctor or pharmacist says it’s safe. Many pills, especially capsules or time-release tablets, shouldn’t be split. Splitting them can change how the drug works or make it unsafe. Always ask before cutting a pill.
Why do some labels say "take on an empty stomach"?
Some medicines are absorbed better without food. Others get blocked by fats or acids in your stomach. "Empty stomach" usually means 1 hour before or 2 hours after eating. If you take it with food, it might not work as well - or it could cause side effects like nausea.
What if the label says "take daily" but my doctor said "take every other day"?
Call your pharmacy immediately. The label might be wrong - or your doctor’s instructions weren’t passed on correctly. Never guess. Medication errors from conflicting instructions are common. Get it clarified before you take another dose.
Are generic drugs labeled the same way as brand-name ones?
Yes. By law, generic drugs must have the same active ingredient, strength, dosage form, and directions as the brand-name version. The only differences are the inactive ingredients (like fillers) and the packaging. The Drug Facts box and warnings are identical.
What should I do if I accidentally take too much?
Call Poison Control at 1-800-222-1222 (U.S.) or your local emergency number. Don’t wait for symptoms. Don’t try to induce vomiting. Have the medicine bottle ready - they’ll need the active ingredient and dosage. If you’re unsure, go to the ER. Overdoses can be silent at first.




Emma Duquemin
December 30, 2025 AT 02:24Okay but have you ever tried reading a prescription label after 3 a.m. while holding a screaming toddler and your coffee’s cold? The print is smaller than my will to live. I used to wing it until my kid threw up after amoxicillin because I used a dinner spoon. Now I keep a syringe in my purse like a weapon. Pharmacist? Best. Human. Ever.
Kevin Lopez
December 31, 2025 AT 11:14Active ingredient misidentification is the primary driver of iatrogenic hepatotoxicity in non-prescription polypharmacy cases. The FDA’s Drug Facts box is underutilized due to cognitive load and low health literacy. Recommend structured patient education via pharmacy-based counseling protocols.
Fabian Riewe
January 2, 2026 AT 04:21My grandma used to say, ‘If you’re not sure, don’t swallow.’ Best advice I ever got. I keep a little notebook next to my pill organizer now - active ingredient, dose, time, and whether I ate. Took me 3 years to stop guessing. You’re not dumb for not knowing this stuff - the system’s just designed to confuse you.
Duncan Careless
January 2, 2026 AT 16:44i’ve been takin meds for 12 years and still mess up sometimes. the labels are too small, the wording is weird, and no one ever explains it like you’re a person. last month i took 2 ibuprofen at once cause i thought ‘as needed’ meant ‘whenever i hurt’. i didn’t know it was max 4x/day. dumb mistake. i asked my pharmacist for a big print copy and now i use the app. it’s not hard, just need a lil help.
Nicole K.
January 3, 2026 AT 15:00If you can’t read the label, you shouldn’t be taking the medicine. It’s that simple. You’re not too busy or too tired - you’re just careless. This isn’t hard. Read it. Or don’t take it. Your life is not a gamble.
Sharleen Luciano
January 4, 2026 AT 13:14Let’s be real - the FDA’s ‘plain language’ initiative is a PR stunt. I’ve seen the new labels. They still say ‘take on an empty stomach’ and then bury the definition in a footnote. Meanwhile, the actual dosage instructions are printed in 5-point font under a QR code that only works if you’ve got the latest iOS and a steady hand. The system isn’t broken - it’s designed to exclude. People who can’t afford smartphones, glasses, or time to decode this? They’re collateral damage. And we call it ‘health literacy’ like it’s their fault.
I’ve worked in pharmacy for 18 years. The real solution? Mandatory verbal confirmation by a licensed pharmacist before every dispense. Not a QR code. Not a pamphlet. A human saying: ‘This is what you’re taking, why, when, and what happens if you mess up.’ But that costs money. And nobody wants to pay for safety.
And don’t get me started on ‘natural’ supplements. I had a woman come in last week taking St. John’s Wort with her SSRIs because ‘it’s herbal, so it’s safe.’ She was dizzy, nauseous, and convinced the world was spinning. I asked her if she’d read the interaction warning. She said, ‘I didn’t think it applied to me.’ That’s not ignorance. That’s systemic failure.
And yes, I know the FDA is rolling out color-coding. Red for danger. Yellow for caution. Green for safe. Cute. But what about the colorblind? What about the elderly with macular degeneration? What about the person who’s just too tired to care? Labels aren’t the problem - our entire approach to medication safety is. We treat patients like puzzles to be solved, not humans to be protected.
So yes, read the label. But also demand better. Demand bigger print. Demand audio instructions. Demand pharmacists paid to talk to you, not just scan barcodes. Because if your life depends on a tiny font and a QR code, we’ve already lost.
Amy Cannon
January 5, 2026 AT 16:58As a native speaker of English with a postgraduate degree in biomedical ethics, I must emphasize that the linguistic complexity of pharmaceutical labeling remains an egregious barrier to equitable healthcare access, particularly among non-native speakers, cognitively impaired populations, and those with low socioeconomic status. The FDA's recent standardization initiatives, while commendable in intent, still rely upon a paradigm of individual responsibility that fundamentally neglects structural inequities in health literacy infrastructure. For instance, the proposed QR code system presupposes digital literacy, device ownership, and network reliability - privileges not universally accessible. Furthermore, the use of colloquial replacements such as 'swallow the pill' may inadvertently infantilize adult patients, particularly in cultures where direct medical instruction is perceived as authoritative and respectful. The true solution lies not in simplifying language, but in institutionalizing multilingual, multimodal, and culturally competent patient education programs embedded within the dispensing process - preferably delivered by trained bilingual pharmacy technicians with cultural liaison training. Until then, we are merely decorating the prison walls while the inmates remain locked inside.
Himanshu Singh
January 5, 2026 AT 22:25i never read the label till i got sick from mixing tylenol and cold meds. now i use an app that scans and tells me if its same ingrediant. saved my life. also, ask pharmacist, they dont bite. trust me, i am from india, we dont have this habit here, but usa teach me. thank you for post.