Getting the medicine you need shouldn’t mean choosing between rent and refills. For millions of Americans, patient assistance programs from drug companies are the only way to afford life-saving prescriptions. But getting approved isn’t simple. Eligibility rules vary wildly between companies, and even small mistakes can get your application denied. This isn’t about charity-it’s about a system built to help people who fall through the cracks. And if you’re struggling to pay for your meds, you need to know exactly how it works.
Who Qualifies for Drug Company Assistance?
The biggest myth about these programs is that they’re only for the completely uninsured. That’s not true. While some programs require you to have no insurance at all, others are designed for people with insurance that still leaves them paying hundreds or thousands out of pocket. The real common thread? Income. Nearly all programs use the Federal Poverty Level (FPL) as their baseline. For 2023, 500% of FPL means $75,000 a year for a single person and $153,000 for a family of four. But here’s where it gets messy: some companies set the bar lower. Pfizer’s program for basic medications like Eucrisa caps eligibility at 300% FPL ($43,200 for one person). For cancer drugs, they raise it to 500-600% FPL. GSK’s cutoff is $58,650 for a single person. So even if you make $60,000, you might qualify for one drug but not another-depending on the manufacturer.Insurance Status: The Biggest Trap
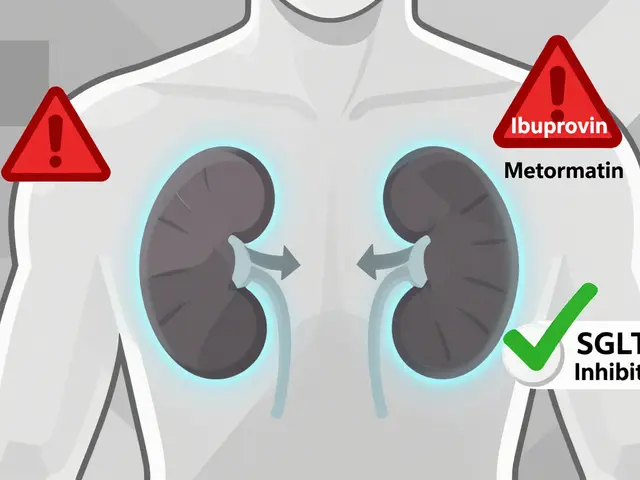
This is where most people get stuck. If you have Medicare, Medicaid, or private insurance, you might assume you’re automatically disqualified. Not necessarily. But the rules are confusing. Most manufacturer programs (like those from Pfizer, Merck, and AbbVie) require you to be uninsured or underinsured. That means if you have commercial insurance that covers your drug, you’re usually out of luck. But here’s the twist: if your insurance requires you to try a cheaper alternative first (called step therapy), or if your plan has a high deductible and you’ve hit your out-of-pocket maximum, some companies will still help. Medicare Part D beneficiaries face the toughest hurdles. To qualify for help from companies like Takeda, you must first apply for Medicare’s Extra Help program and get denied. Only then can you apply for the drug company’s program. And even then, your income must be below 150% FPL ($20,385 for one person). That creates a dangerous gap: people earning between $18,347 and $20,385 often get turned down by both programs. No help at all.What You Need to Apply
You can’t just fill out a form online and get approved. Every program requires hard proof. Here’s what most ask for:- Proof of income: W-2s, pay stubs, tax returns, or Social Security award letters
- Proof of residency: Utility bill, lease, or driver’s license showing a U.S. address
- Proof of prescription: A signed form from your doctor confirming the medication and dosage
- Proof of insurance status: Medicare card, insurance ID card, or a letter stating you have no coverage
How Different Companies Compare
Not all programs are built the same. Here’s how the big players stack up:| Company | Max Income (Single Person) | Insurance Eligibility | Medicare Part D Allowed? | Re-Enrollment Required |
|---|---|---|---|---|
| Pfizer | $77,760 (for specialty drugs) | Uninsured or underinsured only | Yes, after Extra Help denial | Annually |
| Merck | 500% FPL ($75,000) | Uninsured; hardship exceptions for insured | Yes, with denial from Extra Help | Annually |
| GSK | $58,650 | Uninsured or underinsured | Yes, with Extra Help denial | Every 12 months |
| AbbVie | Varies by drug (up to 600% FPL) | Uninsured or underinsured | Yes, after Extra Help denial | Every 6-12 months |
| Takeda | 150% FPL ($20,385) | Only if Extra Help denied | Yes, mandatory denial required | Every 12 months |
Notice something? Most programs don’t help if you’re on commercial insurance-even if your copay is $500 a month. And if you’re on Medicare, you need to jump through extra hoops. The system is designed to prioritize the uninsured, but it leaves a lot of people stranded.
Why Applications Get Denied
It’s not just about income. The paperwork is the real killer. Here’s what actually gets people turned down:- Missing doctor signature on forms (28-day average wait time for physician verification)
- Outdated pay stubs (must be within 90 days)
- Incorrect household size (52% of errors in CMS data)
- Not submitting a denial letter from Medicare Extra Help
- Using gross income instead of MAGI
What Happens After You’re Approved
Once you’re in, it’s not automatic forever. Most programs require you to reapply every year. For specialty drugs like cancer treatments, you might need to re-verify every three months. That means updating your income, submitting new prescriptions, and getting your doctor to sign off again. But here’s the good part: once approved, medications usually arrive within 72 hours. Some programs even ship directly to your home. And unlike Medicare Part D, the value of the free drugs doesn’t count toward your out-of-pocket maximum. That means if you’re trying to reach catastrophic coverage, PAPs don’t help you get there faster.What’s Changing in 2025 and Beyond
The rules are shifting. Starting in 2025, Medicare Part D will cap out-of-pocket drug costs at $2,000 a year. That’s a game-changer. Experts predict 35-40% fewer Medicare beneficiaries will need PAPs after that. But that doesn’t mean the programs will disappear. Drug companies are already launching new “commercial PAPs” for people with private insurance who face high copays. Pfizer and AbbVie now offer these for select drugs. And more are coming. These programs don’t require you to be uninsured-they just need you to show your insurance didn’t cover the full cost. The real question is whether these programs are helping-or just letting drug companies avoid lowering prices. Critics say PAPs let companies charge $100,000 for a cancer drug, then say, “Look, we’re helping!” while never touching the price tag. But for the person holding that prescription, it doesn’t matter why the help exists. It matters that it’s there.
How to Get Started
Don’t wait until you’re out of pills. Start now:- Find your drug’s manufacturer. Google “[drug name] patient assistance program.”
- Go to their official website. Avoid third-party sites-many are scams.
- Use their online portal or download the application form.
- Gather your documents: income proof, ID, prescription, insurance info.
- Ask your doctor to complete their section. Don’t wait-this is the slowest part.
- Submit. If denied, read the reason. Fix it. Apply again.
Frequently Asked Questions
Can I get help if I have Medicare Part D?
Yes, but only after you’ve applied for and been denied Medicare’s Extra Help program. Most drug companies require proof of that denial before approving you. Income limits are strict-usually below 150% of the Federal Poverty Level. If you’re between 135% and 150% FPL, you might be stuck with no help from either program.
Do I need to be completely uninsured to qualify?
No. While many programs require you to have no insurance, others accept people with insurance if they’re underinsured-meaning your plan doesn’t cover your drug, or your out-of-pocket costs are too high. Some companies now offer special programs just for insured patients with high copays. Check the manufacturer’s website for details.
How long does it take to get approved?
It varies. Most applications take 7-14 days to process. If your doctor’s paperwork is delayed, it can take longer. Once approved, medications usually arrive within 72 hours. Some programs offer expedited approval for life-threatening conditions like cancer or severe autoimmune diseases.
Can I apply for multiple drugs at once?
Yes, but you need to apply separately for each drug and each manufacturer. A drug company only helps with their own medications. If you’re taking three different drugs from three different companies, you’ll need three separate applications. Some tools like the Medicine Assistance Tool (MAT) let you search all programs at once to make it easier.
What if I make too much money for PAPs but still can’t afford my meds?
You’re not alone. Many people fall into this gap. Try independent charities like the PAN Foundation or HealthWell Foundation-they often have higher income limits and can help with copays even if you have insurance. You can also ask your doctor about generic alternatives, patient coupons, or pharmacy discount programs like GoodRx. Some pharmacies offer 90-day supplies at lower prices.





Colin Pierce
January 27, 2026 AT 05:42I applied for Pfizer's program last year for my insulin. Got denied twice because I used gross income instead of MAGI. Third time, I grabbed my tax transcript and added my kid's SSN-got approved in 5 days. It’s a nightmare, but it works if you’re stubborn enough.
Don’t let the paperwork scare you. Just fix one thing at a time.
Mark Alan
January 27, 2026 AT 13:49USA IS THE ONLY COUNTRY WHERE YOU NEED A PHD JUST TO GET YOUR MEDS 😭💸
Drug companies are laughing all the way to the bank while we’re filling out 17 forms for a $300 pill. #MedicareForAllOrBust 🇺🇸💊
Ambrose Curtis
January 27, 2026 AT 15:39Man, I used to think these programs were just charity stuff. Then my sister got diagnosed with MS and we had to navigate this mess. Turns out, even if you make $65k, you can still qualify for some drugs if they’re expensive enough.
But holy hell, the doctor signature wait time? 3 weeks. I called the pharma rep directly-she sent me a pre-signed form. That’s how you beat the system.
Also, if you’re on Medicare and make $19k, you’re in the gap zone. No help from gov, no help from pharma. That’s not a glitch-that’s design.
Phil Davis
January 29, 2026 AT 11:03So let me get this straight. You need to be denied by a government program before a corporation will help you… and then you still have to prove you’re poor enough for them to care?
How very… American.
Anna Lou Chen
January 29, 2026 AT 22:17The entire architecture of PAPs is a neoliberal necropolitical mechanism designed to externalize the social cost of pharmaceutical monopolies onto the individual’s labor of care.
By forcing patients to become bureaucratic technicians of their own survival, capital absolves itself of responsibility while maintaining the fiction of benevolence.
It’s not assistance-it’s performative philanthropy wrapped in W-2s and MAGI calculations.
Bryan Fracchia
January 31, 2026 AT 10:06It’s brutal, but I’m glad these programs exist. I’ve seen people skip doses because they can’t afford the copay. I’ve seen people cry in pharmacy parking lots.
Yeah, the system’s broken. But if this is the only thing keeping someone alive today, then we need to fix how we talk about it-not tear it down.
Help someone fill out a form today. It matters more than you think.
Timothy Davis
February 1, 2026 AT 11:12Let’s be real-most of these people don’t even know what MAGI is. You’re telling me someone making $70k with a 401(k) and a side hustle qualifies for free drugs? Nah. This is just welfare creep disguised as compassion.
And don’t get me started on the Medicare Extra Help loophole. That’s a backdoor subsidy for middle-class retirees who should be paying full price.
Drug prices are insane, but this isn’t the fix-it’s the bandage on a hemorrhage.
fiona vaz
February 2, 2026 AT 21:40I work at a community clinic and help people apply every week. The most common mistake? Not submitting the denial letter from Medicare Extra Help. It’s not optional. It’s the key.
Also, if your doctor doesn’t sign the form, it’s trash. Call them. Email them. Text them. Beg them.
And yes-reapplying is normal. Don’t take it personally. It’s the system, not you.
Sue Latham
February 4, 2026 AT 06:03Oh sweetie, you’re applying for PAPs? How… quaint.
I mean, I know you’re trying, but have you considered just moving to Canada? Or at least getting a job with real insurance? You’re not poor-you’re just bad at budgeting.
Also, your W-2 was from 2022? Honey, that’s not proof-it’s a museum piece.
John Rose
February 5, 2026 AT 13:10Interesting data. The 63% error rate in income reporting is alarming. I’d be curious to see if there’s a correlation between education level and application success. Also, does the 27-minute average include time spent gathering documents? That’s not just form-filling-it’s full-time labor.
Lexi Karuzis
February 6, 2026 AT 10:59THIS IS A GOVERNMENT-DRUG COMPANY CONSPIRACY!!!
They WANT you to fail! They leak your info to credit agencies! The W-2 requirement? That’s how they track you! And don’t get me started on the “Medicine Assistance Tool” website-it’s a CIA front! I saw a guy in a suit watching me submit my form!
They’re putting microchips in the pills now. I know it. I’ve felt it.
CALL THE FBI. NOW.
Colin Pierce
February 7, 2026 AT 06:46Just saw your comment about the “CIA front” and had to reply. No, Lexi, the website isn’t a surveillance tool. It’s run by a nonprofit. I’ve used it. It’s free. No login. No tracking.
But if you think your meds are spying on you… maybe check your blood sugar first.
Also, I’m Colin. I got approved. Twice. You can too. Just don’t panic. Just fix one thing.