Side Effect Trade-Off Calculator
Understand Your Treatment Choices
This tool helps you understand the real trade-offs of medical treatments. Enter the benefits and side effects using actual percentages to see how they impact your life. Many patients feel more confident discussing these trade-offs with their doctors when they understand the numbers.
When you’re prescribed a new medication, your doctor might say, "This will help your blood pressure, but some people get dizzy." That’s not enough. Dizziness might sound minor-until you fall on the stairs, miss work, or stop taking the pill because you’re scared. That’s where shared decision-making comes in. It’s not about giving patients a checklist. It’s about having a real conversation where side effects aren’t just statistics-they’re lived experiences.
Why "It’s Rare" Doesn’t Cut It
Doctors often say side effects are "rare" or "common." But what does that even mean? If a drug causes nausea in "1 in 10 people," that’s 10%. That’s not rare. That’s one out of every ten people you know. And if you’re that person, it doesn’t matter how many others are fine. A 2019 study in Annals of Internal Medicine found patients understood side effect risks 37% better when numbers were given as absolute risks-like "15% chance of nausea"-instead of vague terms. Saying "this side effect affects 3-5% of users" tells you something. Saying "it’s uncommon" tells you nothing. And when patients don’t understand the real risk, they either panic or ignore the warning entirely.The SHARE Approach: A Real Conversation Framework
The Agency for Healthcare Research and Quality (AHRQ) created the SHARE Approach-a five-step model used in 47 U.S. healthcare systems. It’s not a script you memorize. It’s a structure that keeps the conversation focused on what matters to you.- Seek opportunities: Start by asking, "What’s most important to you when thinking about this treatment?" Not "Do you have any questions?" That’s passive. This opens the door.
- Help explore options: Lay out the choices clearly. For example: "We can try this statin, which lowers cholesterol but might cause muscle pain in about 1 in 10 people. Or we can try lifestyle changes first, which take longer but have no side effects."
- Assess values: This is the key. Ask: "Which side effect would be a deal-breaker for you?" For one person, it’s fatigue. For another, it’s weight gain. For someone who drives for a living, dizziness is unacceptable. You don’t know unless you ask.
- Reach a decision: Don’t push. Don’t assume. Say: "Based on what you’ve told me, it sounds like avoiding muscle pain matters more than getting the fastest drop in cholesterol. Does that sound right?" Then agree together.
- Evaluate: Follow up. "How’s the medication going? Are you noticing anything you didn’t expect?" This isn’t a one-time talk. It’s an ongoing check-in.
What Works in Real Life
A 2021 JAMA Internal Medicine study looked at chemotherapy patients. Those who had structured shared decision-making conversations were 29% less likely to quit treatment because of unexpected side effects. Why? Because they’d already talked about what they could tolerate. They weren’t blindsided. At Scripps Health, doctors who used these scripts saw a 22% drop in follow-up visits for side effect complaints. That’s not just better care-it’s less stress, fewer phone calls, and fewer trips to the clinic. One patient on Reddit shared how her doctor asked: "If you had to pick one side effect you absolutely couldn’t live with, what would it be?" She said, "I can’t handle brain fog. I’m a teacher. If I can’t think clearly, I can’t do my job." Her doctor switched her to a different medication. No guesswork. No regret.The Three-Talk Model: Clarity Over Complexity
The American Academy of Family Physicians recommends the Three-Talk Model, which breaks it down simply:- Option talk: What are the choices? Include no treatment.
- Decision talk: What matters to you? What are you willing to accept?
- Support talk: Let’s make a plan together.
When Scripts Go Wrong
Not all shared decision-making works. If a doctor reads from a script like a robot-without listening, without adjusting-it feels hollow. A 2022 study found 19% of patients felt less satisfied when scripts were used rigidly. The problem isn’t the model. It’s the delivery. A patient on HealthUnlocked said: "My doctor asked all the right questions, but never looked up from the screen. It felt like a form, not a conversation." Effective shared decision-making isn’t about checking boxes. It’s about asking: "What’s your life like? What are you afraid of? What are you willing to give up?" And then listening-really listening-to the answers.Tools That Help
Many clinics now use visual aids-color-coded charts showing side effect risks as bars or pie slices. Scripps Health found patient satisfaction jumped 41% when these were used. Seeing a 15% risk as a chunk of a circle makes it real. Numbers on paper? Often ignored. Pre-visit videos are also helping. Kaiser Permanente gave patients a 5-minute video explaining statin side effects before their appointment. The result? A 33% drop in patients stopping their medication within six months. They weren’t surprised. They were prepared.It’s Not Just for Chronic Illness
You might think this only matters for long-term meds like statins or blood thinners. But it applies everywhere. Even for antibiotics. "This will help your infection, but might give you diarrhea. Some people find that so bad they’d rather not take it. Would you be okay with that?" That’s shared decision-making. In fact, 86% of patients who stop statins do so because of side effect concerns. Not because the drug doesn’t work. Because they weren’t ready for what it might do to them.
What’s Changing Now
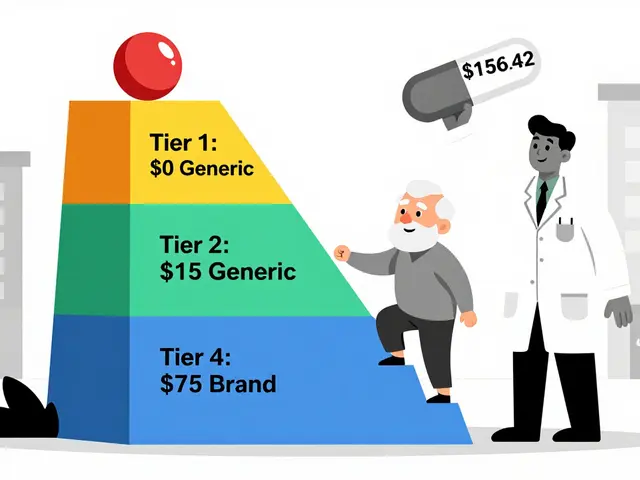
In 2023, Medicare Advantage plans were required to document shared decision-making for high-risk medications. That’s not a suggestion. It’s a rule. And it’s driving change. Hospitals are adding SDM modules into their electronic health records. Epic Systems now includes ready-made scripts for common conditions like high cholesterol, depression, and diabetes. There’s even a new CPT code-96170-that pays doctors $45 to $65 for documented shared decision-making visits. That means it’s no longer seen as "extra time." It’s seen as essential care.What You Can Do
You don’t need to wait for your doctor to bring this up. You can start it:- Before your appointment, write down: "What side effect would make me stop this treatment?"
- Ask: "Can you tell me the chance of each side effect in numbers?"
- Say: "I’m not sure what’s more important-getting better fast or avoiding this side effect. Can we talk about that?"
- After the visit: "Can I text you if I start feeling something strange?"
What’s Next
AI tools are being developed to listen to doctor-patient conversations and spot when side effect concerns aren’t being voiced. In trials, these tools flag phrases like "I’m scared to take it" or "I had a bad reaction before" that clinicians might miss. This isn’t about replacing humans. It’s about helping them hear better. The future of care isn’t just better drugs. It’s better conversations. And it starts with asking the right question: "What matters to you?"What if my doctor doesn’t use shared decision-making?
You can still start the conversation. Say: "I’ve read that it helps to talk about side effects before starting a new medication. Can we go over what to expect?" Most doctors will adjust. If they push back or seem dismissive, it’s okay to ask for a second opinion or ask to speak with a nurse or pharmacist trained in patient communication.
Are side effect trade-offs only for medications?
No. They apply to any treatment with risks and benefits-like surgery, physical therapy, mental health treatments, or even lifestyle changes. For example: "If I do this exercise program, I might feel sore for weeks. But if I don’t, my pain could get worse. Which outcome matters more to you?" The same principles of clarity, values, and choice apply.
Why do some side effects feel worse than others, even if they’re less common?
Because it’s not about statistics-it’s about your life. A 1% chance of hair loss might feel unbearable to someone who values their appearance. A 5% chance of nausea might be tolerable to someone who’s used to stomach issues. What matters isn’t the number-it’s how it impacts your daily life, identity, or routine. Shared decision-making puts your experience first.
Can I change my mind after deciding?
Yes. Shared decision-making isn’t a one-time contract. It’s an ongoing process. If a side effect shows up that you didn’t expect-or if your priorities shift-you can always revisit the decision. Your doctor should welcome that. In fact, follow-up is part of the process.
Is this only for serious conditions?
No. Even for mild conditions like acid reflux or mild depression, side effect trade-offs matter. If a pill makes you sleepy, and you’re a parent or a driver, that’s a big deal. Shared decision-making isn’t about how serious the illness is-it’s about how serious the side effect is to you.






Jerry Rodrigues
January 21, 2026 AT 18:11Been there. Took a beta blocker, got dizzy walking the dog. Thought it was just aging. Turns out it was the med. Docs say 'rare' like it's a ghost. Then you're face-planting on the porch. Just say the numbers. 1 in 10. Not 'sometimes.' That's all I need.
Amber Lane
January 22, 2026 AT 01:20My mom’s doctor never asked what she feared. She stopped her pills because she thought 'fatigue' meant 'never waking up again.' He never explained it was just tiredness. Just one question could’ve changed everything.
Ashok Sakra
January 22, 2026 AT 16:03OMG THIS IS SO TRUE I HAD A DR WHO JUST HANDED ME A PAPER AND SAID 'TAKE THIS' I ASKED ABOUT SIDE EFFECTS AND HE LAUGHED AND SAID 'YOU’LL BE FINE' I GOT SO SICK I THOUGHT I WAS DYING AND HE DIDN’T EVEN CALL BACK. THIS IS WHY PEOPLE DIE FROM MEDS THEY DON’T UNDERSTAND.
Andrew Rinaldi
January 23, 2026 AT 18:09It’s funny how we treat medical decisions like they’re math problems when they’re really about identity. What you’re willing to trade isn’t just about risk-it’s about who you are when you’re not sick. The person who fears brain fog isn’t being dramatic. They’re protecting the version of themselves that teaches, writes, laughs, drives. That’s not a side effect. That’s a core self.
And when doctors skip that part, they’re not being efficient. They’re being erasers.
Numbers help. But context is the real medicine.
Maybe the goal isn’t to reduce side effects. It’s to reduce the silence around them.
And maybe the real innovation isn’t in the drugs. It’s in the listening.
That’s the hard part. Not the science. The humanity.
And we’re still learning how to do that.
It’s not a protocol. It’s a practice.
And it starts with asking what matters-not what’s measurable.
And then actually waiting for the answer.
Not just nodding while typing.
That’s the difference between care and transaction.
Gerard Jordan
January 24, 2026 AT 09:51YES YES YES 🙌 I used to think 'rare' meant 'not me' until I was the 1 in 10 with the muscle pain. Now I ask my docs: 'What’s the worst thing that could happen? Not statistically-what’s the thing that would make me say no?' It’s changed everything. 🩺❤️
Glenda Marínez Granados
January 25, 2026 AT 04:04So let me get this straight. We’re now paying doctors $65 to stop talking like robots and actually, I don’t know, talk to people? Who knew? Next they’ll charge for eye contact. 😏
Yuri Hyuga
January 26, 2026 AT 20:58This is the future of medicine-human-centered, not system-centered. 🌍❤️ When we stop treating patients like cases and start treating them like people with lives, fears, and jobs, outcomes improve. Not just clinically-but emotionally. This isn’t soft care. It’s smart care. And it’s long overdue. Keep pushing this model. It works.
MAHENDRA MEGHWAL
January 27, 2026 AT 09:21Respectfully, the framework presented herein is both commendable and aligned with the principles of patient autonomy. However, its implementation in resource-constrained environments remains a significant challenge. The time-intensive nature of such dialogues may not be feasible within the current healthcare delivery structure, particularly in public sector institutions.
While the conceptual model is exemplary, systemic support-including reimbursement, training, and documentation infrastructure-is indispensable for scalability. Without these, it remains an ideal rather than a practice.
May this initiative inspire policy reform at the institutional level.
Kevin Narvaes
January 27, 2026 AT 23:15bro i took a pill and got the worst headache of my life and my doc said 'it's uncommon' like that makes it ok? i was in the er for 8 hours and he never even asked if i was ok. this whole thing is a scam. doctors don't care. they just want to check the box.
Philip Williams
January 28, 2026 AT 20:09Can we clarify something? The SHARE approach is evidence-based and validated across multiple studies. The fact that some clinicians implement it poorly doesn’t invalidate the model. The issue isn’t the framework-it’s the training gap. We need mandatory communication modules in med school, not optional workshops. This isn’t a nice-to-have. It’s a clinical competency.
And if you’re a patient reading this: you have the right to ask for this. No one should be prescribed a drug without knowing what they’re signing up for. Not just in numbers-but in lived terms.
Knowledge isn’t power. It’s safety.
Uju Megafu
January 29, 2026 AT 23:38Ugh. Another ‘patient empowerment’ blog post. Let me guess-you think if you just ‘ask the right questions’ you can fix a broken system? Newsflash: doctors are overworked, underpaid, and drowning in paperwork. You think they have time to play therapist? Stop blaming them. Blame the insurance companies. Blame the 15-minute visits. Blame the EHR that makes them stare at screens instead of your face. This isn’t about scripts. It’s about capitalism killing care.
And if you think telling your doctor ‘what matters to you’ is going to change anything, you’re naive. The system doesn’t care. It just wants to bill CPT 96170 and move on.