Medication Side Effect Risk Calculator
Side Effect Risk Analysis
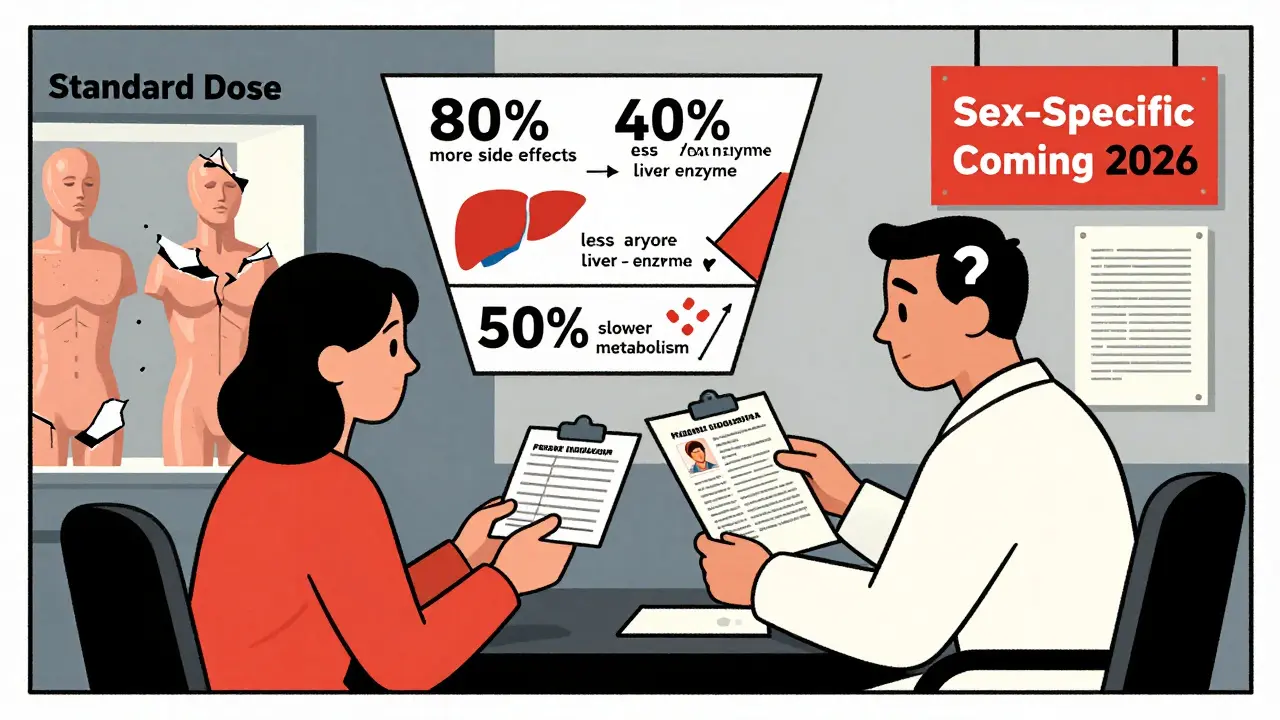
Women are nearly twice as likely as men to have a bad reaction to the same dose of a medication. It’s not just in their head. It’s in their biology, their body composition, and decades of medical research that mostly ignored them.
Why Women Get Hit Harder by Medications
From antidepressants to painkillers, women report side effects like dizziness, nausea, and extreme fatigue at much higher rates than men-even when they’re taking the exact same dose. The FDA’s own data shows women suffer adverse drug reactions 80% to 90% more often than men. And it’s not because they’re more sensitive. It’s because most drugs were tested on men, and the doses were set based on male physiology.
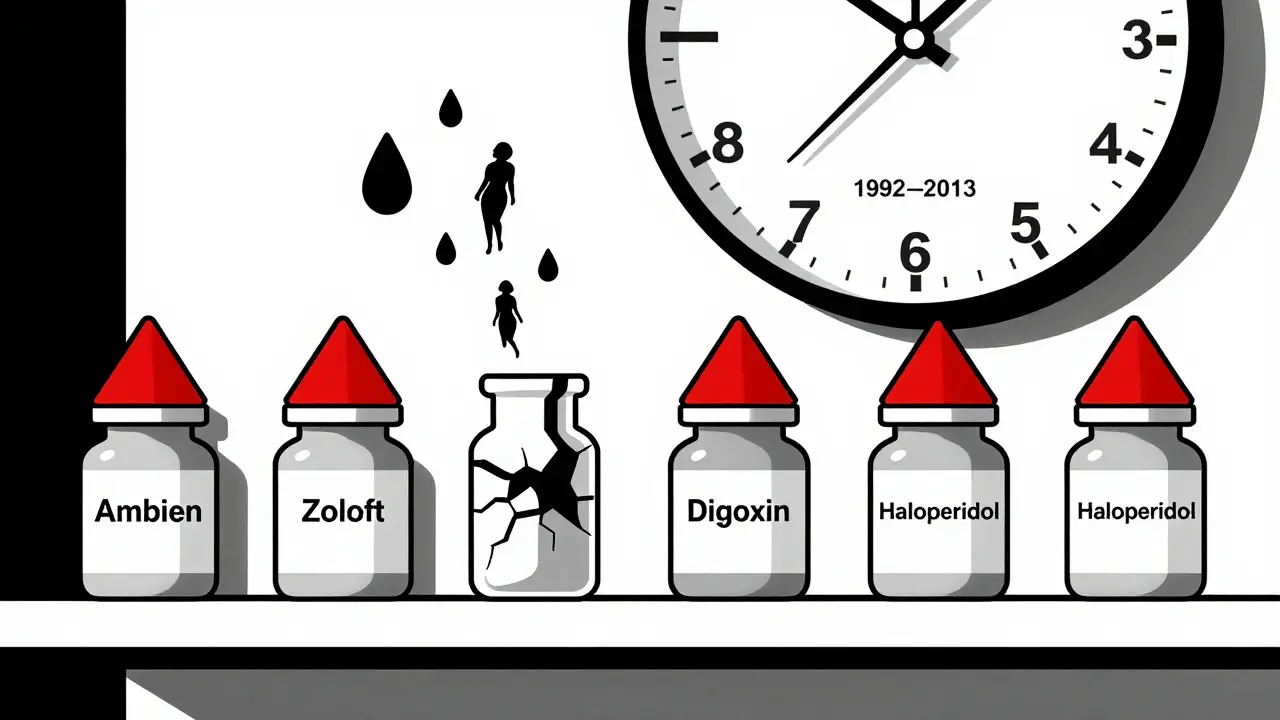
Take zolpidem, the sleeping pill sold as Ambien. In 1992, researchers noticed women stayed drowsy longer after taking the standard 10mg dose. Their bodies metabolized it 50% slower. But it took 21 years before the FDA finally cut the recommended dose for women in half. By then, thousands of women had woken up sleepwalking, driving, or even making phone calls while still asleep-all because the dose was never tested properly on them.
The Science Behind the Difference
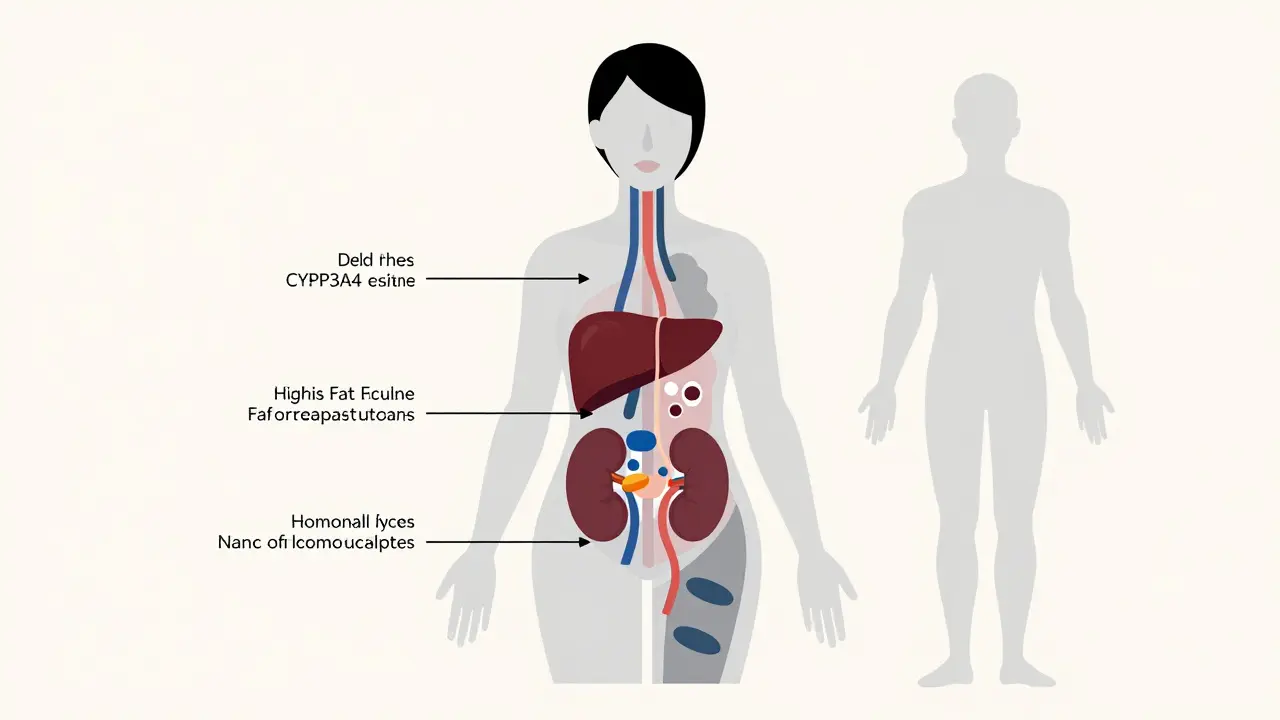
Women’s bodies process drugs differently in four key ways:
- Liver metabolism: Women have about 40% less of the enzyme CYP3A4, which breaks down half of all prescription drugs-like statins, benzodiazepines, and some antidepressants. This means drugs stick around longer, building up to toxic levels.
- Body fat and water: On average, women have 10-12% more body fat than men. Fat-soluble drugs like diazepam (Valium) get trapped in fat tissue and release slowly, prolonging their effect. Women also have less total body water, so water-soluble drugs like lithium become more concentrated in the bloodstream.
- Kidney clearance: Women clear drugs like lithium and certain antibiotics 20-25% slower than men. That’s not a small difference-it’s enough to cause toxicity if doses aren’t adjusted.
- Hormones: Estrogen and progesterone change how drugs are absorbed and broken down. Oral contraceptives can cut the effectiveness of the seizure drug lamotrigine by half. Even the phase of a woman’s menstrual cycle can shift how fast a drug is processed by up to 30%.
These aren’t theoretical. They’re measurable. A 2020 University of Chicago study found that women had 20-30% higher blood levels of digoxin, a heart medication, at standard doses. That meant their risk of dangerous heart rhythm problems jumped by 40%.
What Medications Are Most Problematic?
It’s not just sleep aids. The drug dose gender gap affects at least 86 FDA-approved medications across common categories:
- Antidepressants: Women are 1.5 to 2 times more likely to have severe nausea and dizziness on SSRIs like sertraline and fluoxetine.
- Heart drugs: Aténolol and verapamil build up to higher levels in women, increasing the risk of low blood pressure and slow heart rate.
- Anti-seizure meds: Gabapentin and carbamazepine stay in women’s systems longer, leading to more drowsiness and coordination issues.
- Painkillers: Ibuprofen and acetaminophen show different effectiveness and side effect profiles, but dosing hasn’t been adjusted.
- Antipsychotics: Women are 2.3 times more likely to develop dangerous heart rhythm changes (QT prolongation) on haloperidol.
- Antibiotics: Sulfamethoxazole causes severe skin reactions in women 47% more often than in men.
Men aren’t immune. They’re more likely to get sexual dysfunction from antidepressants and urinary retention from anticholinergics. But the scale of risk for women is far greater across more drug classes.
Why This Problem Still Exists
This isn’t new. In the 1970s, the FDA banned women of childbearing age from early drug trials to protect fetuses. It sounded protective. It was disastrous.
Even after the 1993 NIH law required women to be included in clinical trials, researchers kept analyzing results as if sex didn’t matter. A 2022 FDA review found only 12% of pharmacokinetic studies even looked at sex differences. That means 88% of drug metabolism data was based on men.
And it’s not just science-it’s culture. A 2022 AMA survey found only 28% of doctors routinely consider sex differences when prescribing. Two-thirds didn’t even know about the FDA’s 2013 zolpidem dose change for women.
Drug labels? Only 4% of FDA-approved medications have sex-specific dosing instructions. The rest? Still labeled for “adults,” meaning men.
Real Stories, Real Consequences
On Drugs.com, women taking sertraline (Zoloft) reported severe nausea 68% more often than men. On Reddit, a nurse with 12 years in the ER said she sees twice as many women coming in with bad reactions to standard pain meds.
A 2022 survey of 15,000 chronic pain patients found women were more than twice as likely to have to stop opioids because of side effects. 63% of them said they had to lower their dose or quit altogether. Men? Only 22% reported the same.
And then there’s the quiet suffering: women waking up groggy after zolpidem, feeling like they’ve been drugged all morning. A MyMedAssist.org survey found 78% of women on standard zolpidem doses reported morning grogginess. Only 32% of men did. After the FDA cut the dose, adverse event reports from women dropped by 38%.
That’s not luck. That’s proof that changing the dose saves lives.
What’s Being Done-And What’s Not
There’s progress. The FDA launched its “Sex and Gender Roadmap” in 2023, aiming to fix this by 2026. The European Medicines Agency now requires sex-stratified data in all Phase III trials. Harvard’s GenderSci Lab analyzed 33 million FDA adverse event reports and found that when you account for the fact that women take 56% more prescriptions than men, the biological sex gap in side effects shrinks to under 5%.
That’s a big deal. It suggests part of the problem isn’t just biology-it’s overprescribing. Women are more likely to see doctors, report symptoms, and get multiple prescriptions. But that doesn’t erase the biological differences. It just means we need to look at both.
Some companies are stepping up. Startups like Adyn and Womb Society are building drugs specifically for women’s bodies. But they’re tiny players in a $970 billion industry. Only 0.5% of pharmaceutical R&D is focused on sex-specific medicine.
The NIH just invested $12.5 million into a new research center at Harvard Medical School to study sex differences in medicine. The University of California’s JUST Dose study is training AI on 10,000 patient records to predict sex-specific dosing for 50 common drugs. Early results show a 40% drop in side effects when doses are adjusted.
What You Can Do
If you’re a woman taking medication:
- Ask your doctor: “Was this dose tested on women?”
- Ask: “Are there known side effects more common in women?”
- Track your symptoms. Keep a log of when side effects happen and how severe they are.
- If you’re on multiple drugs, ask about interactions that might affect women more.
- Don’t assume a higher dose means better results. Sometimes, less is safer.
If you’re a healthcare provider:
- Check the FDA’s Drug Trials Snapshots for sex-disaggregated data.
- Use the Organization for the Study of Sex Differences’ free CME courses.
- Start prescribing lower doses for women unless proven otherwise.
- Document sex-specific responses in patient records.
The system is broken, but it’s not hopeless. The Fair Trials for Women Act, introduced in March 2024, could make sex-specific dosing mandatory for all new drugs. If it passes, we could see real change by 2030.
It’s Not About Blame. It’s About Better Care.
This isn’t about saying men’s bodies are better or women’s are weaker. It’s about recognizing that human bodies aren’t one-size-fits-all. Medicine has spent 50 years treating women like small men. That’s not science. It’s negligence.
When we fix this, we don’t just help women. We improve care for everyone. Because if we learn how drugs work differently in women, we learn how drugs work differently in people. That’s the future of medicine: personalized, precise, and fair.
Why do women have more side effects from medications than men?
Women have different body composition, hormone levels, liver enzyme activity, and kidney function than men. These biological differences mean drugs are absorbed, metabolized, and cleared from their bodies at different rates. For example, women have 40% less of the liver enzyme CYP3A4, which breaks down half of all prescription drugs. This leads to higher drug concentrations and longer exposure, increasing side effect risk. Historical exclusion of women from clinical trials also means most drug doses were set based on male physiology.
Which medications are most dangerous for women?
Zolpidem (Ambien), digoxin, sertraline, haloperidol, and sulfamethoxazole are among the most problematic. Women metabolize zolpidem 50% slower, leading to next-day drowsiness and impaired driving. Digoxin builds up to toxic levels, increasing heart rhythm risks. SSRIs cause more nausea and dizziness in women. Antipsychotics like haloperidol cause QT prolongation 2.3 times more often. Antibiotics like sulfamethoxazole trigger severe skin reactions in women 47% more frequently.
Is the FDA doing anything about this?
Yes, but slowly. The FDA mandated a 50% dose reduction for zolpidem in women in 2013 after decades of evidence. Since 2018, their Drug Trials Snapshots include sex-disaggregated data for new drugs. In 2023, they launched the Sex and Gender Roadmap to integrate these considerations into all regulatory decisions by 2026. However, only 4% of drug labels currently include sex-specific dosing, and most clinical trials still don’t analyze results by sex.
Do doctors know about these differences?
Most don’t. A 2022 American Medical Association survey found only 28% of physicians routinely consider sex differences when prescribing. Two-thirds were unaware of the FDA’s 2013 zolpidem dose change for women. Medical schools rarely teach sex-based pharmacology, and drug labels rarely mention it. This knowledge gap puts women at risk every day.
What can women do to protect themselves?
Ask your doctor if the medication was tested on women and whether the dose might need adjustment. Keep a symptom log-note when side effects start and how bad they are. If you’re on multiple drugs, ask about interactions that affect women more. Don’t assume higher doses are better. If you’re having side effects, don’t ignore them-push for a lower dose or alternative. Your body isn’t wrong. The dose might be.





RAJAT KD
January 9, 2026 AT 07:30Women aren't just 'small men.' This isn't rocket science-it's basic physiology. The fact that we're still treating half the population as an afterthought in drug trials is a scandal.
Angela Stanton
January 11, 2026 AT 06:55So let me get this straight-women’s bodies are biologically different, but we’re still dosing them like men because… laziness? Budget cuts? Or just plain misogyny disguised as 'efficiency'? 🤡
Jenci Spradlin
January 12, 2026 AT 11:59My grandma took zolpidem for years and would wake up making toast at 3am. No one ever asked if the dose was right for her. She just got told to 'sleep better.'
Kiruthiga Udayakumar
January 13, 2026 AT 14:22Finally someone says it out loud. I’ve been telling my doctor for years that SSRIs make me feel like I’m drowning in syrup. He just nodded and upped the dose. 🙄
Ian Long
January 13, 2026 AT 20:04This isn’t just about gender-it’s about how medicine stopped being science and started being a one-size-fits-all industry. We’ve been treating biology like a spreadsheet. It’s not.
Maggie Noe
January 15, 2026 AT 06:16Imagine if we designed cars only for male bodies and then wondered why women got hurt more in crashes. We’d call it negligence. But with medicine? We call it 'tradition.'
Pooja Kumari
January 16, 2026 AT 03:59I’ve been on 7 different antidepressants. Every single one made me feel like my brain was wrapped in wet cotton. My doctor said, 'Just give it time.' But my body wasn’t the problem-the dose was. I cried for 3 days after reading this. Thank you.
Chris Kauwe
January 17, 2026 AT 13:07Let’s be real-this isn’t about biology. It’s about women being too emotional to be trusted with proper dosing. If they’d just stop complaining and take the pill like men do, none of this would be an issue.
Jacob Paterson
January 19, 2026 AT 11:08Oh wow, so women’s bodies are complex? Shocking. Next you’ll tell me the moon affects tides. Maybe if women stopped taking so many pills, they wouldn’t have so many side effects. Just a thought.
Patty Walters
January 19, 2026 AT 20:38My nurse practitioner actually asked me if I wanted to try lowering my sertraline dose after I mentioned the nausea. She had the FDA’s drug snapshot open on her screen. I almost cried. Someone finally listened.
Elisha Muwanga
January 19, 2026 AT 20:44This is why we need to stop letting women make medical decisions. They’re too emotional. Look at how they overreact to every side effect. Men just take the pill and move on.
Jerian Lewis
January 21, 2026 AT 13:00My wife’s heart medication dose was never adjusted. She ended up in the ER. The doctor said, 'It’s probably just anxiety.' She’s been on the same dose for 8 years. I’m done.
Drew Pearlman
January 22, 2026 AT 19:18Look, I get it. Biology is complicated. But here’s the thing-we’ve spent decades trying to make medicine universal because it’s easier. We assumed men were the baseline because they were the majority in trials. But now we know better. The real question isn’t whether we should change-it’s why it took this long. And why are we still dragging our feet? The science is here. The data is clear. The FDA has guidelines. The problem isn’t ignorance-it’s inertia. And inertia kills. Every day a woman takes a dose designed for a man’s body, we’re not just being inefficient-we’re being cruel. We don’t need more studies. We need action. We need doctors trained in sex-specific pharmacology. We need drug labels that say ‘This dose may not be safe for women.’ We need insurance to cover lower doses without extra paperwork. We need to stop treating women’s health as an add-on. It’s not a niche. It’s half the population. And if we fix this, we fix medicine for everyone. Because when you understand how a drug works in a woman’s body, you understand how it works in *all* bodies. That’s not special treatment. That’s just good science.
tali murah
January 23, 2026 AT 03:30Let’s not pretend this is about science. It’s about power. Men designed the system. Men wrote the guidelines. Men got the funding. And now we’re surprised women are dying from it? Wake up. This isn’t negligence-it’s systemic erasure.