When you're stuck in a loop of negative thoughts-worrying about what others think, replaying past mistakes, or expecting the worst-your mind isn't just being dramatic. It's caught in a pattern. And the good news? You can change it. Cognitive Behavioral Therapy, or CBT, isn't magic. It's science. More than 2,000 clinical studies back it up. It's not about digging up childhood trauma or analyzing dreams. It's about spotting how your thoughts shape your feelings and actions-and learning how to flip the script.
How CBT Works: Thoughts, Feelings, Actions
CBT is built on three simple ideas. First, distorted thinking causes emotional pain. Second, those thoughts lead to behaviors that make things worse. Third, you can learn new ways to think and act that break the cycle. It’s not about being positive. It’s about being accurate.
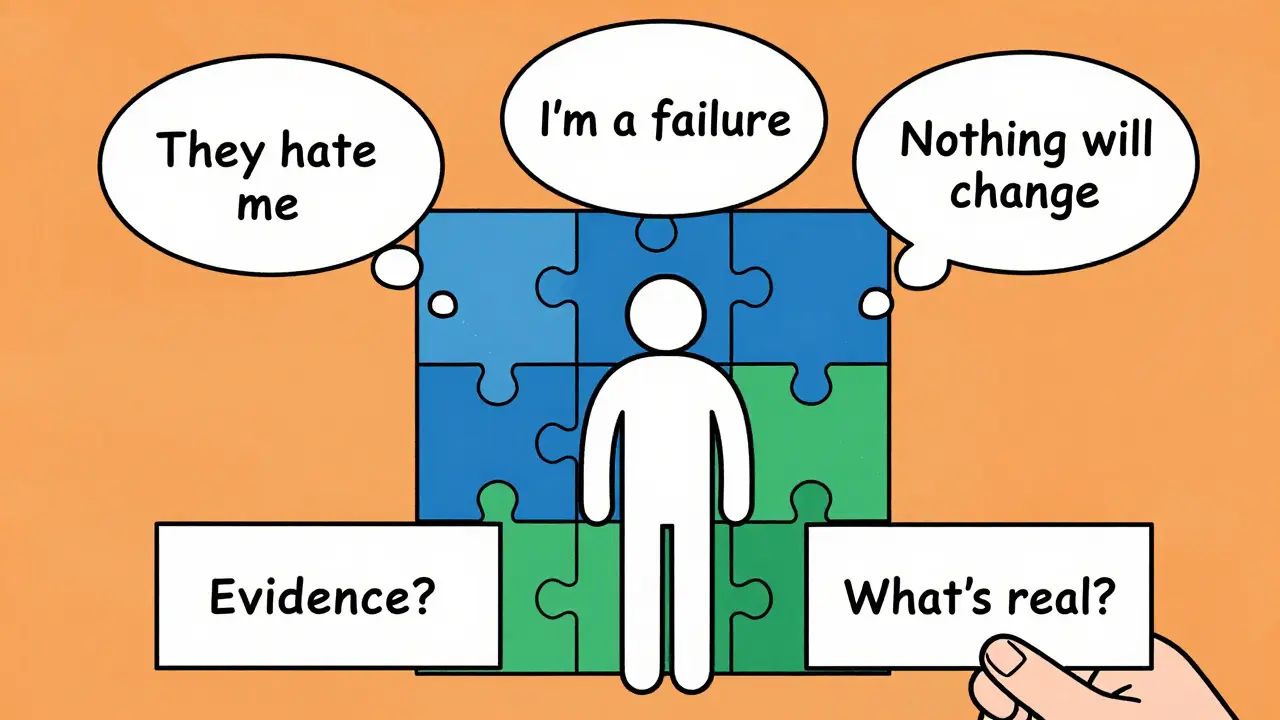
Think of it like this: You send a text to a friend and don’t get a reply. Your brain might jump to: “They hate me.” That thought triggers anxiety. You cancel plans. You isolate. The next time, you’re even more afraid to reach out. CBT helps you pause and ask: “What’s the evidence? Did they say they were busy? Did they reply to someone else?” You replace the automatic thought with something more realistic: “They’re probably just swamped.” That shift changes how you feel-and what you do next.
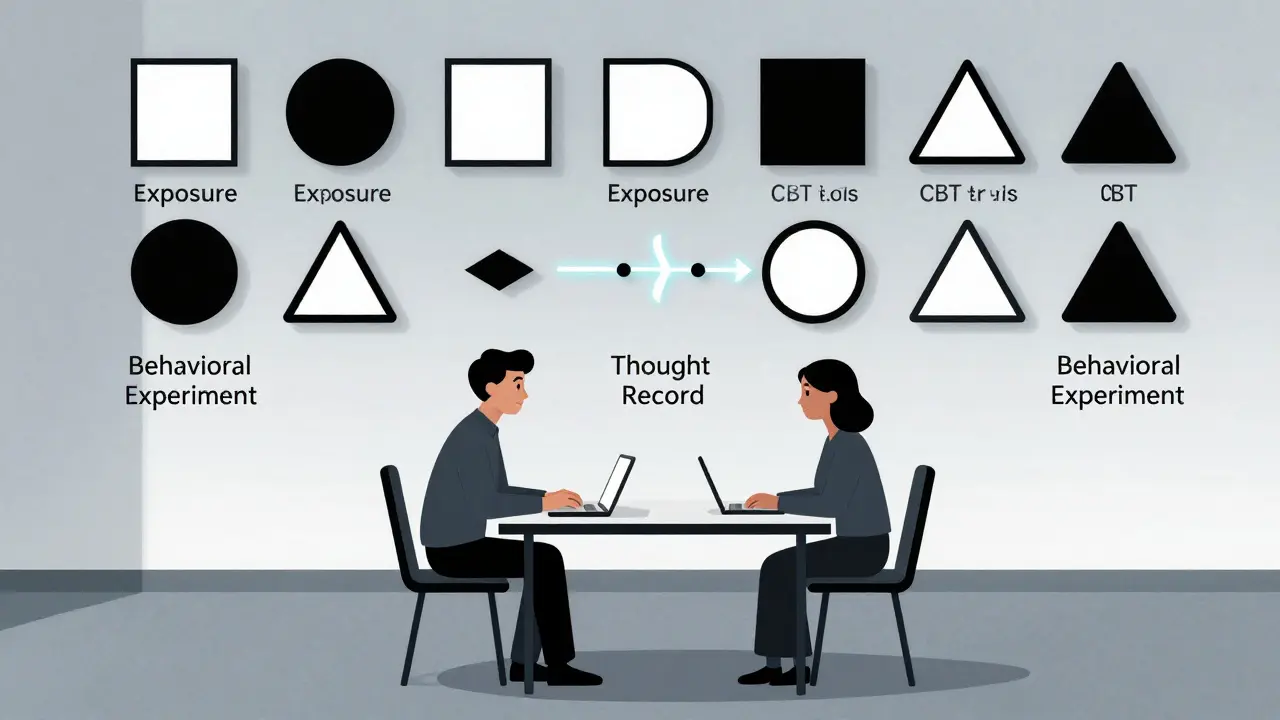
This is called the cognitive triad: negative views of yourself, the world, and the future. CBT targets each one with tools like thought records, behavioral experiments, and exposure. You don’t just talk about problems-you test them. Like a scientist, you collect data on your own mind.
What Conditions Does CBT Actually Help?
CBT isn’t a one-size-fits-all. It’s a toolkit. And it’s been proven to work for specific disorders, not vague “feeling down.” The National Institute for Health and Care Excellence (NICE) recommends it as a first-line treatment for:
- Depression
- Generalized anxiety disorder
- Panic disorder
- Social anxiety
- Obsessive-compulsive disorder (OCD)
- Post-traumatic stress disorder (PTSD)
- Eating disorders
- Insomnia
For depression, CBT works as well as antidepressants in the short term-and better in the long run. A major study in JAMA Psychiatry found that after 12 months, people who did CBT had a 24% relapse rate. Those on medication alone? 52%. That’s because CBT teaches skills you keep using after therapy ends.
For OCD, a CBT variant called Exposure and Response Prevention (ERP) is the gold standard. One case study in the Journal of Clinical Psychology followed a man with severe contamination fears. He avoided doorknobs, public restrooms, even his own home. After 18 sessions of ERP-gradually touching dirty surfaces without washing-he went from 20 compulsive hand-washes a day to zero. He returned to work. He hugged his kids again.
Even chronic pain and tinnitus respond to CBT. Not because it “fixes” the pain, but because it changes how your brain reacts to it. You stop fighting it. You stop fearing it. And that reduces the suffering.
How Long Does CBT Take? What Happens in a Session?
Most people start feeling better in 4 to 6 weeks. Full treatment usually lasts 12 to 20 sessions-once a week, 45 to 60 minutes each. That’s it. No years of weekly visits. No open-ended therapy.
Each session follows a clear structure:
- Check-in: How did your mood change since last week?
- Review homework: Did you track your thoughts? Try the exposure?
- Set an agenda: What’s the focus today?
- Work on skills: Learn a new technique or practice one you’ve started.
- Assign homework: Something you’ll do before next session.
- Summarize: What did you learn? What’s your plan?
Homework isn’t optional. It’s the core. You’ll keep a thought record: write down the situation, your automatic thought, your emotion, your behavior, and a more balanced thought. It sounds simple. But doing it daily for two weeks rewires your brain. You start noticing distortions before they take hold.
Exposure is another key tool. If you’re afraid of flying, you don’t just talk about it. You watch videos of planes. Then you go to the airport. Then you sit in a stationary plane. Then you take a short flight. Each step is planned, safe, and tracked. You learn fear doesn’t kill you-it fades.

CBT vs. Other Therapies: What’s the Real Difference?
Psychoanalysis? It’s about childhood and unconscious drives. It can take years. CBT? It’s about now. What’s happening today? What can you change today?
Medication? Antidepressants help balance brain chemicals. But they don’t teach you how to handle stress, challenge thoughts, or face fears. CBT does. And when you combine them? For severe depression, the combo works better than either alone.
Other therapies like DBT (Dialectical Behavior Therapy) are great for borderline personality disorder-better than CBT in some cases. ACT (Acceptance and Commitment Therapy) works better for chronic pain. But for most common mental health issues, CBT is still the most tested, most effective option.
A 2012 meta-analysis of 269 studies found CBT had effect sizes of 0.77 to 1.14 for anxiety disorders. Other therapies? 0.58 to 0.89. That’s a clear edge.
Who CBT Doesn’t Work For-and Why
CBT isn’t for everyone. It requires effort. You have to show up. Do the work. Think critically about your own mind. That’s hard when you’re exhausted, overwhelmed, or in acute psychosis.
People with severe cognitive impairment-like advanced dementia or untreated schizophrenia-often can’t engage with the cognitive parts. For them, other approaches are better.
Also, if you’re deeply distrustful of therapy or feel ashamed of “thinking too much,” you might resist homework. Therapists handle this with motivational interviewing: not pushing, but exploring why change feels scary.
And while CBT helps with trauma, complex PTSD with multiple losses or long-term abuse often needs longer-term, trauma-focused therapies like EMDR or somatic therapy. CBT alone might not be enough.
Real People, Real Results
On Psychology Today, 87% of 1,243 users rated CBT as “very effective” or “extremely effective” for anxiety. On Reddit, people regularly post about breakthroughs:
- “I used to have panic attacks before every meeting. After 10 sessions of CBT, I spoke up in my first team call. No shaking. No nausea. Just me.”
- “I kept thinking, ‘I’m a failure.’ My therapist had me list every time I helped someone, even small things. I had 47 entries by week 5. I stopped believing the lie.”
- “I avoided parties for 8 years. Graded exposure started with texting one friend. Then a coffee. Then a small gathering. Now I go to weddings. I didn’t know I could feel this free.”
But it’s not all easy. About a third of people say homework feels overwhelming. Some find exposure terrifying at first. That’s normal. The goal isn’t to feel comfortable. It’s to feel capable.
How to Find a Qualified CBT Therapist
Not every therapist does CBT well. Look for someone with formal training. The Beck Institute requires 120-180 hours of training, 20 supervised cases, and a certification exam. Many therapists list their credentials on their website: “Certified CBT Therapist” or “Academy of Cognitive Therapy.”
In the U.S., CBT is covered by most insurance plans under CPT codes 90832-90837. Twenty-two states include it in Medicaid. If you’re on the NHS in the UK, you can get free CBT through the IAPT program.
Free resources exist too. The National Alliance on Mental Illness (NAMI) offers downloadable CBT workbooks. Apps like Woebot (FDA-cleared in 2021) give daily CBT exercises-but they’re supplements, not replacements for human therapy.
The Future of CBT: AI, Personalization, and Digital Tools
CBT is evolving. The next wave-called “third-wave” CBT-includes mindfulness and acceptance. ACT, for example, teaches you to make room for painful thoughts instead of fighting them. It’s helping people with chronic pain and cancer-related anxiety.
AI is stepping in. Tools now analyze your thought records using natural language processing. They flag distortions like “catastrophizing” or “mind reading” in real time. The National Institute of Mental Health is testing personalized CBT based on brain scans and biomarkers. In 5 to 7 years, you might get a treatment plan tailored to your unique brain activity.
But here’s the catch: a 2024 meta-analysis in World Psychiatry found app-based CBT is 22% less effective than in-person therapy. Human connection matters. The therapist’s tone, timing, and ability to adjust on the fly can’t be replaced by an algorithm.
Still, CBT’s dominance is secure. The World Health Organization lists it in 94% of global clinical guidelines. It’s the most studied therapy ever. And it’s growing: 89% of private clinics in the U.S. offer it as a primary treatment. The market is worth over $5 billion.
Is CBT Right for You?
Ask yourself:
- Do I want to learn practical tools, not just talk about my past?
- Am I willing to do homework-even if it feels awkward at first?
- Do I want to see results in weeks, not years?
- Am I struggling with anxiety, depression, OCD, or another specific condition?
If you answered yes to most of these, CBT could be the most powerful thing you try this year. It’s not about fixing who you are. It’s about changing how you think, feel, and act-so you can live the life you already want.
Is CBT just positive thinking?
No. CBT isn’t about forcing yourself to think happy thoughts. It’s about replacing distorted, unhelpful thoughts with more accurate ones. For example, instead of thinking, “I’ll never get better,” you might learn to say, “I’m having a hard time right now, but I’ve improved before, and I have tools to help.” It’s realism, not optimism.
How long until I feel better with CBT?
Many people notice small shifts within 4 to 6 weeks. For anxiety or depression, significant improvement usually happens by session 12. It’s not instant, but it’s faster than most other therapies. The key is consistency-doing the homework between sessions.
Can I do CBT on my own?
Yes, but with limits. Self-help books, apps like Woebot, and free workbooks from NAMI can help with mild anxiety or low mood. But for moderate to severe symptoms, working with a trained therapist leads to much better results. A therapist helps you spot blind spots, stay motivated, and adjust techniques when they’re not working.
Does CBT work for kids and teens?
Yes, especially for anxiety, OCD, and depression in adolescents. For younger children, therapists adapt it using games, drawings, and stories. Parent involvement is often part of the process. Studies show CBT helps 63% of teens with anxiety-slightly lower than adults, but still highly effective.
What if I don’t like my therapist?
It’s okay to switch. The relationship matters. If you feel judged, rushed, or misunderstood, find someone else. Good CBT therapists welcome feedback. Ask: “Can we adjust how we’re working?” If not, it’s fine to move on. The goal is progress-not loyalty to one person.
Is CBT covered by insurance?
In the U.S., most private insurance plans cover CBT under psychotherapy codes (90832-90837). Medicaid in 22 states includes it. In the UK, it’s free through the NHS IAPT program. Always check your plan’s mental health benefits. Many employers offer EAPs (Employee Assistance Programs) with free sessions too.
What’s the biggest mistake people make in CBT?
Waiting to feel ready before doing the work. You don’t need to be motivated to start-you build motivation by doing. Skipping homework, avoiding exposure, or only doing the “easy” parts slows progress. CBT works when you lean into discomfort, not away from it.




Michael Burgess
January 4, 2026 AT 12:14I used to think CBT was just 'think happy thoughts' crap-until I did it. My panic attacks? Gone after 8 weeks. No meds. Just thought records and graded exposure. I started by texting one friend. Then a coffee. Then a whole damn dinner party. Now I speak up in meetings. It’s not magic. It’s math. And it works.
Also, Woebot is cute but don’t mistake it for therapy. Human connection? Non-negotiable. 😊
Wren Hamley
January 5, 2026 AT 22:32CBT’s effect size (0.77–1.14) is solid, but let’s not ignore the publication bias. Most meta-analyses are funded by CBT-aligned institutions. And what about neurodivergent folks? My autistic friend tried CBT and got worse-too much cognitive load, too little scaffolding. It’s not universal. Context matters.
Also, ERP for OCD? Gold standard. But if you’re trauma-impacted, you need somatic integration too. CBT alone can re-traumatize if not paired with safety-first approaches.
Sarah Little
January 6, 2026 AT 08:08Wait-so you’re saying CBT works better than antidepressants long-term? But what about the side effects of meds? And how do you explain the placebo effect in these studies? Also, why are they always measuring relapse rates and not quality of life? And who funds these ‘2,000 clinical studies’? Big Pharma? I’m just saying… maybe we’re missing something.
Also, I tried CBT and it made me feel worse because my therapist kept telling me to ‘challenge my thoughts’-but my thoughts were real! My boss *is* a jerk. Why should I think otherwise?
innocent massawe
January 6, 2026 AT 13:08Back home in Nigeria, people still think mental health is ‘spiritual attack’. But I showed my cousin this article-he’s now doing CBT worksheets on his phone. He said, ‘So I don’t have to be broken to fix my mind?’ That’s the shift we need. Not just meds, not just prayer. Real tools. Simple. Practical. Thank you for this.
One day, maybe we’ll have CBT in our village clinics too. 🙏
Ian Ring
January 8, 2026 AT 02:33Well-researched, well-structured. Thank you. I’ve been in therapy for 18 months-12 of those were CBT-and I can confirm: the homework is the engine. Thought records? Awkward at first. But after three weeks, I started catching distortions before they spiraled. I no longer assume silence = rejection. It’s a skill, like learning to ride a bike.
Also, I appreciate the caveat about complex PTSD. EMDR saved me where CBT stalled. Not competition-complementarity. And yes, human therapists > bots. Always. 😊
erica yabut
January 9, 2026 AT 01:35Of course CBT works-it’s just modern self-help dressed up as science. The real issue? We’ve turned emotional pain into a diagnostic category. Depression isn’t a ‘disorder’-it’s a response to a broken system. Capitalism, isolation, digital overload-those are the problems. CBT just teaches you to adapt to them. That’s not healing. That’s compliance.
And why are we still using 1960s cognitive models? We have fMRI now. We know trauma lives in the body. This is 2024. Stop pretending thought records fix systemic collapse.
Vincent Sunio
January 9, 2026 AT 23:52While the data on CBT’s efficacy is robust, the author’s reliance on anecdotal Reddit testimonials is methodologically unsound. Furthermore, the claim that CBT ‘works better than medication in the long term’ is misleading without controlling for attrition rates and therapeutic alliance variables. The JAMA Psychiatry study cited has a dropout rate of 31% in the CBT group-significantly higher than the pharmacotherapy cohort. Also, the term ‘distorted thinking’ is itself a value-laden construct, implying that non-CBT-aligned cognition is inherently pathological. This is not science. It’s epistemic hegemony.
JUNE OHM
January 10, 2026 AT 10:11CBT? Yeah, right. They’re just training you to shut up and accept the grind. Meanwhile, the real problem is the government, the media, and the corporations gaslighting us into thinking we’re broken. My therapist told me to ‘reframe my fear of layoffs’-like I should be grateful for a 9-to-5 that hates me. No. I’m not the problem. The system is. CBT is just brainwashing with a clipboard. 🤖🇺🇸
Philip Leth
January 12, 2026 AT 03:50Man, I’m from L.A. We got therapists on every corner. But I didn’t believe in CBT till my cousin told me: ‘You don’t need to be fixed. You just need to stop fighting your own mind.’
Did the thought journal. Did the exposure. Got scared. Did it again. Now I call my mom without my heart racing. No magic. Just repetition.
Also-woah, the NHS gives it free? That’s wild. We need that here. No one should have to choose between rent and a session.
And yeah, Woebot’s fun. But nothing beats a real person saying, ‘I see you.’