Opioid Dose Safety Calculator for Older Adults
Safe Dosing Calculator
Based on CDC and geriatric guidelines for patients over 65
Recommended starting dose:
Critical Safety Note
Even at correct doses, opioids increase fall risk by 28% in older adults. Monitor for:
- Unusual dizziness or confusion
- Difficulty walking or balance issues
- Excessive sedation
- Confusion or delirium (11x higher mortality risk)
Every year, tens of thousands of older adults end up in emergency rooms because of opioids-medications meant to help with pain but that often do more harm than good in people over 65. It’s not just about addiction. It’s about falls, delirium, and doses that are way too high for their bodies. These aren’t rare side effects. They’re predictable, preventable, and happening far too often.
Why Older Bodies Handle Opioids Differently
Your body changes as you age, and those changes affect how drugs work. Older adults have less muscle mass, more body fat, and kidneys and livers that don’t process drugs as quickly. That means opioids stick around longer and build up in the system. Even a dose that’s safe for a 40-year-old can be dangerous for a 75-year-old.Another big issue: the blood-brain barrier weakens with age. This protective layer that keeps toxins out becomes more porous. So more of the drug gets into the brain, leading to stronger sedation, confusion, and dizziness. It’s not that older people are ‘sensitive’-it’s that their biology has changed, and most prescriptions don’t account for that.
Studies show that older adults are twice as likely to die from opioid-related causes compared to younger people with the same condition. In one study of veterans over 50 with opioid use disorder, death rates were double those of younger veterans. And it’s not just overdoses. Many die from falls, heart attacks, or sudden confusion that leads to hospitalization.
Falls: The Silent Epidemic
Falls are the leading cause of injury-related death in people over 65. Opioids make them far more likely. How? Three main ways:- Sedation-opioids slow down the central nervous system, making reactions sluggish.
- Orthostatic hypotension-a sudden drop in blood pressure when standing up, causing dizziness or fainting.
- Impaired balance and coordination-even weak opioids like tramadol can mess with your sense of where your body is in space.
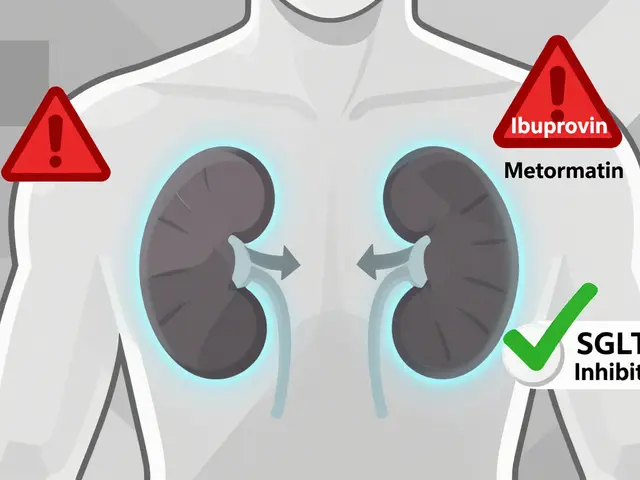
Tramadol is especially risky. It can cause hyponatremia-low sodium in the blood-which leads to confusion, nausea, and dizziness. Combine that with other medications like diuretics or antidepressants, and the risk spikes even higher. One study of 2,341 adults over 60 found that those on opioids had a 28% higher chance of breaking a bone over three years. That’s not a small risk-it’s a major red flag.
And here’s the twist: some doctors prescribe opioids to treat chronic pain because they think it will help people move better. But if the opioid causes dizziness or weakness, the person ends up falling more. Pain control doesn’t always mean fewer falls. Sometimes, it’s the opposite.
Delirium: When Opioids Fog the Mind
Delirium isn’t just ‘being confused.’ It’s a sudden, severe change in mental state-trouble focusing, hallucinations, agitation, or extreme sleepiness. It’s common in hospitals, but it’s also happening at home, often because of opioids.A landmark 2023 study tracked 75,000 Danes over 65 with dementia. Those who started opioids within two weeks of diagnosis had an elevenfold higher risk of dying than those who didn’t. That’s not a typo. Eleven times. And this wasn’t just in the hospital-it happened at home, often without anyone realizing opioids were the cause.
Delirium is often mistaken for dementia or depression. A loved one might say, ‘Grandma’s just getting forgetful,’ when in reality, she’s reacting to a new pain pill. Providers often miss it because they’re focused on pain scores, not cognitive changes. But in older adults, confusion isn’t a normal part of aging-it’s a warning sign.
And it’s not just dementia patients. Anyone over 70 taking opioids long-term has a higher chance of developing delirium. The risk is highest in the first few days after starting the drug, or after a dose increase. That’s when you need to watch closest.

Dose Adjustments: The ‘Start Low, Go Slow’ Rule
There’s no such thing as a ‘standard’ opioid dose for older adults. The rule is simple: start low, go slow.That means starting with 25% to 50% of the dose you’d give a younger adult. For example, if a typical starting dose for oxycodone is 5 mg every 6 hours, an older adult might start at 1.25 to 2.5 mg every 8 hours. And wait. Wait at least 3-5 days before increasing it. And if there’s any drowsiness, dizziness, or confusion-even mild-stop increasing and reassess.
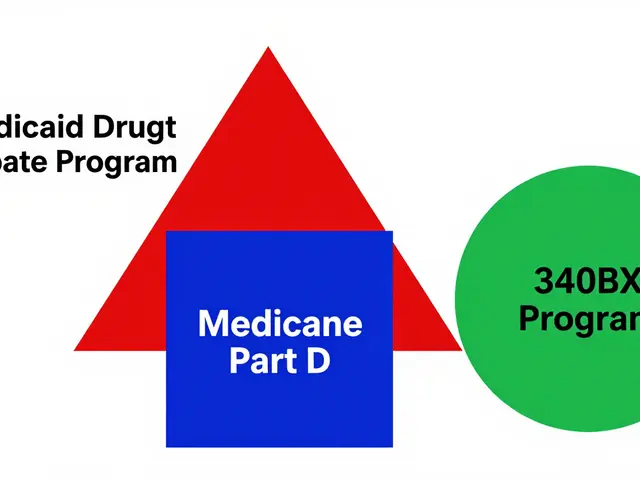
Many doctors still prescribe the same doses they’d use for a 30-year-old. That’s outdated. And dangerous. A 2022 review found that nearly 60% of older adults on opioids were prescribed doses that exceeded geriatric safety guidelines.
It’s not just about the dose-it’s about the drug. Avoid long-acting opioids like fentanyl patches or extended-release oxycodone unless absolutely necessary. They’re harder to adjust and more likely to cause buildup. Short-acting options like immediate-release hydrocodone or morphine are easier to monitor and taper.
And don’t forget drug interactions. Opioids mixed with benzodiazepines, sleep aids, antihistamines, or even some antibiotics can turn dangerous. A simple cold medicine with diphenhydramine can double sedation. Always check the full medication list-not just the pain pills.
When to Stop: Deprescribing Is Not Giving Up
Many older adults stay on opioids for years-even when they’re not helping. Why? Because stopping feels scary. Patients worry about rebound pain. Doctors worry about withdrawal. But the truth? Long-term opioid use for chronic pain often doesn’t improve function or quality of life. And the risks keep growing.Deprescribing isn’t about taking away comfort. It’s about replacing a risky solution with safer ones. The STOPPFall tool helps doctors decide when to reduce or stop opioids in people who’ve fallen or are at risk. It’s not a checklist-it’s a conversation starter.
Here’s how to approach it:
- Ask: Is the opioid still helping? Is pain down? Can they walk better? Sleep better?
- Check: Are they dizzy? Confused? Falling? Sleeping too much?
- Try reducing by 10-25% every 1-2 weeks. Monitor closely.
- Replace with non-drug options: physical therapy, heat/cold packs, acupuncture, or cognitive behavioral therapy for pain.
- Don’t stop cold turkey. Even a few weeks of opioid use can cause physical dependence. Withdrawal can include anxiety, sweating, nausea, and insomnia.
Many patients improve after tapering. Their balance gets better. Their mind clears. They sleep better. And yes-they still have pain. But it’s manageable without the danger.

What Patients and Families Need to Know
Most older adults don’t know opioids can cause falls or delirium. They think it’s just ‘a pain pill.’ They don’t realize that confusion isn’t normal aging. They don’t know that physical dependence isn’t addiction.Families should ask three simple questions:
- Why was this opioid prescribed?
- Is there a non-opioid option we could try first?
- What signs should we watch for-like dizziness, confusion, or trouble walking?
If your loved one is on opioids and has fallen, become confused, or seems ‘off,’ talk to the doctor immediately. Don’t wait for the next appointment. Bring a list of all medications, including over-the-counter ones. Ask if the dose is appropriate for their age and weight.
And remember: pain matters. But safety matters more. A person who can’t walk because of dizziness from an opioid isn’t better off than someone with moderate pain who’s stable and alert.
The Bigger Picture: Better Pain Management Is Possible
The good news? We’re starting to change. The CDC, FDA, and geriatric societies now strongly recommend avoiding opioids as first-line treatment for chronic pain in older adults. Non-drug therapies-physical therapy, tai chi, massage, nerve blocks, and even mindfulness-are proven to help with pain without the risks.And tools like STOPPFall and START/STOPP guidelines are now being used in clinics to help doctors make smarter choices. More training is happening. More awareness is growing.
But progress is slow. Too many older adults are still getting prescriptions that don’t match their needs. Too many families are unaware of the risks. Too many doctors are still using old habits.
The goal isn’t to eliminate opioids entirely. It’s to use them wisely-only when the benefit clearly outweighs the risk. And for most older adults with chronic pain, that bar is much higher than most realize.



Paul Mason
January 6, 2026 AT 19:21Look, I’ve seen this too many times-grandpa on oxycodone after a hip replacement, then he starts nodding off in the chair, trips over the rug, and cracks his skull. It’s not ‘old age,’ it’s the damn pill. Doctors act like it’s magic, but it’s just a slow poison for seniors. Start low, go slow? Yeah, if only they actually did it.
Katrina Morris
January 6, 2026 AT 21:20i read this and thought of my mom-she was on tramadol for back pain and suddenly she was seeing things at night, talking to the wall like it was her sister who passed. we thought dementia was coming… turns out it was the pill. took 3 weeks to clear her system. she’s back to herself now. no one told us this could happen. thanks for putting it out there 💙
LALITA KUDIYA
January 7, 2026 AT 13:20so true 😔 my aunt in delhi got prescribed fentanyl patch for arthritis… she got confused, stopped eating, fell three times. family blamed her age. doctor said 'she’s just old'. no one checked the meds. she died in hospital. this needs to change. 🙏
Poppy Newman
January 8, 2026 AT 20:30the blood-brain barrier thing? mind blown. 🤯 i always thought older people were just ‘more sensitive’… but no, it’s biology. like their brain’s security system got hacked by time. and we’re still giving them adult doses?? this is wild. also-why is tramadol even still on the market for seniors??
Aparna karwande
January 9, 2026 AT 21:01Western medicine is a disaster for the elderly. You give them chemicals like they’re machines, not human beings with aging organs. In India, we use turmeric, massage, yoga-natural, gentle, safe. But no, you Americans and Brits must pump them full of opioids because you’re too lazy to learn real healing. This isn’t care-it’s corporate negligence.
Vince Nairn
January 10, 2026 AT 03:04so the doctor says ‘start low, go slow’… then writes a script for 10mg oxycodone and says ‘take one every 6 hours’. yeah. that’s low. 😒 i’ve seen this. it’s not ignorance-it’s convenience. easier to prescribe than to sit down and figure out PT or gabapentin. we’ve turned pain management into a vending machine.
Kamlesh Chauhan
January 10, 2026 AT 10:19another article about old people dying from pills… i mean come on. they’re old. they’re gonna fall. they’re gonna get confused. why are we babying them? just stop giving them opioids if they can’t handle it. problem solved. also why does everyone act like this is new news? i’ve been saying this since 2015
Christine Joy Chicano
January 11, 2026 AT 06:31the 11x higher mortality rate in dementia patients on opioids? That statistic alone should trigger a national audit. This isn’t just medical error-it’s systemic malpractice. And the fact that delirium is mislabeled as ‘just dementia’? That’s linguistic negligence. Language shapes perception, and we’re normalizing death by prescription.
Adam Gainski
January 11, 2026 AT 13:28I work in geriatric care and this is spot on. We use STOPPFall every week. The hardest part? Getting families to agree to taper. They think we’re abandoning their loved one. But when we do it right-reduce the dose, add physical therapy, monitor sleep and balance-the improvement is stunning. One man went from using a walker to hiking his garden again. No opioids. Just patience and care.
Anastasia Novak
January 12, 2026 AT 03:34OMG I’m literally crying. My grandmother was on a fentanyl patch for 2 years. She stopped recognizing me. She’d stare at the ceiling and whisper to people who weren’t there. We were told it was ‘just aging’. But when we finally got her off it? She remembered my birthday. She laughed. She asked for ice cream. That’s not ‘normal’. That’s a stolen life. Why wasn’t anyone talking about this?!
Jonathan Larson
January 13, 2026 AT 10:04There is a profound ethical imperative here: to treat aging not as a disease to be medicated, but as a natural phase of human existence that demands humility in intervention. The biomedical model, in its pursuit of pain eradication, has often sacrificed cognitive integrity and physical safety. The solution lies not in abandoning opioids entirely, but in restoring agency, context, and individualized assessment to the prescribing process-guided not by protocol, but by personhood.
Alex Danner
January 15, 2026 AT 01:30the real tragedy? most of these deaths are preventable. but nobody wants to admit that pain meds are overused. it’s easier to blame the patient’s age than to admit the system’s broken. i’ve seen nurses cry after a patient dies from an opioid overdose. they knew it was too much. but they were told ‘it’s what the doctor ordered’. that’s not healthcare. that’s complicity.
Elen Pihlap
January 15, 2026 AT 16:11my dad died from this. they gave him 10mg of morphine for back pain. he was 78. he fell asleep in the shower. drowned. they said it was an accident. i know better. i’ve been screaming about this for 5 years. no one listens.