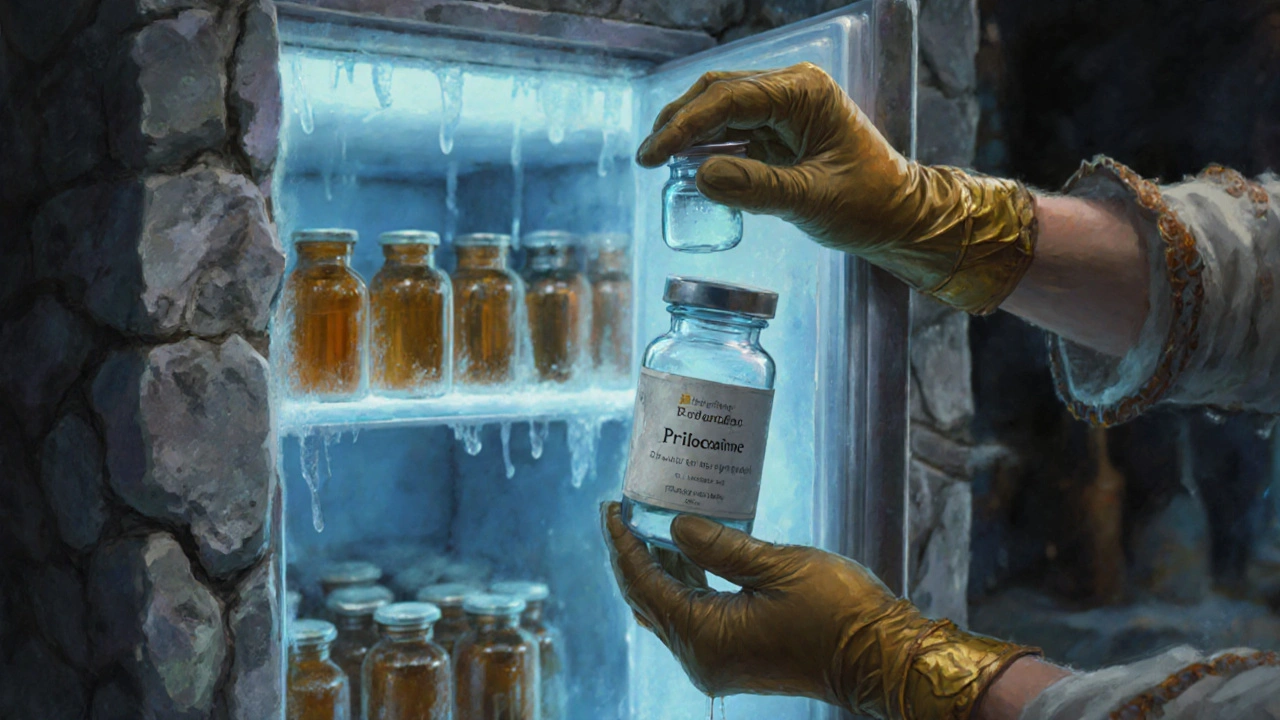
Prilocaine Temperature Compliance Calculator
This tool helps determine if your storage temperature for Prilocaine meets safety requirements and estimates potential potency loss.
When handling Prilocaine is a medium‑acting amide local anesthetic used in dentistry, dermatology and minor surgical procedures, the stakes are higher than you might think. A mix‑up in temperature or a careless throw‑away can turn a routine drug into a health hazard. This guide walks you through everything you need to know to store and dispose of prilocaine safely, whether you work in a hospital pharmacy, a dental clinic, or a field‑medicine setting.
What Is Prilocaine and Why Does It Need Special Care?
Prilocaine belongs to the amide class of local anesthetics. Compared with lidocaine, it has a slightly slower onset but causes less vasodilation, making it a favorite for procedures where bleeding control matters. Its chemical formula is C13H20N2O, and it’s supplied as a sterile solution (usually 2% or 4%) in glass vials or plastic ampoules. Because it contains a base that can hydrolyze over time, improper storage can reduce potency and, in rare cases, produce toxic degradation products such as o‑toluidine.
Key Storage Principles
prilocaine storage isn’t just about keeping the vial in a cupboard. Follow these three pillars:
- Temperature control: Keep the solution between 2°C and 8°C (36°F-46°F). A modest refrigerator works, but avoid the freezer zone where temperatures dip below 0°C. Studies from the U.S. Pharmacopeia show a 5% loss of potency for each week stored above 15°C.
- Light protection: Prilocaine is moderately light‑sensitive. Store vials in amber‑tinted containers or a dark shelf. Direct sunlight accelerates the breakdown of the anesthetic base.
- Segregation from incompatible agents: Keep it away from strong oxidizers (e.g., hydrogen peroxide) and strong acids. Cross‑contamination can trigger a hazardous reaction.
Below is a quick visual reference:
| Attribute | Prilocaine | Lidocaine |
|---|---|---|
| Recommended Temp | 2-8°C | 2-25°C |
| Light Sensitivity | Moderate - store amber | Low - clear container OK |
| Shelf Life ( unopened ) | 24months | 36months |
| Container Type | Glass vial or polypropylene ampoule | Glass ampoule or pre‑filled syringe |
Understanding Shelf‑Life and Stability
The expiration date printed on the label is not arbitrary. It reflects the date until which the manufacturer guarantees full potency and safety. Once past that date, the concentration of active drug can drop below therapeutic levels, and degradation by‑products may appear.
Key signs of a compromised vial include:
- Hazy or cloudy solution - indicates precipitation.
- Unusual odor - could signal oxidation.
- Visible particles - risk of embolism if injected.
If you notice any of these, discard the vial according to the disposal protocol outlined below.

Regulatory Landscape for Disposal
Both OSHA (Occupational Safety and Health Administration) and the EPA (Environmental Protection Agency) treat unused local anesthetic solutions as hazardous pharmaceutical waste. The CDC (Centers for Disease Control and Prevention) recommends segregation from regular trash and disposal via licensed medical waste incinerators or approved chemical neutralization services.
In Europe, the European Medicines Agency follows the same principle, mandating that member states apply the EU Directive 2001/83/EC for pharmaceutical waste.
Step‑by‑Step Disposal Process
- Label the waste: Write "UNUSED PRILOCAINE - AMIDE LOCAL ANESTHETIC" on the container. Include the batch number and expiration date.
- Containment: Place the ampoule in a puncture‑resistant sharps container if it has a needle attachment, or a sealable hazardous‑waste bag for bulk liquid.
- Segregate: Keep it separate from cytotoxic drugs, which have different incineration temperature requirements.
- Transport: Use a licensed medical waste carrier that complies with U.S. Pharmacopeia guidelines for temperature‑controlled transport.
- Final disposal: Preferred method is high‑temperature incineration (>1000°C) which destroys the active compound entirely. Alternative is chemical deactivation using a 0.5% sodium hypochlorite solution, validated by the World Health Organization for small‑scale clinics.
Document every step in the facility’s waste‑log. Audits are common, and missing paperwork can result in hefty fines.
Common Mistakes and How to Avoid Them
- Throwing vials in regular trash: This risks landfill contamination and potential needle injuries.
- Mixing with chemotherapy waste: Different combustion temperatures can release toxic gases.
- Storing at room temperature for extended periods: Potency loss leads to under‑dosage and procedural failure.
- Re‑using opened vials: Once the seal is broken, sterility is compromised.
Institute a double‑check system: one staff member verifies the storage temperature, another verifies waste labeling before disposal.

Emergency Spill Response
If a vial breaks or leaks, act quickly:
- Evacuate the immediate area and wear nitrile gloves plus eye protection.
- Absorb the liquid with an approved spill kit (e.g., absorbent pads designed for pharmaceutical chemicals).
- Place the contaminated material in a sealed hazardous‑waste container.
- Ventilate the room for at least 15 minutes.
- Report the incident to the safety officer and record it in the incident log.
Training drills twice a year keep the response sharp.
Quick Reference Checklist
- Store between 2°C‑8°C; use a dedicated medical fridge.
- Keep vials in amber or dark‑colored storage to block light.
- Check expiration dates monthly; discard any past‑date vials.
- Label waste clearly and place in a puncture‑resistant container.
- Use licensed incineration or approved chemical neutralization.
- Document every step; keep logs accessible for audits.
Frequently Asked Questions
Can I store unopened prilocaine at room temperature for a short time?
Short‑term (under 24hours) exposure to room temperature is acceptable, but you should return the vial to the refrigerator as soon as possible. Prolonged exposure (>48hours) can lower potency.
What PPE is required when handling discarded prilocaine?
Wear nitrile gloves, a lab coat, and safety goggles. If there’s a risk of aerosolisation, use a face shield and a fitted N95 respirator.
Is chemical neutralization as safe as incineration?
For small‑scale clinics, a 0.5% sodium hypochlorite solution effectively deactivates the anesthetic without generating toxic gases. However, the waste must still be collected and sent to a licensed disposal facility.
How often should I audit my storage fridge?
Quarterly temperature logs are mandatory under OSHA 1910.1030. Conduct a physical inspection at least once a month.
Can expired prilocaine be used for animal research?
No. Regulatory bodies (e.g., USDA, EU Directive) consider expired pharmaceuticals unsafe for any use, human or animal.
What do I do if a patient reacts to prilocaine?
Treat it as a local anesthetic systemic toxicity (LAST) case: stop the injection, provide airway support, administer 20% lipid emulsion IV bolus, and call emergency services.



Darryl Gates
October 16, 2025 AT 18:36Great rundown on the fridge temps – keep those vials between 2 °C and 8 °C and you’ll avoid the potency dip. A quick double‑check each shift is all it takes, and the amber containers really do the trick for light protection.
Carissa Padilha
October 17, 2025 AT 13:21The whole “store in a medical fridge” spiel feels like a cover‑up; who’s really tracking every ampoule anyway? If you think OSHA is watching, you’re missing the fact that waste logs can be faked with a simple spreadsheet. The EPA guidelines sound solid on paper, but they were written by people who never had a broken vial in a field clinic. Trust your own temperature gauge and don’t let “licensed incinerators” write your protocol. Bottom line: question every official step.
Richard O'Callaghan
October 18, 2025 AT 08:06Honestly, i think the amber bottle thing is overkill – you can just toss the vial in a regular dark drawer and it’ll be fine. just make sure it’s not too hot oR in direct sun. folks forget that you can use a regular fridge as long as you label it.
Alexis Howard
October 19, 2025 AT 02:51Sounds like a lot of hassle for a syringe.
Virginia Dominguez Gonzales
October 19, 2025 AT 21:36This guide is a lifesaver for anyone juggling a busy clinic; the way it breaks down each step feels like a backstage pass to safety. I can picture the team doing a quick temperature sweep before each patient, and the drama of a spill being handled like a Hollywood stunt – but with gloves and absorbent pads. The checklist at the end turns a mountain of regulations into a tidy script you can actually follow.
Valerie Vanderghote
October 20, 2025 AT 16:21First off, let me say that the level of detail in this guide is exactly what our department needed, because far too often we see shortcuts that end up costing the hospital both money and reputation. The emphasis on temperature control is spot on; we’ve lost a batch before when the fridge door stayed open too long, and the potency loss was measurable. Light protection may sound trivial, but I’ve witnessed a vial turn cloudy after a weekend in a sunny storage cabinet, and that’s a nightmare when you’re about to start a procedure. Segregation from oxidizers and acids is a point that can’t be stressed enough – a simple mix‑up with a peroxide bottle could create toxic by‑products you don’t want floating around. The visual table comparing prilocaine and lidocaine is incredibly helpful for quick reference, especially for new graduates who are still learning the nuances. I also appreciate the step‑by‑step disposal process; labeling the waste with batch numbers and expiration dates saves us from audit headaches later on. Using a puncture‑resistant sharps container for any ampoule that’s been accessed is a non‑negotiable safety measure, and the guide reinforces that without any ambiguity. The recommendation for high‑temperature incineration (>1000 °C) aligns with what we’ve seen in the literature as the most thorough method of destroying residual drug. For smaller clinics, the sodium hypochlorite neutralization is a practical alternative, provided the waste still gets taken to a licensed facility. The spill response section reads like a drill script – evacuate, wear PPE, absorb, ventilate, report – and that order of operations can be the difference between a minor incident and a regulatory violation. I also love that the guide reminds us to audit the fridge quarterly; the temperature logs are not just paperwork, they’re a legal shield. The FAQ at the end answers the most common doubts without forcing us to hunt through dense regulatory text. Overall, this guide turns a complex regulatory maze into a user‑friendly roadmap, and that is exactly what we need on the front lines. It also serves as a training tool for residents who need to internalize best practices early. Keep up the great work, and consider adding a quick printable poster for the lab walls.
Michael Dalrymple
October 21, 2025 AT 11:06From an ethical standpoint, ensuring the integrity of prilocaine storage safeguards not only patient outcomes but also upholds the principle of non‑maleficence. The structured approach outlined herein reflects a commitment to both scientific rigor and moral responsibility, which we, as clinicians, must embody.
Emily (Emma) Majerus
October 22, 2025 AT 05:51totes agree – keep it cold and dark, log it, and toss it right.
Miriam Rahel
October 23, 2025 AT 00:36While the guide comprehensively addresses the procedural aspects of prilocaine management, it omits a critical appraisal of the underlying pharmacokinetic variability attributable to temperature fluctuations, a factor well documented in contemporary pharmaco‑analytical studies. Future revisions would benefit from integrating quantitative data on degradation kinetics to bolster the evidentiary basis of the recommendations.
Samantha Oldrid
October 23, 2025 AT 19:21Oh sure, because a tiny spreadsheet is going to stop a hazardous waste catastrophe.
Malia Rivera
October 24, 2025 AT 14:06Honestly, all this fuss about disposal is just bureaucracy; the real Americans want quick solutions, not endless paperwork that slows down care.
lisa howard
October 25, 2025 AT 08:51When that vial shatters, the room fills with a panic that feels like a scene from a thriller, and you can hear hearts thudding as everyone scrambles for the spill kit. The dramatic gasp at the sight of amber glass glittering on the floor is real, but the training drills turn that chaos into choreography. Gloves snap, eyes widen, and the absorbent pads flutter like white flags surrendering to the spill. Everyone knows the protocol, yet in the heat of the moment the adrenaline makes you think twice about the simple steps. Once the container is sealed, the silence that follows is almost deafening – a reminder that safety isn’t just a rule, it’s a performance. The ventilation step feels like a breath of fresh air after a dramatic climax, and the final log entry is the curtain call, confirming that the act is over.
Cindy Thomas
October 26, 2025 AT 02:36Sure, chemical neutralization sounds neat, but the data show that even 0.5 % hypochlorite can leave residues that interact with other meds – just sayin’ 😒. If you really want to be safe, stick with incineration and keep the paperwork tidy.
Kate Marr
October 26, 2025 AT 21:21We’re not here to waste precious resources on extra steps – incinerate it fast, keep America’s clinics running smoothly 🇺🇸🔥.
James Falcone
October 27, 2025 AT 16:06Bottom line, follow the guide or risk a fine – nobody has time for that.