Why Generic Drug Safety Reports Are Falling Through the Cracks
More than 90% of prescriptions filled in the U.S. are for generic drugs. Yet, when something goes wrong - a patient has a severe reaction, ends up in the hospital, or suffers a life-threatening side effect - the report rarely points to the right manufacturer. This isn’t because the rules are different. They’re not. The same federal laws that require brand-name drug makers to report serious adverse events apply to generics. But in practice, the system is broken.
Here’s the reality: brand-name drug companies file about 68% of all serious adverse event reports, even though they make up less than 10% of prescriptions. Meanwhile, the companies producing the actual pills most people take - the generics - account for barely 10% of reports. That’s not a coincidence. It’s a blind spot in drug safety.
What Counts as a Serious Adverse Event?
Not every side effect is serious. The FDA defines a serious adverse event (SAE) as any reaction that:
- Results in death
- Is life-threatening
- Requires hospitalization or extends an existing hospital stay
- Causes permanent disability or significant loss of function
- Leads to birth defects
- Needs medical intervention to prevent any of the above
For example, if someone takes a generic version of simvastatin and develops rhabdomyolysis - a muscle breakdown that can cause kidney failure - that’s an SAE. If a patient on generic levothyroxine has a heart attack after a sudden spike in thyroid hormone levels, that’s an SAE too. The drug doesn’t have to be the only cause. It just has to be a likely contributor.
And here’s the key: it doesn’t matter if it’s a brand or generic. The definition is the same. But the reporting? That’s where things fall apart.
How Reporting Is Supposed to Work
The FDA’s MedWatch program is the official channel for reporting serious adverse events. Both manufacturers and healthcare providers use it. For generic drug makers, the rules are clear:
- If you learn of a serious and unexpected adverse reaction, you have 15 calendar days to report it to the FDA.
- You must keep records of every adverse event for 10 years.
- You must identify the drug by its active ingredient - not the brand name - and include the manufacturer’s name.
Reports go through MedWatch Form 3500 (paper) or its electronic equivalent. The system is designed to link the reaction to the specific product. But here’s the catch: many generic drugs have the same active ingredient - say, amlodipine - but come from 10 different manufacturers. The form doesn’t make it easy to pick the right one.
Even worse, many patients don’t know which company made their pills. Pharmacies switch suppliers without telling them. Labels are tiny. Manufacturer names are printed in 6-point font on the side of the bottle. If a doctor or pharmacist tries to report an event, they’re stuck guessing.

The Reporting Gap: Brand vs. Generic
Studies from the NIH and the FDA show the same pattern over and over. For drugs like losartan and metoprolol, when generic versions hit the market, the number of adverse event reports from the brand-name maker didn’t drop. It stayed high. Meanwhile, the generic makers barely reported anything.
Why? Three big reasons:
- Resources: Big brand companies have entire departments - pharmacovigilance teams, data analysts, compliance officers - dedicated to tracking side effects. Most generic manufacturers, especially small ones, outsource this work or handle it part-time.
- Confusion: Healthcare providers don’t know which generic manufacturer to report to. A 2020 survey found 68% of providers struggled to identify the maker of the generic drug involved in an adverse event.
- Time: Filling out a MedWatch report for a brand drug takes 15-30 minutes. For a generic? It can take 45 minutes or more because you’re digging through pill bottles, checking NDC codes, and searching DailyMed to find the right manufacturer.
The result? The FDA’s database - FAERS - is full of gaps. It looks like generics are safer than they really are. That’s dangerous. If a pattern of reactions isn’t visible, the FDA can’t act. A drug might be causing kidney damage in 1 in 5,000 patients - but if no one reports it, the signal stays buried.
What Healthcare Providers Can Do
If you’re a doctor, nurse, or pharmacist and you see a serious reaction linked to a generic drug, you’re not off the hook. You can and should report it. Here’s how to do it right:
- Check the bottle. Look for the manufacturer name on the label. It’s usually small, but it’s there.
- Find the NDC code. That 11-digit number on the label? Look it up in the DailyMed database. It will tell you exactly who made the product.
- Use MedWatch online. Go to the FDA’s MedWatch portal. Select "Healthcare Professional" as the reporter type. When asked for the drug name, enter the generic active ingredient (e.g., "amlodipine"). Then, in the manufacturer field, type the full name - not "generic" or "store brand."
- Include details. Write down when the reaction started, what symptoms occurred, and how it was treated. Even if you’re unsure if the drug caused it, report it. The FDA needs all the data.
Some hospitals now use barcode scanners at the point of dispensing. When a nurse scans the pill bottle, the system automatically logs the manufacturer and NDC code. That’s cut reporting errors by 63% in pilot programs. If your facility doesn’t have this, push for it.

What Generic Manufacturers Need to Fix
Generic drug makers can’t keep pretending this isn’t their problem. The FDA’s 2023 draft guidance says pharmacies should start printing manufacturer names on prescriptions. That’s a start. But manufacturers need to do more:
- Build reporting teams. Even small companies can hire a part-time pharmacovigilance contractor. The cost is a fraction of what brand companies spend - and it’s cheaper than a lawsuit or recall.
- Make labels clear. Print your company name in 10-point font or larger. Don’t hide it.
- Partner with pharmacies. Offer to supply pharmacies with quick-reference sheets listing your NDC codes and product names. Make it easy for them to help.
- Track your own data. Don’t wait for the FDA to find a pattern. Monitor patient feedback, pharmacy complaints, and claims data. If three patients report the same reaction in a month, investigate.
The Generic Drug User Fee Amendments (GDUFA III) just allocated $15 million to improve generic drug safety monitoring. That money is meant to help manufacturers build better systems. Use it.
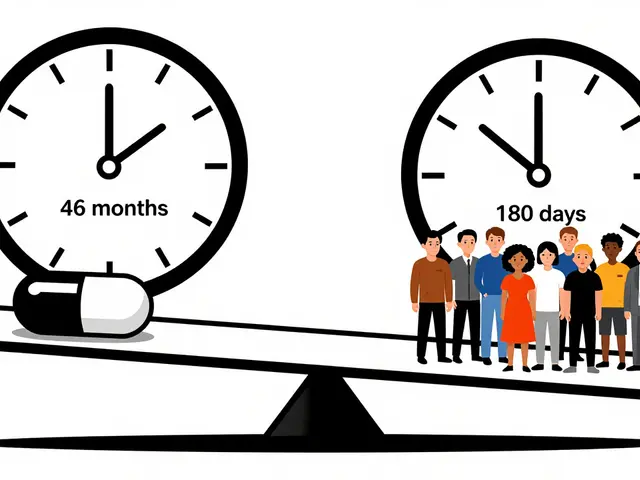
The Future: What’s Changing
The FDA is finally waking up. In 2023, they launched FAERS 2.0 - a new system that can link adverse events directly to NDC codes. That means even if a provider doesn’t know the manufacturer, the system can auto-match it.
A 2024 pilot program with CVS, Walgreens, and other major chains will automatically capture manufacturer data at the pharmacy counter. If it works, it could boost reporting accuracy by 55% within three years.
Meanwhile, the European Medicines Agency is pushing for stricter labeling rules across the EU. And the U.S. Government Accountability Office says without action, we could miss 15-20 dangerous generic drugs per year by 2030.
This isn’t about blame. It’s about safety. Generic drugs save billions of dollars every year. But if we don’t know what they’re doing to people, we’re trading cost for risk.
What You Can Do Today
Whether you’re a patient, provider, or manufacturer, here’s your action list:
- Patient: Keep your pill bottles. If you have a reaction, write down the manufacturer name before you toss the bottle.
- Provider: Don’t skip the report because it’s a hassle. One report might be the clue that saves 100 people.
- Manufacturer: Set up a simple reporting system. Even if you only have one person handling it, make sure it’s done.
Drug safety isn’t a luxury. It’s a requirement. And for generics, it’s long overdue.



Jodi Olson
January 31, 2026 AT 05:10So the system is designed to fail because nobody wants to trace a 6-point font on a pill bottle. This isn't a bug. It's a feature for companies that don't care if you die as long as the profit margin stays high.
Eliana Botelho
February 1, 2026 AT 13:00I’ve had three different generic versions of my blood pressure med and each one gave me a different side effect. One made me dizzy, one made me nauseous, one made me feel like I was underwater. I reported all of them. Nobody cared. The pharmacist just shrugged and said, 'It’s the same chemical.' No. It’s not. The fillers, the coatings, the manufacturing environment - it’s all different. But the FDA doesn’t track that. They track the active ingredient and call it a day. That’s why people keep dying. They’re treating pills like cereal boxes.
Melissa Cogswell
February 3, 2026 AT 05:54Just wanted to say I’ve been reporting every odd reaction I see in my clinic. Took me 20 minutes the first time. Now it’s under 5. The MedWatch portal is way better than people say. Just don’t skip the manufacturer field. I’ve seen so many reports that just say 'generic amlodipine' - useless.
Sazzy De
February 4, 2026 AT 08:54My mom had a reaction to a generic metformin last year. We didn’t know who made it until I dug through the receipt and found the NDC code. Took me an hour. I reported it. Never heard back. I’m not surprised. The system is broken but nobody’s got the energy to fix it.
kate jones
February 4, 2026 AT 12:47FAERS 2.0 linking to NDC codes is a game-changer. The current system relies on human error - and pharmacists are overworked. If the barcode at the point of sale auto-populates the manufacturer, that’s 80% of the problem solved. The rest is just enforcement. FDA needs to mandate NDC visibility on labels and penalize non-compliance. No more 6-point font.
Rohit Kumar
February 4, 2026 AT 22:11In India, we don’t even have this problem. Every generic bottle has the manufacturer name in bold, 12-point font. The government requires it. No excuses. Why can’t the U.S. do the same? It’s not about money. It’s about will. You let corporations hide behind anonymity while patients suffer. That’s not capitalism. That’s negligence dressed up as free market.
Diana Dougan
February 5, 2026 AT 03:21Oh wow so the problem is… the people who make the pills don’t wanna do paperwork? Shocking. Next you’ll tell me water is wet. I’m sure the generic makers are just sitting around crying because they can’t afford a 15-minute report. Maybe they should’ve thought of that before they started selling drugs to people who can’t afford brand names. 😏
Donna Fleetwood
February 6, 2026 AT 10:11My nurse practitioner started scanning pill bottles last month. Now she knows exactly who made every drug. I’ve never seen her so confident. One report led to a recall of a bad batch of levothyroxine. We saved three people. It’s not glamorous. But it matters. Keep reporting. Even if it feels like shouting into the void - someone’s listening.
Lily Steele
February 7, 2026 AT 14:03I used to skip reporting because it felt pointless. Then I found out a guy in my town died from a generic statin reaction - and it was never reported. I filled out the form that week. It took me 37 minutes. I didn’t feel like a hero. I felt like I had to do it. That’s the sad part.
Gaurav Meena
February 8, 2026 AT 19:16As someone who works in pharma logistics in India, I can say this: clear labeling isn’t expensive. It’s a cultural priority. We don’t hide our makers. We’re proud of them. In the U.S., you treat generics like disposable items. But they’re not. They’re life-saving. Treat them like it. And yes, I’ve seen the FDA’s new NDC system - it’s brilliant. Just make it mandatory. No more loopholes.
KATHRYN JOHNSON
February 9, 2026 AT 07:43The FDA's inaction is indefensible. This is not a technical issue. It is a moral failure. Manufacturers are violating their fiduciary duty to public health. The fact that this has persisted for over a decade is evidence of systemic corruption. Regulatory capture is real. And it is killing people.
Marc Bains
February 10, 2026 AT 22:17Let me tell you what’s really going on. The brand companies report because they’re scared of lawsuits. The generics? They’re scared of losing their 3-cent profit margin. So they play the game: report only when forced. But here’s the thing - if every provider reported correctly, the data would explode. And then the FDA would have to act. So don’t wait for them. Report anyway. One report might be the one that flips the switch.
Beth Beltway
February 12, 2026 AT 03:11Oh please. You think the FDA is going to fix this? They’re the same agency that approved OxyContin. They’re not here to protect you. They’re here to protect the industry. You report your reaction? Congrats. You’re now a data point in a spreadsheet that’ll be buried under 12 million others. Wake up. This system is designed to silence you.
Shubham Dixit
February 12, 2026 AT 15:16India produces 40% of the world’s generic drugs. We have over 20,000 manufacturers. And not once have we had a systemic failure like this. Why? Because we have mandatory labeling laws. Because we have national databases that auto-identify NDC codes. Because we don’t treat patients like afterthoughts. The U.S. has the technology. It has the money. But it lacks the will. This isn’t about drugs. It’s about values. And right now, the U.S. values profit over people. That’s not innovation. That’s decay.
April Allen
February 14, 2026 AT 03:33Pharmacovigilance for generics is underfunded because it’s seen as low-margin, low-risk. But risk isn’t measured by price - it’s measured by volume. With 90% of prescriptions being generic, even a 0.01% adverse reaction rate translates to 30,000 events annually. That’s not noise. That’s a signal. And the current MedWatch system is statistically underpowered to detect it. We need AI-driven signal detection, automated NDC mapping, and mandatory manufacturer liability. Until then, we’re just guessing.