Sleep & Depression Alternative Comparison Tool
Find Your Best Alternative
Answer a few questions to get personalized recommendations based on your needs
Best Options For You
Important Considerations
- Never stop trazodone suddenly - Always taper under medical supervision
- Medication works best when combined with sleep hygiene habits
- CBT-I offers the most sustainable long-term solution for insomnia
If you’re taking Desyrel (trazodone) for sleep or depression and wondering if there’s a better fit, you’re not alone. Thousands of people in the UK and beyond switch off trazodone each year-not because it doesn’t work, but because the side effects, timing, or long-term results don’t match their needs. The truth? Trazodone isn’t the only option. Some alternatives work faster. Others cause less grogginess. A few don’t carry the same risk of dizziness or low blood pressure. Let’s cut through the noise and compare what’s actually out there, based on real patient experiences and clinical data from 2025.
What Desyrel (Trazodone) Actually Does
Desyrel is the brand name for trazodone, a medication originally developed in the 1960s as an antidepressant. It works by increasing serotonin in the brain, but unlike SSRIs like sertraline or fluoxetine, it also blocks certain receptors that affect sleep. That’s why it’s commonly prescribed off-label for insomnia-even though it’s not FDA-approved for that use in the US, and not officially licensed for sleep in the UK.
Most people take 25-100 mg at night for sleep. At that dose, it’s not strong enough to treat depression, but it’s enough to make you drowsy. Around 60% of users report improved sleep in the first week. But here’s the catch: about 40% say they wake up feeling foggy, dry-mouthed, or dizzy the next morning. Some report headaches, nausea, or even rare cases of priapism (a prolonged, painful erection). These side effects are why many look for alternatives.
Alternative 1: Doxepin (Silenor)
Doxepin is an older tricyclic antidepressant, but at low doses (3-6 mg), it’s FDA-approved specifically for sleep maintenance insomnia. Unlike trazodone, it doesn’t cause next-day grogginess in most people. A 2024 study in the Journal of Clinical Sleep Medicine found that 72% of users on 6 mg of doxepin stayed asleep longer than those on placebo, with no significant morning impairment.
It’s not a first-line choice for depression because it’s too sedating at higher doses. But for sleep alone? It’s cleaner than trazodone. The downside? It’s not always covered by the NHS in the UK, and prescriptions are less common. You might need to pay out of pocket-around £35 for a 30-day supply.
Alternative 2: Mirtazapine (Remeron)
If you’re taking trazodone for both depression and sleep, mirtazapine might be a more natural fit. It’s an antidepressant that also strongly promotes sleep, especially at lower doses (7.5-15 mg). Unlike trazodone, mirtazapine doesn’t cause dizziness or low blood pressure as often. Instead, it can increase appetite and cause weight gain-which is a problem for some, but a benefit for others who’ve lost weight due to depression.
One big advantage: it kicks in faster for sleep than most SSRIs. People report feeling sleepy within 30-60 minutes. A 2023 trial comparing mirtazapine 15 mg to trazodone 50 mg found similar sleep quality, but fewer reports of morning hangover with mirtazapine. It’s available on the NHS, and generic versions are cheap. But if you’re trying to avoid weight gain, this isn’t the pick.
Alternative 3: Trazodone vs. Melatonin (Extended-Release)
Melatonin isn’t a drug-it’s a hormone your body makes naturally to signal bedtime. But synthetic, extended-release melatonin (like Circadin) is licensed in the UK for people over 55 with primary insomnia. It doesn’t cause dependency, withdrawal, or next-day fog. It’s not strong enough for severe sleep onset issues, but if your problem is waking up at 3 a.m. and not falling back asleep, it’s often more effective than trazodone.
A 2025 meta-analysis from the Cochrane Collaboration showed that extended-release melatonin improved total sleep time by an average of 13 minutes and reduced wake time after sleep onset by 17 minutes. That’s modest, but for someone who’s sensitive to medications, it’s a safer bet. You can buy it over the counter in the UK, but the licensed version (Circadin) requires a prescription. Many people start here before trying stronger meds.
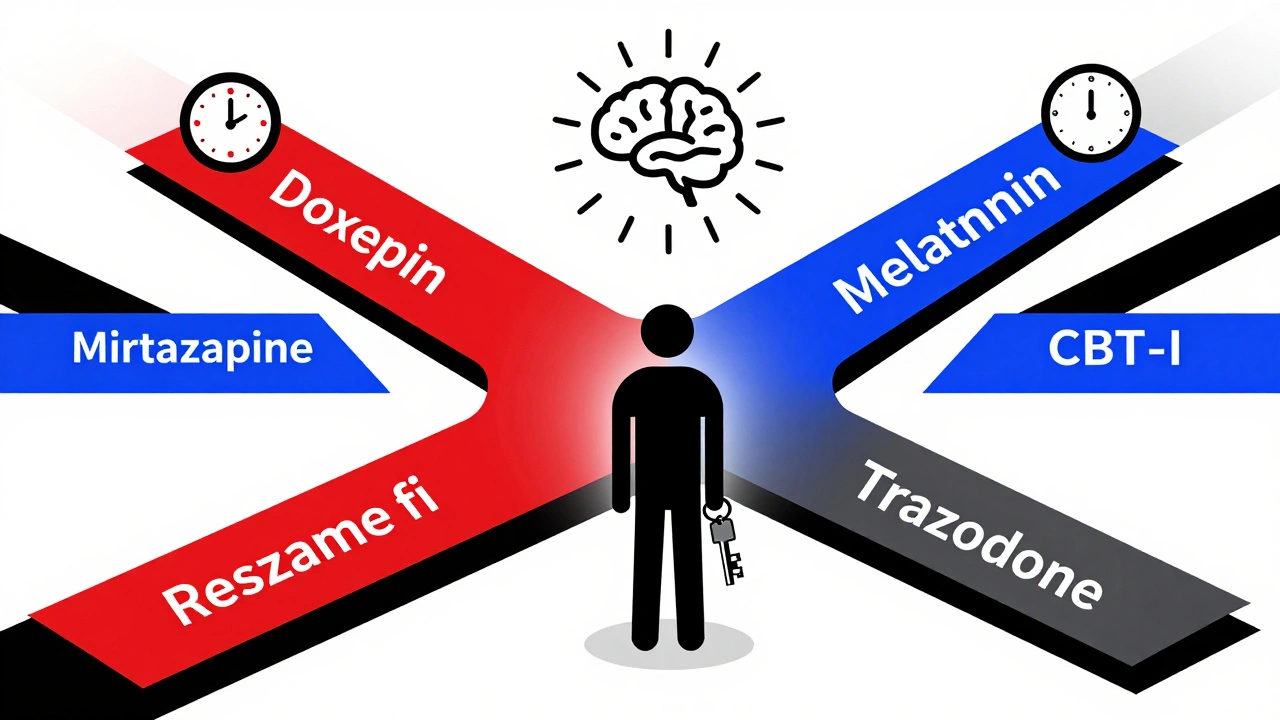
Alternative 4: Cognitive Behavioral Therapy for Insomnia (CBT-I)
If you’ve tried trazodone and it didn’t stick, or if you’re tired of taking a pill every night, CBT-I might be the most powerful alternative you haven’t considered. It’s not a drug. It’s a structured, 6-8 week program that teaches you how to retrain your brain to sleep. Studies show it works better than any sleep medication-including trazodone-over the long term.
Unlike meds, CBT-I doesn’t wear off. You don’t need to keep taking it. A 2024 NHS pilot in Northern Ireland tracked 300 patients with chronic insomnia. After CBT-I, 78% stopped using sleep aids entirely within six months. The program includes sleep restriction, stimulus control, and cognitive restructuring. It’s available through the NHS, often via your GP referral. Some private therapists offer it too. It takes effort, but the results last.
Alternative 5: SSRIs and SNRIs (Sertraline, Escitalopram, Venlafaxine)
Many people take trazodone because they’re also depressed. But if your main issue is depression with secondary insomnia, you might be better off treating the depression directly. SSRIs like sertraline or escitalopram, or SNRIs like venlafaxine, can improve both mood and sleep over time.
The catch? These drugs often make insomnia worse in the first 2-4 weeks. That’s why doctors sometimes pair them with trazodone short-term. But if you’re stable on an SSRI and still struggling to sleep, switching to mirtazapine or adding melatonin might be smarter than staying on trazodone long-term. A 2023 study in The Lancet Psychiatry found that patients on escitalopram alone had better sleep quality after 12 weeks than those on escitalopram + trazodone.
When Not to Switch
Not everyone should stop trazodone. If you’ve been on it for over a year and it’s working-no grogginess, no side effects, you’re sleeping 7 hours a night-then don’t fix what isn’t broken. Also, if you’ve tried other sleep aids and they caused anxiety, heart palpitations, or worsened your depression, trazodone might be your safest bet.
And if you’re on it for chronic pain or anxiety disorders like PTSD, trazodone’s mild calming effect might be exactly what you need. Some patients with fibromyalgia or severe nighttime anxiety report better results with trazodone than with gabapentin or benzodiazepines.
What to Ask Your Doctor
Before switching, have this conversation:
- Is my insomnia primary, or linked to depression/anxiety?
- Am I taking trazodone for sleep, or for mood?
- Have I tried non-drug options like CBT-I or sleep hygiene?
- What are the risks of long-term use for me?
- Is there a cheaper, safer, or more effective option based on my age, weight, or other meds?
Don’t stop trazodone cold turkey. It can cause rebound insomnia or even mild withdrawal symptoms like nausea or irritability. Always taper under medical supervision.
Quick Comparison: Trazodone vs. Top Alternatives
| Medication | Best For | Onset of Sleep | Next-Day Drowsiness | Dependence Risk | NHS Availability |
|---|---|---|---|---|---|
| Trazodone | Mild depression + sleep | 30-60 mins | Common | Low | Yes |
| Doxepin (3-6 mg) | Staying asleep | 45-90 mins | Low | Very low | Yes (special request) |
| Mirtazapine (7.5-15 mg) | Depression + sleep + poor appetite | 20-40 mins | Mild | Low | Yes |
| Extended-Release Melatonin | Older adults, circadian rhythm | 60-90 mins | None | None | Yes (Circadin) |
| CBT-I | Long-term solution | Weeks | None | None | Yes (referral needed) |
What Most People Miss
The biggest mistake? Treating sleep as a standalone problem. If you’re taking trazodone for sleep but still scrolling on your phone until 1 a.m., drinking caffeine after 3 p.m., or sleeping in on weekends, no pill will fix that. Medication works best when paired with habits.
One patient in Belfast, 62, stopped trazodone after 18 months. She switched to melatonin and started a 10-minute wind-down routine: no screens after 9 p.m., dim lights, herbal tea, and reading a physical book. Within three weeks, she was sleeping through the night. She didn’t need anything stronger.
Another, a 45-year-old nurse with anxiety, tried CBT-I after three failed attempts with trazodone. She learned to stop lying in bed worrying. Now, she only goes to bed when sleepy. Her sleep quality improved more than it ever did on meds.
Medication is a tool. Not a cure. And sometimes, the best alternative isn’t another pill-it’s a change in how you live.
Is trazodone addictive?
Trazodone isn’t considered addictive in the way benzodiazepines or sleeping pills like zolpidem are. You won’t crave it or need higher doses to get the same effect. But your body can get used to it, and stopping suddenly can cause rebound insomnia or mild withdrawal symptoms like nausea or anxiety. Always taper off under a doctor’s guidance.
Can I take trazodone with other antidepressants?
Yes, but only under close supervision. Combining trazodone with SSRIs or SNRIs increases the risk of serotonin syndrome-a rare but serious condition. Symptoms include agitation, rapid heartbeat, sweating, and confusion. Your doctor will monitor you if you’re on both. Never mix them without medical advice.
Which alternative is best for older adults?
For people over 65, extended-release melatonin (Circadin) is often the first choice. It’s safer than trazodone, which can increase fall risk due to dizziness. Mirtazapine is also used, but its weight gain effect can be problematic in frail older adults. Avoid benzodiazepines entirely-they’re linked to memory loss and increased dementia risk in this age group.
How long does it take for alternatives to work?
Melatonin and doxepin usually help within a few days. Mirtazapine can take 1-2 weeks for sleep to improve. SSRIs may make sleep worse at first, then better after 3-4 weeks. CBT-I takes 6-8 weeks to show full results, but those results last years after stopping.
Is trazodone safe for long-term use?
There’s no strong evidence that trazodone causes organ damage with long-term use. But prolonged use increases the risk of tolerance-meaning you might need higher doses over time. It also raises the chance of daytime drowsiness, low blood pressure, and falls in older adults. For chronic insomnia, CBT-I is the preferred long-term solution according to NICE guidelines.
Next Steps
If you’re considering switching from trazodone:
- Track your sleep for two weeks with a simple journal-note bedtime, wake time, and how rested you feel.
- Ask your GP about CBT-I. It’s free on the NHS and often the most effective long-term fix.
- If you want a replacement pill, ask about doxepin or mirtazapine, depending on whether your main issue is staying asleep or mood.
- Try extended-release melatonin if you’re over 55 or sensitive to meds.
- Never stop trazodone suddenly. Work with your doctor to taper safely.
There’s no one-size-fits-all solution. But there is a better fit for you-if you’re willing to look beyond the pill bottle.





Sean McCarthy
December 2, 2025 AT 19:00Trazodone makes me feel like a zombie by 10am. Doxepin was a game changer. No fog. Just sleep. No drama.
soorya Raju
December 4, 2025 AT 10:59lol the pharma giants dont want you to know melatonin is just a hormone your body makes… they sell you trazodone for $80 a month because its patented. the real cure? stop staring at screens after 8pm. they dont want you to know that either. #BigSleep
Kshitij Shah
December 6, 2025 AT 07:51So you're telling me the NHS gives you a pill to fix a habit problem? Classic. I tried CBT-I after my third failed trazodone run. Now I read actual books before bed. No meds. No guilt. Just me, a lamp, and my cat judging me for staying up too late.
Linda Migdal
December 7, 2025 AT 11:46CBT-I is the only real solution. Everything else is just chemical band-aids. America needs to stop treating sleep like a broken machine you can fix with a part. This isn't Germany. We don't need more pills. We need discipline.
Tommy Walton
December 8, 2025 AT 11:57Existential question: if you sleep on a pill, are you really resting… or just chemically surrendering to entropy? 🤔
Also, melatonin > trazodone. The body knows what it's doing. We just forgot how to listen.
James Steele
December 9, 2025 AT 15:15The pharmacokinetic profile of trazodone is suboptimal for chronic insomnia due to its 5-HT2A antagonism with concomitant alpha-1 adrenergic blockade - hence the orthostatic hypotension and next-day sedation. Doxepin’s selective H1 antagonism at low doses offers superior temporal specificity. CBT-I remains the gold standard per NICE 2024 guidelines.
Louise Girvan
December 10, 2025 AT 07:41They’re all lies. The FDA knows trazodone causes brain fog because they tested it on veterans. The VA hides it. Melatonin? They say it’s ‘natural’ so they can’t patent it. That’s why it’s not pushed. Wake up.
Dennis Jesuyon Balogun
December 11, 2025 AT 16:07Let me say this plainly: you don’t treat sleep with chemicals if you’re ignoring the rhythm of your life. I’ve seen men in Lagos work 16-hour days, sleep 4 hours, and still thrive - not because of pills, but because they learned to honor their body’s clock. Trazodone is a crutch. CBT-I is a compass.
Grant Hurley
December 12, 2025 AT 09:14just tried melatonin after reading this and holy crap i slept like a rock. no grogginess. no weird dreams. just… peace. also i stopped scrolling at 10pm and now i feel like a new person. thanks for the nudge guys 🙌
Lucinda Bresnehan
December 12, 2025 AT 23:44For anyone over 50: try Circadin. I was on trazodone for 3 years - woke up dizzy, forgot my keys, felt like I was underwater. Switched to melatonin ER. Within a week, I was falling asleep faster and actually waking up refreshed. My doctor was skeptical… until I showed him my sleep log. It’s not magic. It’s biology.
Shannon Gabrielle
December 13, 2025 AT 18:31Of course the article says CBT-I works - it’s free. Pharma doesn’t make money off it. Meanwhile, they’re selling trazodone like it’s bottled magic. Wake up. You’re being played.
ANN JACOBS
December 14, 2025 AT 17:42It is my profound belief, grounded in both empirical observation and compassionate clinical experience, that the modern paradigm of pharmacological intervention for sleep disturbances represents a fundamental misalignment with the holistic nature of human physiology. The human organism, when provided with environmental harmony, circadian alignment, and psychological safety, possesses an innate capacity for restorative slumber - a capacity that is, in contemporary society, systematically eroded by artificial light, chronic stress, and the commodification of sleep as a pharmacological problem. I encourage each individual to consider, with the utmost seriousness, the possibility that the solution does not reside in the pill bottle, but rather in the quiet, disciplined reclamation of one’s natural rhythm - a journey not of chemical substitution, but of existential recalibration.