For many women, menopause isn’t just about hot flashes and sleepless nights. It’s a shift that affects mood, energy, bones, heart health, and even how you feel about your own body. Hormone Replacement Therapy (HRT) has been around since the 1940s, but for decades, the conversation around it was muddled by fear. Then came the 2002 Women’s Health Initiative study-and everything changed. Now, in 2026, we know more than ever: HRT isn’t a one-size-fits-all drug. It’s a tool. And when used right, it can be life-changing.
What HRT Actually Does
HRT replaces the estrogen (and sometimes progesterone) your body stops making after menopause. That’s it. No magic. No miracle cure. Just science. Estrogen drops cause hot flashes, night sweats, vaginal dryness, brain fog, and bone thinning. HRT brings levels back up to where they were in your 30s and 40s-not higher, not lower. Just enough to ease the symptoms.
There are two main types: estrogen-only (ET) for women who’ve had a hysterectomy, and estrogen-plus-progestogen (EPT) for those with a uterus. Why the progesterone? Because estrogen alone can cause the lining of the uterus to thicken, which raises the risk of endometrial cancer. Progesterone prevents that. It’s not optional-it’s safety.
Benefits: More Than Just Hot Flash Relief
If you’re struggling with hot flashes, HRT works better than anything else. Studies show it reduces hot flashes by 80-90%. SSRIs and other non-hormonal options? They help about half as much. That’s not a small difference. It’s the difference between getting through your day and dreading it.
But it’s not just about comfort. HRT cuts your risk of osteoporotic fractures by 34%. That’s huge. After 60, a hip fracture can change your life forever. HRT helps keep your bones strong. It also improves skin elasticity, reduces vaginal atrophy, and may help with mood swings and sleep quality.
Here’s the real game-changer: if you start HRT before age 60 or within 10 years of your last period, it can lower your risk of heart disease by 32%. That’s not a guess. It’s from the Women’s Health Initiative and confirmed by the North American Menopause Society. The key word? Timing. Starting late? No benefit. Starting early? Real protection.
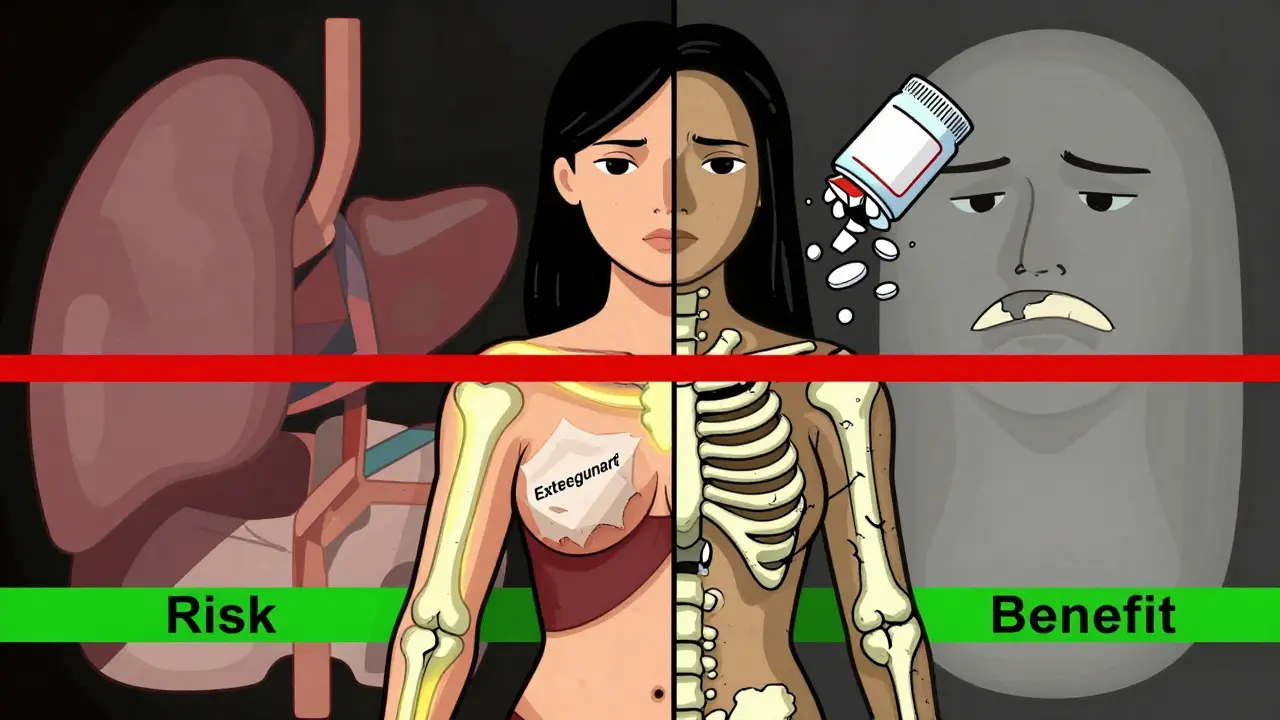
Risks: What You Need to Worry About
Let’s be clear: HRT isn’t risk-free. But the risks aren’t what they used to be.
For women taking estrogen plus progestogen, there’s a small increase in breast cancer risk-about 8 extra cases per 10,000 women per year. That sounds scary, but let’s put it in context. The average woman’s lifetime risk of breast cancer is about 13%. HRT adds less than 1% to that over 5 years. And here’s the twist: transdermal estrogen (patches or gels) doesn’t raise breast cancer risk at all, according to multiple studies. Oral estrogen does. So delivery method matters.
Another concern: blood clots. Oral HRT increases the risk of deep vein thrombosis (DVT) by about 2.5 times. But transdermal HRT? The risk is nearly the same as not taking anything. One study found 3.7 cases per 1,000 women per year with pills versus 1.3 with patches. That’s a 65% drop. If you’re over 40, have a history of clots, or smoke, patches are the only safe choice.
Stroke risk? Slightly higher with oral HRT. Again, transdermal lowers that risk by 30-50%. And if you’ve had breast cancer, endometrial cancer, liver disease, or a past blood clot-HRT is off the table. Always.
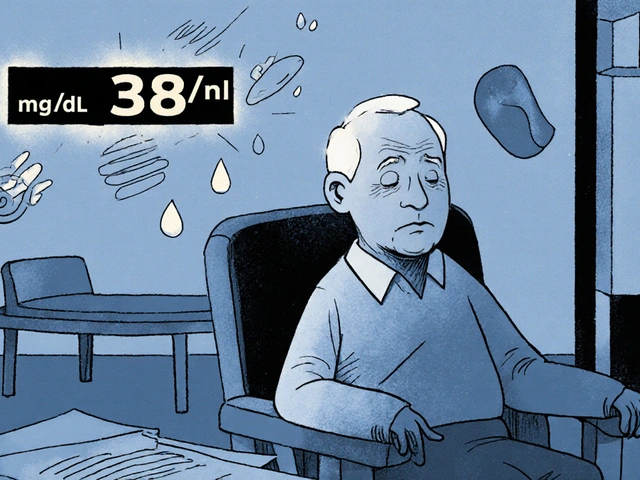
Monitoring: It’s Not a Set-and-Forget Treatment
HRT isn’t something you start and forget. You need to check in. Regularly.
Before you begin, your doctor should do a full check: mammogram, pelvic exam, blood pressure, BMI, and liver tests. No exceptions. Then, at 3 months, you’ll talk about how you’re feeling. Any new bleeding? Mood changes? Breast tenderness? These aren’t side effects to ignore-they’re signals.
After that, annual visits are the standard. Every year: mammogram, blood pressure, weight check, and a conversation. No one should be on HRT for more than 5-7 years unless there’s a strong medical reason. And even then, the dose should be the lowest that works. Some women need it for 10 years. Others stop after 2. It depends on symptoms, health history, and goals.
One thing that catches people off guard: irregular bleeding in the first 6 months. It’s common-happens in 30-50% of users. But if it lasts longer than 6 months, you need an ultrasound or biopsy. Don’t wait. Don’t assume it’s "normal."
Transdermal vs. Oral: The Real Difference
Most women don’t realize their pill isn’t the only option. Patches, gels, sprays, and vaginal rings are all HRT too-and often better.
Oral estrogen goes through your liver first. That’s why it raises clot and stroke risk. Transdermal estrogen goes straight into your bloodstream. No liver overload. Lower risk. Fewer side effects like nausea or bloating. In one Cleveland Clinic survey, 28% of pill users had nausea. Only 12% of gel users did.
And the numbers back it up. Transdermal estrogen cuts blood clot risk in half. Stroke risk drops by 30-50%. Breast cancer risk? Studies show no increase with patches or gels. That’s why experts like Dr. Jessica L. Chan at Cedars-Sinai now recommend transdermal as first-line for most women.
For vaginal symptoms-dryness, pain during sex-low-dose vaginal estrogen (tablets, rings, creams) is the gold standard. It doesn’t affect your whole body. Just your vagina. No systemic risks. Perfect for women who only need local relief.
Bioidentical vs. Synthetic: The Myth vs. The Data
You’ve probably heard about "natural" or "bioidentical" HRT. It sounds safer, right? Not necessarily.
Bioidentical hormones are chemically identical to what your body makes. That’s true. But so are FDA-approved estradiol and progesterone. The difference? Compounded bioidenticals-made in pharmacies-are not regulated. Doses vary. Purity isn’t guaranteed. There’s no proof they’re safer than standard HRT. In fact, the Endocrine Society says there’s no evidence they reduce risks.
Some clinics push compounded hormones as "customized" or "miracle cures." But they’re not. And they can be dangerous. If you’re going bioidentical, stick to FDA-approved versions: estradiol patches, progesterone capsules, or gels. Not the stuff mixed in a backroom lab.
Who Should Avoid HRT?
HRT isn’t for everyone. Absolute no-go zones:
- History of breast cancer
- History of blood clots (DVT, pulmonary embolism)
- History of stroke or heart attack
- Unexplained vaginal bleeding
- Active liver disease
- Known estrogen-sensitive cancer
If you have a strong family history of breast cancer or carry BRCA mutations, talk to a specialist. HRT might still be an option, but it needs careful planning. Don’t rule it out without a full risk assessment.
What Happens When You Stop?
Many women stop HRT because they’re scared. Others stop because they feel fine. But symptoms often come back-and sometimes harder than before.
One study found 35% of women quit HRT within a year. Half of them cited fear of breast cancer. But when they stopped, 70% reported hot flashes returned within weeks. And for some, they were worse.
There’s no evidence that stopping HRT increases cancer risk. But stopping suddenly can trigger bone loss, mood dips, and sleep disruption. If you want to stop, taper slowly. Talk to your doctor. Don’t just quit.
The Big Picture: Is HRT Right for You?
Here’s the truth: if you’re under 60, within 10 years of menopause, and your symptoms are disrupting your life-HRT is likely the best option you have. Not the only one. But the most effective.
It’s not about living longer. It’s about living better. Fewer hot flashes. Better sleep. Stronger bones. Less anxiety. More energy. Those aren’t trivial. They’re the foundation of quality of life.
And the data supports it. The FDA updated its labels in 2022 to say exactly that: for women who start HRT early, benefits outweigh risks. The black box warnings? Gone. The fear? Outdated.
Still, you need to be smart about it. Choose transdermal. Use the lowest dose. Get monitored. Ask questions. Don’t let old myths scare you away from something that could change your daily reality.
Menopause isn’t a disease. But it’s a medical event. And like any medical event, you have choices. HRT is one of them. And for millions of women, it’s the right one.
Is hormone replacement therapy safe for women over 60?
For women over 60 who haven’t taken HRT before, starting it now is generally not recommended. The risks-like blood clots, stroke, and breast cancer-outweigh the benefits at this age. But if you started HRT before 60 and are doing well, continuing it may still be safe under a doctor’s supervision. The key is timing: HRT works best when started early.
Can HRT cause weight gain?
HRT itself doesn’t cause weight gain. But menopause does. As estrogen drops, your body stores more fat around the abdomen. Some women feel bloated on oral HRT due to water retention, but this usually fades. Transdermal HRT is less likely to cause bloating. Weight gain during menopause is more about metabolism, diet, and activity levels than hormones.
How long should I stay on HRT?
There’s no fixed time limit. Most women take HRT for 3-7 years to manage symptoms. But if you still have severe hot flashes, night sweats, or bone loss after 7 years, continuing may be appropriate. The goal is the lowest dose for the shortest time needed. Regular check-ups help decide when to taper off. Never stop abruptly.
Do I need progesterone if I’ve had a hysterectomy?
No. If you’ve had a hysterectomy (removal of the uterus), you only need estrogen. Progesterone is only required to protect the uterine lining. Without a uterus, there’s no lining to protect. Taking progesterone unnecessarily can increase side effects like mood swings or breast tenderness without benefit.
Are there alternatives to HRT for hot flashes?
Yes-but they’re less effective. SSRIs like paroxetine can reduce hot flashes by 50-60%. Gabapentin and clonidine help some women. Lifestyle changes-cooling techniques, avoiding triggers, exercise-also help. But none match HRT’s 80-90% reduction rate. If your symptoms are mild, alternatives are fine. If they’re severe, HRT remains the gold standard.
Can I use HRT if I have a family history of breast cancer?
It’s complicated. A family history alone doesn’t rule out HRT, but it requires careful review. If you carry BRCA1/2 mutations, most experts advise against estrogen-only HRT. Transdermal estrogen without progesterone may be an option in some cases, but only after genetic counseling and a full risk-benefit discussion. Never assume HRT is unsafe without expert input.
What’s the best way to start HRT?
Start low and go slow. For most women, the best first step is a low-dose transdermal estradiol patch (0.025-0.0375 mg/day) or gel (1.5 mg/day). If you have a uterus, add micronized progesterone (100-200 mg at night, days 1-12 of each month). Avoid oral pills unless you have a specific reason. Always begin with a full medical checkup and discuss your goals and concerns with your doctor.





Ryan Hutchison
January 16, 2026 AT 12:12HRT is just another way big pharma keeps women dependent on pills. We used to manage menopause with diet, exercise, and sleep-now we’re told to inject hormones like we’re lab rats. The WHI study wasn’t wrong, it was misinterpreted. They gave old women synthetic crap and called it science. Transdermal? Still a drug. Still risky. Stop buying into the medical-industrial complex.
Samyak Shertok
January 17, 2026 AT 14:56Oh wow, so now estrogen is the new yoga? You’re telling me the cure for aging is… more hormones? Brilliant. Next you’ll say we should inject dopamine to stop existential dread. Let me guess-your doctor also sells you collagen powder and CBD gummies? At this point, menopause is just capitalism’s way of monetizing biological inevitability. 🤡
Henry Ip
January 19, 2026 AT 11:06I’ve been on low-dose estradiol gel for 4 years now. Hot flashes? Gone. Sleep? Better. Mood? Stable. I started at 52, had a hysterectomy, no uterus, no progesterone needed. My doctor checked my liver, BP, and did a baseline mammogram. No drama. No panic. Just science. If you’re under 60 and suffering, don’t let fear stop you. Talk to a menopause specialist, not your general practitioner. They know the difference.
waneta rozwan
January 19, 2026 AT 12:51Let’s be real-most women on HRT are just scared of getting old. You think estrogen will keep you ‘glowing’? It won’t. It just delays the inevitable. And what about the women who took it for 15 years and ended up with stage 3 breast cancer? You think they were warned? No. They were sold a dream. And now they’re paying the price. Don’t be another statistic. Embrace natural aging. It’s not a disease.
Nicholas Gabriel
January 20, 2026 AT 02:07Hey, I just want to say-this post is SO important. I’ve seen so many women quit HRT because they’re terrified of breast cancer, and then they end up in the ER with a broken hip because their bones turned to dust. I work with older women every day. The ones who stayed on low-dose transdermal? They’re walking, gardening, traveling. The ones who stopped? They’re in wheelchairs. Please don’t let fear make your choices for you. Talk to your doctor. Get tested. Be informed. You’ve got this.
Cheryl Griffith
January 21, 2026 AT 14:53I started HRT at 54 after two years of sleepless nights and crying over spilled coffee. It didn’t fix everything-but it gave me back my mornings. I use a patch. No bloating. No nausea. My doc said 5 years max, but I’m on year 6 and we’re monitoring. I don’t feel guilty. I feel like I got my life back. If you’re debating it, just ask yourself: would I rather live with the symptoms or try something that works? I chose the latter.
swarnima singh
January 21, 2026 AT 20:20hrt is just a tool for the patriarchy to keep women docile and productive… they dont want us to slow down or rest… they want us to keep working, keep smiling, keep looking young… the real issue is society doesnt value older women… not the hormones… the hormones are just the bandaid…
Isabella Reid
January 23, 2026 AT 06:47As someone who’s been through this, I get the fear. But I also get the relief. I tried everything-yoga, acupuncture, black cohosh, even cold showers at 3 a.m. Nothing worked like the patch. I’m not saying it’s perfect. But it’s the best tool we’ve got. And if you’re in your 50s and exhausted, don’t let someone on the internet tell you you’re weak for wanting to feel better. You’re not broken. You’re just human.
Jody Fahrenkrug
January 24, 2026 AT 19:49My mom’s on HRT. She’s 61. Started at 56. No cancer history. Just brutal hot flashes. Patch. Low dose. Annual checkups. She says it’s the best thing she’s done for herself since quitting smoking. I used to be scared too. Now I’m just grateful she’s sleeping and not yelling at the TV every night.
Kasey Summerer
January 25, 2026 AT 11:42Transdermal HRT = real life upgrade 🤘 I switched from pills to gel after 3 months of nausea and bloating. Within 2 weeks? I could actually taste my coffee again. Who knew hormones could make you feel like a person and not a walking side effect?
kanchan tiwari
January 26, 2026 AT 19:48they're hiding the truth. HRT is linked to the glyphosate epidemic. The estrogen mimics the chemicals in your food. The patches? They're laced with nano-plastics from the packaging. The FDA is in bed with big pharma. Your doctor doesn't know what's really in that gel. You're being experimented on. Wake up.
Bobbi-Marie Nova
January 27, 2026 AT 02:31Same. I was skeptical too. Thought it was just another way to make women feel broken. But after my third night of waking up drenched and sobbing? I tried the patch. Didn’t magically fix my life-but it gave me back the energy to try. And honestly? That’s enough. Don’t let anyone make you feel guilty for wanting to feel okay.
john Mccoskey
January 27, 2026 AT 12:49Let’s deconstruct this. The article cherry-picks data from the WHI reanalysis and ignores the 2019 Cochrane meta-analysis that showed no mortality benefit for HRT in women over 60. It promotes transdermal estrogen as safer-true-but fails to mention that even transdermal estrogen increases IGF-1 levels, which are associated with tumor proliferation. It ignores the fact that estrogen receptor-alpha signaling in breast tissue is dose-dependent and cumulative. It also omits that the 32% cardiovascular benefit only applies to women who start within 5 years of menopause, not 10, as the article misleadingly claims. And yet, the narrative is presented as definitive, when in reality, the evidence is nuanced, context-dependent, and still evolving. This isn’t empowerment-it’s pharmaceutical propaganda dressed in scientific language. You’re not being informed. You’re being marketed to.